3 0 0 0 OA Surgical Treatment of Rectal Prolapse in the Laparoscopic Era; A Review of the Literature
- 著者
- Akira Tsunoda
- 出版者
- The Japan Society of Coloproctology
- 雑誌
- Journal of the Anus, Rectum and Colon (ISSN:24323853)
- 巻号頁・発行日
- vol.4, no.3, pp.89-99, 2020-07-30 (Released:2020-07-30)
- 参考文献数
- 98
- 被引用文献数
- 25
Rectal prolapse is associated with debilitating symptoms including the discomfort of prolapsing tissue, mucus discharge, hemorrhage, and defecation disorders of fecal incontinence, constipation, or both. The aim of treatment is to eliminate the prolapse, correct associated bowel function and prevent new onset of bowel dysfunction. Historically, abdominal procedures have been indicated for young fit patients, whereas perineal approaches have been preferred in older frail patients with significant comorbidity. Recently, the laparoscopic procedures with their advantages of less pain, early recovery, and lower morbidity have emerged as an effective tool for the treatment of rectal prolapse. This article aimed to review the current evidence base for laparoscopic procedures and perineal procedures, and to compare the results of various techniques. As a result, laparoscopic procedures showed a relatively low recurrence rate than the perineal procedures with comparable complication rates. Laparoscopic resection rectopexy and laparoscopic ventral mesh rectopexy had a small advantage in the improvement of constipation or the prevention of new-onset constipation compared with other laparoscopic procedures. However, the optimal surgical repair has not been clearly demonstrated because of the significant heterogeneity of available studies. An individualized approach is recommended for every patient, considering age, comorbidity, and the underlying anatomical and functional disorders.
- 著者
- Akira Tsunoda
- 出版者
- The Japan Society of Coloproctology
- 雑誌
- Journal of the Anus, Rectum and Colon (ISSN:24323853)
- 巻号頁・発行日
- vol.5, no.4, pp.335-339, 2021-10-28 (Released:2021-10-28)
- 参考文献数
- 25
- 被引用文献数
- 3
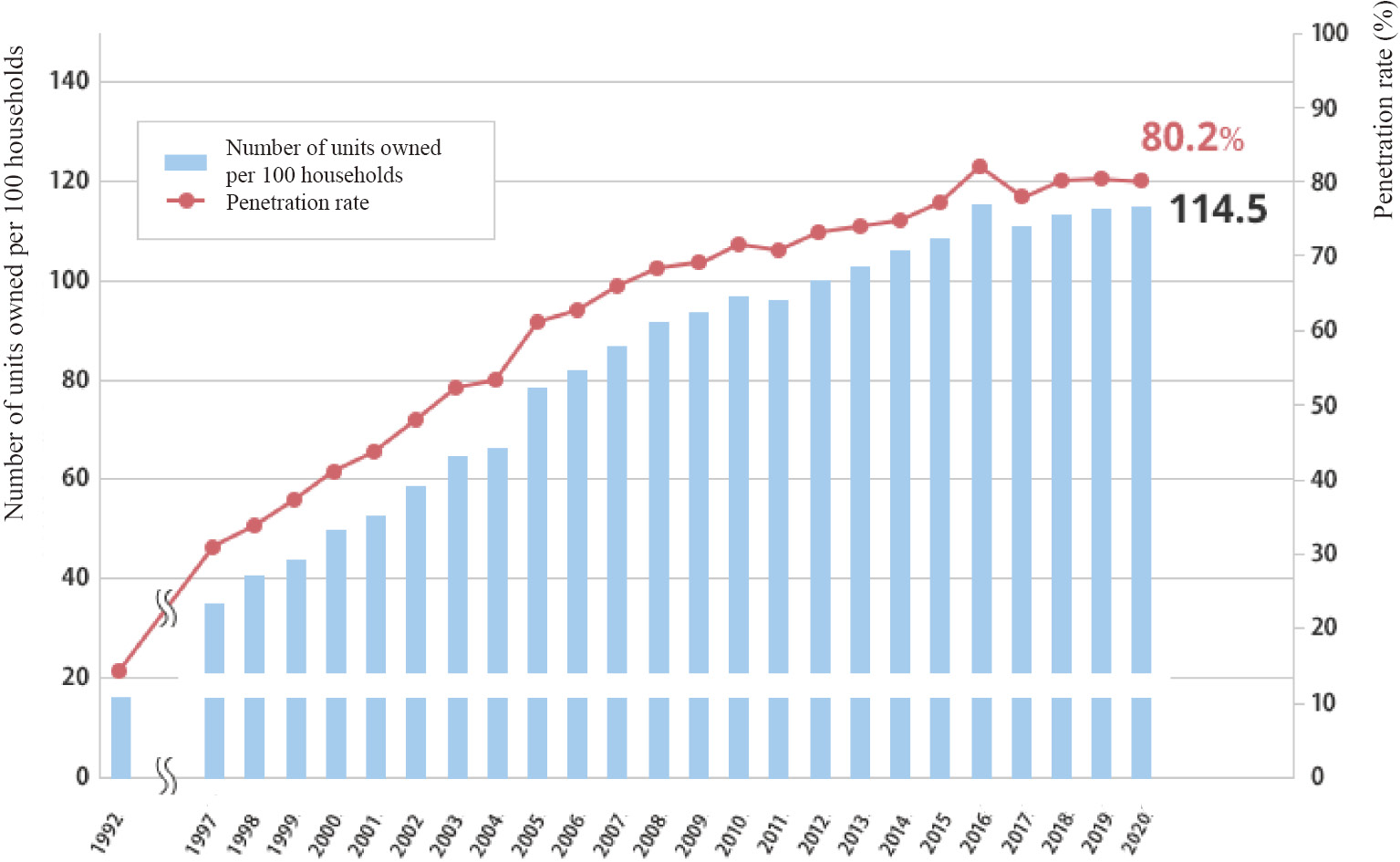
Electric bidet toilets are widely used in Japan and are sanitary devices, that are integral to daily life. Approximately, half of the population washed the anus before or after defecation. Cleaning the anus after defecation using the bidets contributes to hand hygiene and local comfort, and it may be effective against constipation. However, excessive bidet use potentially causes anal pruritus and anal incontinence (AI). Physicians are advised to instruct patients with anal pruritus to avoid excessive cleaning of the anus and those with AI to discontinue bidet use. For the estimation of the inherent severity of AI, physicians should instruct a bidet user with AI to discontinue bidet use and assess the severity of AI later. Additionally, the nozzle surface and splay water of bidet toilets may be contaminated with fecal indicator bacteria, such as Escherichia coli and Pseudomonas aeruginosa, as well as antimicrobial-resistant bacteria, rendering them a potential vehicle for cross-infection. In the hospital setting, compromised patients must be cautious regarding the shared use of bidet toilets to prevent infection by antimicrobial-resistant bacteria. Specifically, they should be provided with bidet toilets exclusive for them or may need to be instructed to not use a bidet.