- 著者
- Makoto Takeyama Sen Yachi Yuji Nishimoto Ichizo Tsujino Junichi Nakamura Naoto Yamamoto Hiroko Nakata Satoshi Ikeda Michihisa Umetsu Shizu Aikawa Hiroya Hayashi Hirono Satokawa Yoshinori Okuno Eriko Iwata Yoshito Ogihara Nobutaka Ikeda Akane Kondo Takehisa Iwai Norikazu Yamada Tomohiro Ogawa Takao Kobayashi Makoto Mo Yugo Yamashita
- 出版者
- Japan Epidemiological Association
- 雑誌
- Journal of Epidemiology (ISSN:09175040)
- 巻号頁・発行日
- pp.JE20220201, (Released:2022-11-12)
- 参考文献数
- 53
- 被引用文献数
- 2 1
Background: Reports of mortality-associated risk factors in patients with the novel coronavirus disease 2019 (COVID-19) are limited.Methods: We evaluated the clinical features that were associated with mortality among patients who died during hospitalization (n = 158) and those who were alive at discharge (n = 2,736) from the large-scale, multicenter, retrospective, observational cohort CLOT-COVID study, which enrolled consecutively hospitalized COVID-19 patients from 16 centers in Japan from April to September 2021. Data from 2,894 hospitalized COVID-19 participants of the CLOT-COVID study were analyzed in this study.Results: Patients who died were older (71.1 years vs 51.6 years, P < 0.001), had higher median D-dimer values on admission (1.7 µg/mL vs 0.8 µg/mL, P < 0.001), and had more comorbidities. On admission, the patients who died had more severe COVID-19 than did those who survived (mild: 16% vs 63%, moderate: 47% vs 31%, and severe: 37% vs 6.2%, P < 0.001). In patients who died, the incidence of thrombosis and major bleeding during hospitalization was significantly higher than that in those who survived (thrombosis: 8.2% vs 1.5%, P < 0.001; major bleeding: 12.7% vs 1.4%, P < 0.001). Multivariable logistic regression analysis revealed that age >70 years, high D-dimer values on admission, heart disease, active cancer, higher COVID-19 severity on admission, and development of major bleeding during hospitalization were independently associated with a higher mortality risk.Conclusion: This large-scale observational study in Japan identified several independent risk factors for mortality in hospitalized patients with COVID-19 that could facilitate appropriate risk stratification of patients with COVID-19.
- 著者
- Ko Yamamoto Hiroki Shiomi Takeshi Morimoto Hiroki Watanabe Akiyoshi Miyazawa Kyohei Yamaji Masanobu Ohya Sunao Nakamura Satoru Mitomo Satoru Suwa Takenori Domei Shojiro Tatsushima Koh Ono Hiroki Sakamoto Kiyotaka Shimamura Masataka Shigetoshi Ryoji Taniguchi Yuji Nishimoto Hideki Okayama Kensho Matsuda Kenji Nakatsuma Yohei Takayama Jun Kuribara Hidekuni Kirigaya Kohei Yoneda Yuta Imai Umihiko Kaneko Hiroshi Ueda Kota Komiyama Naotaka Okamoto Satoru Sasaki Kengo Tanabe Mitsuru Abe Kiyoshi Hibi Kazushige Kadota Kenji Ando Takeshi Kimura on behalf of the OPTIVUS-Complex PCI Investigators
- 出版者
- The Japanese Circulation Society
- 雑誌
- Circulation Journal (ISSN:13469843)
- 巻号頁・発行日
- pp.CJ-22-0837, (Released:2023-03-11)
- 参考文献数
- 11
- 被引用文献数
- 5
Background: There is a paucity of data on the effect of optimal intravascular ultrasound (IVUS)-guided percutaneous coronary intervention (PCI) compared with standard PCI or coronary artery bypass grafting (CABG) in patients with multivessel disease.Methods and Results: The OPTIVUS-Complex PCI study multivessel cohort was a prospective multicenter single-arm study enrolling 1,021 patients undergoing multivessel PCI including the left anterior descending coronary artery using IVUS aiming to meet the prespecified criteria for optimal stent expansion. We conducted propensity score matching analyses between the OPTIVUS group and historical PCI or CABG control groups from the CREDO-Kyoto registry cohort-3 (1,565 and 899 patients) fulfilling the inclusion criteria for this study. The primary endpoint was a composite of death, myocardial infarction, stroke, or any coronary revascularization. In the propensity score-matched cohort (OPTIVUS vs. historical PCI control: 926 patients in each group; OPTIVUS vs. historical CABG control: 436 patients in each group), the cumulative 1-year incidence of the primary endpoint was significantly lower in the OPTIVUS group than in the historical PCI control group (10.4% vs. 23.3%; log-rank P<0.001) or the historical CABG control group (11.8% vs. 16.5%; log-rank P=0.02).Conclusions: IVUS-guided PCI targeting the OPTIVUS criteria combined with contemporary clinical practice was associated with superior clinical outcomes at 1 year compared with not only the historical PCI control, but also the historical CABG control.
6 0 0 0 OA Cancer-Associated Venous Thromboembolism in the Real World ― From the COMMAND VTE Registry ―
- 著者
- Jiro Sakamoto Yugo Yamashita Takeshi Morimoto Hidewo Amano Toru Takase Seiichi Hiramori Kitae Kim Maki Oi Masaharu Akao Yohei Kobayashi Mamoru Toyofuku Toshiaki Izumi Tomohisa Tada Po-Min Chen Koichiro Murata Yoshiaki Tsuyuki Syunsuke Saga Yuji Nishimoto Tomoki Sasa Minako Kinoshita Kiyonori Togi Hiroshi Mabuchi Kensuke Takabayashi Yusuke Yoshikawa Hiroki Shiomi Takao Kato Takeru Makiyama Koh Ono Toshihiro Tamura Yoshihisa Nakagawa Takeshi Kimura on behalf of the COMMAND VTE Registry Investigators
- 出版者
- The Japanese Circulation Society
- 雑誌
- Circulation Journal (ISSN:13469843)
- 巻号頁・発行日
- pp.CJ-19-0515, (Released:2019-09-20)
- 参考文献数
- 28
- 被引用文献数
- 5 57
Background:There is a paucity of data on the management and prognosis of cancer-associated venous thromboembolism (VTE), leading to uncertainty about optimal management strategies.Methods and Results:The COMMAND VTE Registry is a multicenter registry enrolling 3,027 consecutive acute symptomatic VTE patients in Japan between 2010 and 2014. We divided the entire cohort into 3 groups: active cancer (n=695, 23%), history of cancer (n=243, 8%), and no history of cancer (n=2089, 69%). The rate of anticoagulation discontinuation was higher in patients with active cancer (43.5%, 27.0%, and 27.0%, respectively, at 1 year, P<0.001). The cumulative 5-year incidences of recurrent VTE, major bleeding, and all-cause death were higher in patients with active cancer (recurrent VTE: 17.7%, 10.2%, and 8.6%, P<0.001; major bleeding: 26.6%, 8.8%, and 9.3%, P<0.001; all-cause death: 73.1%, 28.6%, 14.6%, P<0.001). Among the 4 groups classified according to active cancer status, the cumulative 1-year incidence of recurrent VTE was higher in the metastasis group (terminal stage group: 6.4%, metastasis group: 22.1%, under chemotherapy group: 10.8%, and other group: 5.8%, P<0.001).Conclusions:In a current real-world VTE registry, patients with active cancer had higher risk for VTE recurrence, bleeding, and death, with variations according to cancer status, than patients without active cancer. Anticoagulation therapy was frequently discontinued prematurely in patients with active cancer in discordance with current guideline recommendations.
4 0 0 0 OA Developing Multidisciplinary Management of Heart Failure in the Super-Aging Society of Japan
- 著者
- Yukihito Sato Takashi Kuragaichi Hiroyuki Nakayama Kozo Hotta Yuji Nishimoto Takao Kato Ryoji Taniguchi Koichi Washida
- 出版者
- The Japanese Circulation Society
- 雑誌
- Circulation Journal (ISSN:13469843)
- 巻号頁・発行日
- pp.CJ-22-0675, (Released:2022-12-23)
- 参考文献数
- 81
- 被引用文献数
- 3
The Japanese population is rapidly aging because of its long life expectancy and low birth rate; additionally, the number of patients with heart failure (HF) is increasing to the extent that HF is now considered a pandemic. According to a recent HF registry study, Japanese patients with HF have both medical and care-related problems. Although hospitalization is used to provide medical services, and institutionalization is used to provide care for frail older adults, it can be difficult to distinguish between them. In this context, multidisciplinary management of HF has become increasingly important in preventing hospital readmissions and maintaining a patient’s quality of life. Academia has promoted an increase in the number of certified HF nurses and educators. Researchers have issued numerous guidelines or statements on topics such as cardiac rehabilitation, nutrition, and palliative care, in addition to the diagnosis and treatment of acute and chronic HF. Moreover, the Japanese government has created incentives through various medical and long-term care systems adjustments to increase collaboration between these two fields. This review summarizes current epidemiological registries that focus not only on medical but also care-related problems and the 10 years of multidisciplinary management experience in Japanese medical and long-term care systems.
- 著者
- Yuji Nishimoto Ryosuke Hara Ryoji Taniguchi Masanao Toma Yukihito Sato
- 出版者
- The Japanese Circulation Society
- 雑誌
- Circulation Reports (ISSN:24340790)
- 巻号頁・発行日
- vol.3, no.12, pp.742-743, 2021-12-10 (Released:2021-12-10)
- 参考文献数
- 1
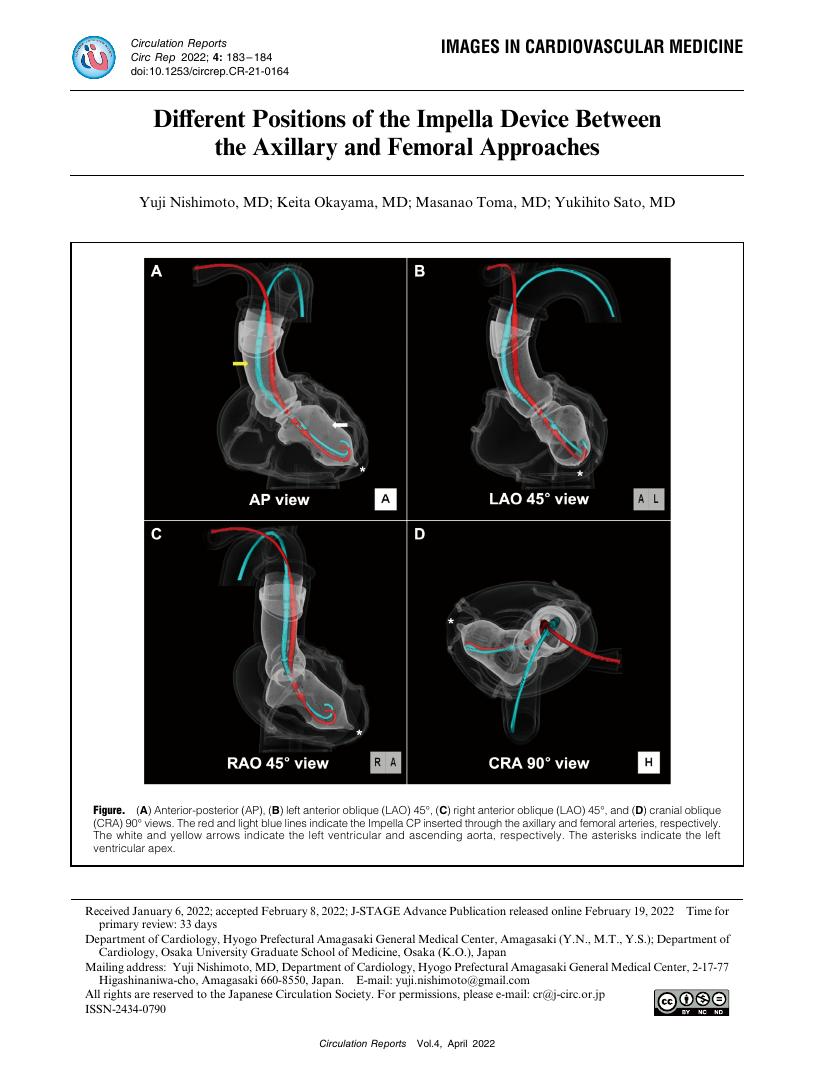
- 著者
- Yuji Nishimoto Keita Okayama Masanao Toma Yukihito Sato
- 出版者
- The Japanese Circulation Society
- 雑誌
- Circulation Reports (ISSN:24340790)
- 巻号頁・発行日
- vol.4, no.4, pp.183-184, 2022-04-08 (Released:2022-04-08)
- 参考文献数
- 1
- 被引用文献数
- 1
- 著者
- Yugo Yamashita Yuuki Maruyama Hirono Satokawa Yuji Nishimoto Ichizo Tsujino Hideki Sakashita Hiroko Nakata Yoshinori Okuno Yoshito Ogihara Sen Yachi Naoki Toya Masami Shingaki Satoshi Ikeda Naoto Yamamoto Shizu Aikawa Nobutaka Ikeda Hiroya Hayashi Shingo Ishiguro Eriko Iwata Michihisa Umetsu Akane Kondo Takehisa Iwai Takao Kobayashi Makoto Mo Norikazu Yamada on behalf of the Taskforce of VTE and COVID-19 in Japan Study
- 出版者
- The Japanese Circulation Society
- 雑誌
- Circulation Journal (ISSN:13469843)
- 巻号頁・発行日
- pp.CJ-21-0169, (Released:2021-05-20)
- 参考文献数
- 33
- 被引用文献数
- 30
Background:Coronavirus disease 2019 (COVID-19) reportedly causes venous thromboembolism (VTE), but the status of this complication in Japan was unclear.Methods and Results:The VTE and COVID-19 in Japan Study is a retrospective, multicenter cohort study enrolling hospitalized patients with COVID-19 who were evaluated with contrast-enhanced computed tomography (CT) examination at 22 centers in Japan between March 2020 and October 2020. Among 1,236 patients with COVID-19, 45 (3.6%) were evaluated with contrast-enhanced CT examination. VTE events occurred in 10 patients (22.2%), and the incidence of VTE in mild, moderate, and severe COVID-19 was 0%, 11.8%, and 40.0%, respectively. COVID-19 patients with VTE showed a higher body weight (81.6 vs. 64.0 kg, P=0.005) and body mass index (26.9 vs. 23.2 kg/m2, P=0.04), and a higher proportion had a severe status for COVID-19 compared with those without. There was no significant difference in the proportion of patients alive at discharge between patients with and without VTE (80.0% vs. 88.6%, P=0.48). Among 8 pulmonary embolism (PE) patients, all were low-risk PE.Conclusions:Among a relatively small number of patients undergoing contrast-enhanced CT examination in Japanese real-world clinical practice, there were no VTE patients among those with mild COVID-19, but the incidence of VTE seemed to be relatively high among severe COVID-19 patients, although all PE events were low-risk without significant effect on mortality risk.
- 著者
- Yuji Nishimoto Yugo Yamashita Kitae Kim Takeshi Morimoto Syunsuke Saga Hidewo Amano Toru Takase Seiichi Hiramori Maki Oi Masaharu Akao Yohei Kobayashi Mamoru Toyofuku Toshiaki Izumi Tomohisa Tada Po-Min Chen Koichiro Murata Yoshiaki Tsuyuki Tomoki Sasa Jiro Sakamoto Minako Kinoshita Kiyonori Togi Hiroshi Mabuchi Kensuke Takabayashi Yusuke Yoshikawa Hiroki Shiomi Takao Kato Takeru Makiyama Koh Ono Yukihito Sato Takeshi Kimura on behalf of the COMMAND VTE Registry Investigators
- 出版者
- The Japanese Circulation Society
- 雑誌
- Circulation Journal (ISSN:13469843)
- 巻号頁・発行日
- vol.84, no.11, pp.2006-2014, 2020-10-23 (Released:2020-10-23)
- 参考文献数
- 33
- 被引用文献数
- 19
Background:Patients with cancer-associated venous thromboembolism (VTE) are at high risk for recurrent VTE and are recommended to receive prolonged anticoagulation therapy if they are at a low risk for bleeding. However, there are no established risk factors for bleeding during anticoagulation therapy.Methods and Results:The COMMAND VTE Registry is a multicenter retrospective registry enrolling 3,027 consecutive patients with acute symptomatic VTE among 29 Japanese centers. The present study population consisted of 592 cancer-associated VTE patients with anticoagulation therapy. We constructed a multivariable Cox proportional hazard model to estimate the hazard ratio (HR) and 95% confidence interval (CI) of the potential risk factors for major bleeding. During a median follow-up period of 199 days, major bleeding occurred in 72 patients. The cumulative incidence of major bleeding was 5.8% at 3 months, 13.8% at 1 year, 17.5% at 2 years, and 28.1% at 5 years. The most frequent major bleeding site was gastrointestinal tract (47%). Terminal cancer (adjusted HR, 4.17; 95% CI, 2.22–7.85, P<0.001), chronic kidney disease (adjusted HR, 1.89; 95% CI 1.06–3.37, P=0.031), and gastrointestinal cancer (adjusted HR, 1.78; 95% CI, 1.04–3.04, P=0.037) were independently associated with an increased risk of major bleeding.Conclusions:Major bleeding events were common during anticoagulation therapy in real-world cancer-associated VTE patients. Terminal cancer, chronic kidney disease, and gastrointestinal cancer were the independent risk factors for major bleeding.
- 著者
- Makoto Takeyama Sen Yachi Yuji Nishimoto Ichizo Tsujino Junichi Nakamura Naoto Yamamoto Hiroko Nakata Satoshi Ikeda Michihisa Umetsu Shizu Aikawa Hiroya Hayashi Hirono Satokawa Yoshinori Okuno Eriko Iwata Yoshito Ogihara Nobutaka Ikeda Akane Kondo Takehisa Iwai Norikazu Yamada Tomohiro Ogawa Takao Kobayashi Makoto Mo Yugo Yamashita
- 出版者
- Japan Epidemiological Association
- 雑誌
- Journal of Epidemiology (ISSN:09175040)
- 巻号頁・発行日
- vol.33, no.3, pp.150-157, 2023-03-05 (Released:2023-03-05)
- 参考文献数
- 53
- 被引用文献数
- 1
Background: Reports of mortality-associated risk factors in patients with the novel coronavirus disease 2019 (COVID-19) are limited.Methods: We evaluated the clinical features that were associated with mortality among patients who died during hospitalization (n = 158) and those who were alive at discharge (n = 2,736) from the large-scale, multicenter, retrospective, observational cohort CLOT-COVID study, which enrolled consecutively hospitalized COVID-19 patients from 16 centers in Japan from April to September 2021. Data from 2,894 hospitalized COVID-19 participants of the CLOT-COVID study were analyzed in this study.Results: Patients who died were older (71.1 years vs 51.6 years, P < 0.001), had higher median D-dimer values on admission (1.7 µg/mL vs 0.8 µg/mL, P < 0.001), and had more comorbidities. On admission, the patients who died had more severe COVID-19 than did those who survived (mild: 16% vs 63%, moderate: 47% vs 31%, and severe: 37% vs 6.2%, P < 0.001). In patients who died, the incidence of thrombosis and major bleeding during hospitalization was significantly higher than that in those who survived (thrombosis: 8.2% vs 1.5%, P < 0.001; major bleeding: 12.7% vs 1.4%, P < 0.001). Multivariable logistic regression analysis revealed that age >70 years, high D-dimer values on admission, heart disease, active cancer, higher COVID-19 severity on admission, and development of major bleeding during hospitalization were independently associated with a higher mortality risk.Conclusion: This large-scale observational study in Japan identified several independent risk factors for mortality in hospitalized patients with COVID-19 that could facilitate appropriate risk stratification of patients with COVID-19.