- 著者
- Hiroshi KARIBE Ayumi NARISAWA Arata NAGAI Satoshi YAMANOUCHI Motonobu KAMEYAMA Atsuhiro NAKAGAWA Teiji TOMINAGA
- 出版者
- The Japan Neurosurgical Society
- 雑誌
- Neurologia medico-chirurgica (ISSN:04708105)
- 巻号頁・発行日
- pp.2022-0327, (Released:2023-01-20)
- 参考文献数
- 34
- 被引用文献数
- 3
Anti-thrombotic drugs may increase the risk for chronic subdural hematoma (CSDH). However, whether to continue or discontinue/counteract these drugs has not been investigated in patients with mild head trauma. CSDH incidence after mild head trauma, as well as the risk for CSDH in patients with anti-thrombotic drugs, were investigated in this study. The study included 765 consecutive elderly (>65 y.o.) patients with mild head trauma and an initial Glasgow Coma Scale (GCS) score of 14 or 15. All patients received initial CT within 24 hours after trauma and were re-examined 30 days after trauma to detect CSDH formation, repeating for every 30 days to examine symptomatic CSDH progression. Patients were divided into two groups, with anti-thrombotic drugs (n = 195) or without them (n = 263), to investigate the influence of pre-traumatic conditioning with anti-thrombotic drugs on CSDH. The whole sample was 458 out of 765 cases. The incidence of CSDH formation was 91 out of 458 cases (19.9%) after mild head trauma, with no significant difference between with and without anti-thrombotic drugs. CSDH progressed as symptomatic in 21 out of 458 cases (4.6%), with no significant difference between with and without anti-thrombotic drugs. Pre-traumatic conditioning with anti-thrombotic drugs and its continuation after trauma did not affect the incidence of formation or symptomatic progression of CSDH. This finding suggests that discontinuing and/or counteracting anti-thrombotic drugs may be unnecessary in patients with mild head trauma.
- 著者
- Arata NAGAI Yasuhiro SUZUKI Tomohisa ISHIDA Yoshimichi SATO Tomoo INOUE Teiji TOMINAGA
- 出版者
- The Japan Neurosurgical Society
- 雑誌
- Neurologia medico-chirurgica (ISSN:04708105)
- 巻号頁・発行日
- pp.2022-0155, (Released:2022-10-13)
- 参考文献数
- 31
- 被引用文献数
- 1
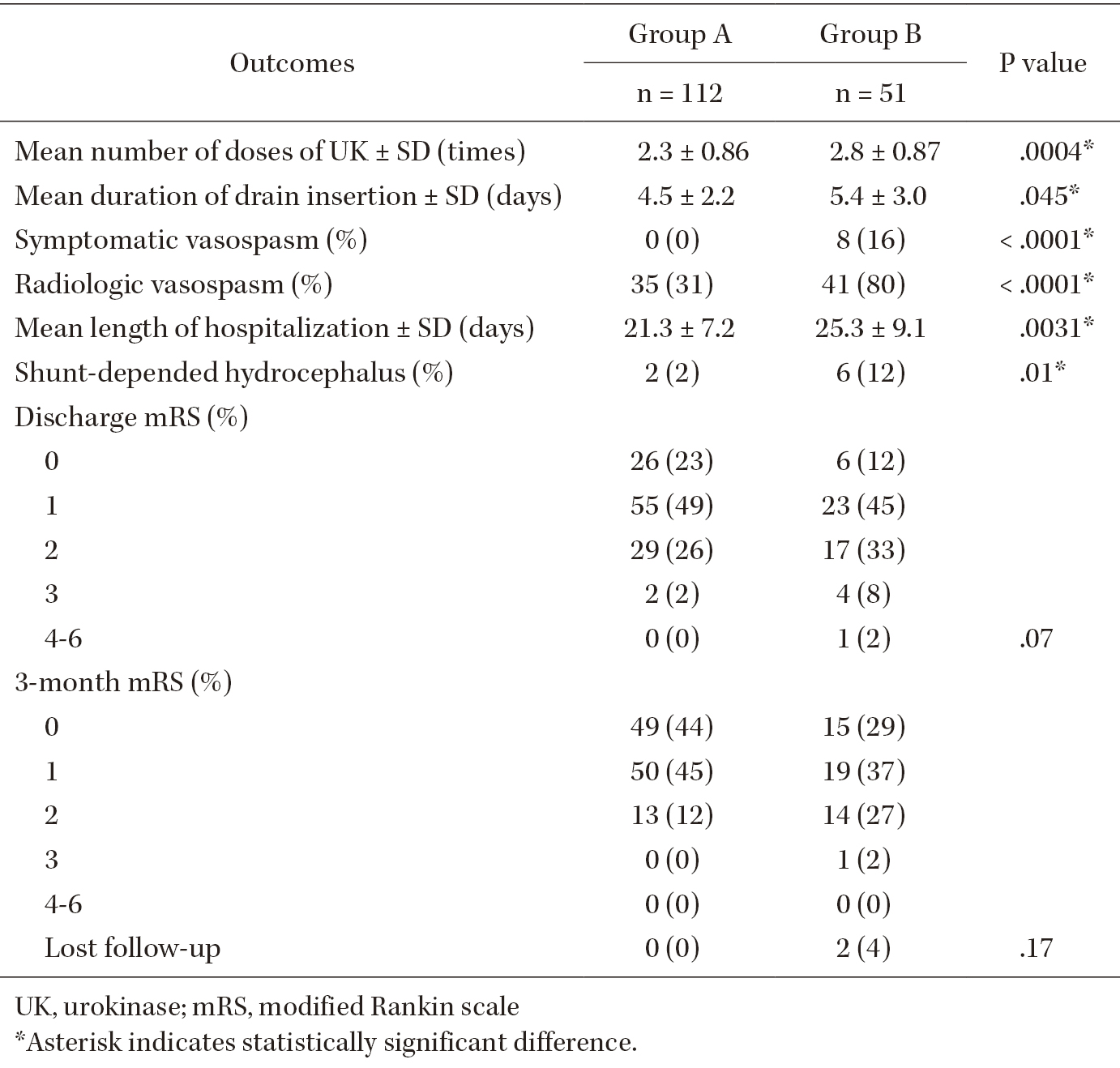
Delayed cerebral vasospasms after subarachnoid hemorrhage (SAH) are a risk factor for poor prognosis after successful treatment of ruptured intracranial aneurysms. Different strategies to remove clots from the subarachnoid space and prevent vasospasms have different outcomes. Intrathecal urokinase infusion therapy combined with endovascular treatment (EVT) can reduce the incidence of symptomatic vasospasms. To analyze the relationship between symptomatic vasospasms and residual SAHs after urokinase infusion therapy, we retrospectively reviewed the records of 348 consecutive patients managed with EVT and intrathecal urokinase infusion therapy for aneurysmal SAH at our institution between 2010 and 2021. Among them, 163 patients met the study criteria and were classified into two groups according to the presence of residual SAH in the cisterns, Sylvian fissures, and frontal interhemispheric fissure. The incidence of symptomatic vasospasms and the clinical outcomes were assessed. In total, eight (5.0%) patients developed symptomatic vasospasms. Patients with symptomatic vasospasms had a significantly higher incidence of residual SAH in the Sylvian or frontal interhemispheric fissures than those without (P <.0001). No patient with SAHs resolved by urokinase infusion therapy developed symptomatic vasospasms. However, the two groups did not differ significantly in terms of modified Rankin scale scores at discharge. Treatment with intrathecal urokinase infusion after EVT for aneurysmal SAH can substantially reduce the risk of clinically evident vasospasms.
1 0 0 0 OA Neurolymphomatosis in a cat
- 著者
- Masashi SAKURAI Kazushi AZUMA Arata NAGAI Toru FUJIOKA Yuji SUNDEN Akinori SHIMADA Takehito MORITA
- 出版者
- 公益社団法人 日本獣医学会
- 雑誌
- Journal of Veterinary Medical Science (ISSN:09167250)
- 巻号頁・発行日
- pp.15-0553, (Released:2016-03-09)
- 被引用文献数
- 6
A 9-year-old male mixed breed cat showed chronic progressive neurological symptoms, which are represented by ataxia and seizures. At necropsy, spinal roots and spinal ganglions at the level of sixth cervical nerve to second thoracic nerve were bilaterally swollen and replaced by white mass lesions. Right brachial plexus and cranial nerves (III, V and VII) were also swollen. A mass lesion was found in the right frontal lobe of the cerebrum. Histologically, neoplastic lymphocytes extensively involved the peripheral nerves, and they infiltrated into the cerebral and spinal parenchyma according to the peripheral nerve tract. Immunohistochemically, most neoplastic lymphocytes were positive for CD20. The clinical and histological features in this case resemble those of neurolymphomatosis in humans.