- 著者
- Hideo Ohuchi Masaaki Kawata Hideki Uemura Teiji Akagi Atsushi Yao Hideaki Senzaki Shingo Kasahara Hajime Ichikawa Hirohiko Motoki Morio Syoda Hisashi Sugiyama Hiroyuki Tsutsui Kei Inai Takaaki Suzuki Kisaburo Sakamoto Syunsuke Tatebe Tomoko Ishizu Yumi Shiina Shigeru Tateno Aya Miyazaki Norihisa Toh Ichiro Sakamoto Chisato Izumi Yoshiko Mizuno Atsuko Kato Koichi Sagawa Ryota Ochiai Fukiko Ichida Takeshi Kimura Hikaru Matsuda Koichiro Niwa on behalf of the Japanese Circulation Society Joint Working Group
- 出版者
- The Japanese Circulation Society
- 雑誌
- Circulation Journal (ISSN:13469843)
- 巻号頁・発行日
- pp.CJ-22-0134, (Released:2022-08-31)
- 参考文献数
- 1071
- 被引用文献数
- 6
- 著者
- Masafumi Kanai Masatoshi Minamisawa Hirohiko Motoki Yuta Seko Kazuhiro Kimura Takahiro Okano Yasushi Ueki Koji Yoshie Tamon Kato Tatsuya Saigusa Soichiro Ebisawa Ayako Okada Neiko Ozasa Takao Kato Koichiro Kuwahara
- 出版者
- The Japanese Circulation Society
- 雑誌
- Circulation Journal (ISSN:13469843)
- 巻号頁・発行日
- pp.CJ-22-0712, (Released:2023-08-04)
- 参考文献数
- 28
- 被引用文献数
- 3
Background: Hyperpolypharmacy is associated with adverse outcomes in older adults, but because literature on its association with cardiovascular (CV) outcomes after acute decompensated heart failure (ADHF) is sparse, we investigated the relationships among hyperpolypharmacy, medication class, and death in patients with HF.Methods and Results: We evaluated the total number of medications prescribed to 884 patients at discharge following ADHF. Patients were categorized into nonpolypharmacy (<5 medications), polypharmacy (5–9 medications), and hyperpolypharmacy (≥10 medications) groups. We examined the relationship of polypharmacy status with the 2-year mortality rate. The proportion of patients taking ≥5 medications was 91.3% (polypharmacy, 55.3%; hyperpolypharmacy, 36.0%). Patients in the hyperpolypharmacy group showed worse outcomes than patients in the other 2 groups (P=0.002). After multivariable adjustment, the total number of medications was significantly associated with an increased risk of death (hazard ratio [HR] per additional increase in the number of medications, 1.05; 95% confidence interval [CI], 1.01–1.10; P=0.027). Although the number of non-CV medications was significantly associated with death (HR, 1.07; 95% CI, 1.02–1.13; P=0.01), the number of CV medications was not (HR, 1.01; 95% CI, 0.92–1.10; P=0.95).Conclusions: Hyperpolypharmacy due to non-CV medications was associated with an elevated risk of death in patients after ADHF, suggesting the importance of a regular review of the prescribed drugs including non-CV medications.
- 著者
- Keisuke Machida Masatoshi Minamisawa Hirohiko Motoki Kanako Teramoto Yukari Okuma Masafumi Kanai Kazuhiro Kimura Takahiro Okano Yasushi Ueki Koji Yoshie Tamon Kato Tatsuya Saigusa Soichiro Ebisawa Ayako Okada Koichiro Kuwahara
- 出版者
- The Japanese Circulation Society
- 雑誌
- Circulation Journal (ISSN:13469843)
- 巻号頁・発行日
- pp.CJ-23-0129, (Released:2023-07-12)
- 参考文献数
- 29
Background: Acute decompensated heart failure (ADHF) has a poor prognosis and common comorbidities may be contributory. However, evidence for the association between dementia and clinical outcomes in patients with is sparse and it requires further investigation into risk reduction.Methods and Results: We assessed the clinical profiles and outcomes of 1,026 patients (mean age 77.8 years, 43.2% female) with ADHF enrolled in the CURE-HF registry to evaluate the relationship between investigator-reported dementia status and clinical outcomes (all-cause death, cardiovascular (CV) death, non-CV death, and HF hospitalization) over a median follow-up of 2.7 years. In total, dementia was present in 118 (11.5%) patients, who experienced more drug interruptions and HF admissions due to infection than those without dementia (23.8% vs. 13.1%, P<0.01; 11.0% vs. 6.0%, P<0.01, respectively). Kaplan-Meier analysis revealed that dementia patients had higher mortality rates than those without dementia (log-rank P<0.001). After multivariable adjustment for demographics and comorbidities, dementia was significantly associated with an increased risk of death (adjusted hazard ratio, 1.43; 95% confidence interval, 1.06–1.93, P=0.02) and non-CV death (adjusted hazard ratio, 1.65; 95% confidence interval, 1.04–2.62, P=0.03), but no significant associations between dementia and CV death or HF hospitalization were observed (both, P>0.1).Conclusions: In ADHF patients dementia was associated with aggravating factors for HF admission and elevated risk of death, primarily non-CV death.
- 著者
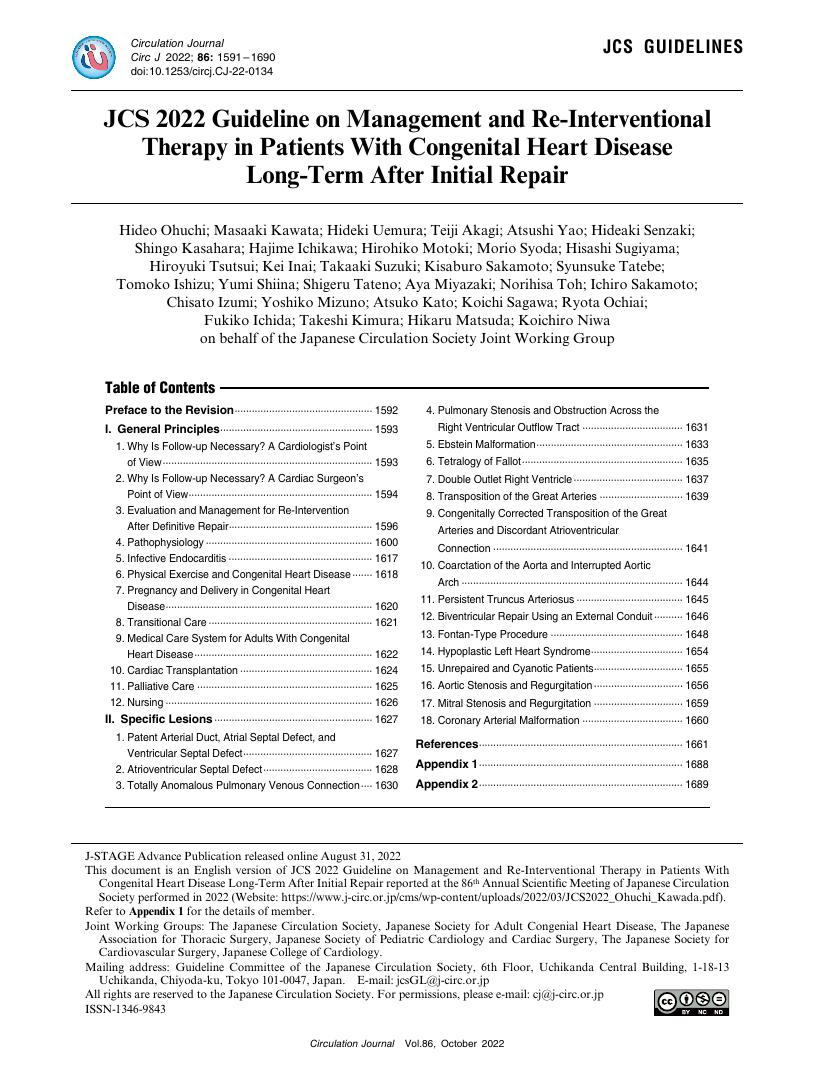
- Hideo Ohuchi Masaaki Kawata Hideki Uemura Teiji Akagi Atsushi Yao Hideaki Senzaki Shingo Kasahara Hajime Ichikawa Hirohiko Motoki Morio Syoda Hisashi Sugiyama Hiroyuki Tsutsui Kei Inai Takaaki Suzuki Kisaburo Sakamoto Syunsuke Tatebe Tomoko Ishizu Yumi Shiina Shigeru Tateno Aya Miyazaki Norihisa Toh Ichiro Sakamoto Chisato Izumi Yoshiko Mizuno Atsuko Kato Koichi Sagawa Ryota Ochiai Fukiko Ichida Takeshi Kimura Hikaru Matsuda Koichiro Niwa on behalf of the Japanese Circulation Society Joint Working Group
- 出版者
- The Japanese Circulation Society
- 雑誌
- Circulation Journal (ISSN:13469843)
- 巻号頁・発行日
- vol.86, no.10, pp.1591-1690, 2022-09-22 (Released:2022-09-22)
- 参考文献数
- 1071
- 被引用文献数
- 6
- 著者
- Sho Suzuki Hirohiko Motoki Yusuke Kanzaki Takuya Maruyama Naoto Hashizume Ayako Kozuka Kumiko Yahikozawa Koichiro Kuwahara
- 出版者
- The Japanese Circulation Society
- 雑誌
- Circulation Reports (ISSN:24340790)
- 巻号頁・発行日
- vol.1, no.3, pp.137-141, 2019-03-08 (Released:2019-03-08)
- 参考文献数
- 24
- 被引用文献数
- 1
Background: Clinical evidence of the effects of loop diuretics in patients with heart failure with preserved ejection fraction (HFpEF) is lacking. Thus, we compared the impact of azosemide and furosemide, long- and short-acting loop diuretics, in patients with HFpEF. Methods and Results: A prospective multicenter cohort study was conducted between July 2014 and July 2018. We enrolled 301 consecutive patients with HFpEF (median age, 84 years; IQR, 79–88 years; 54.8% female). Azosemide was used in 127 patients (azosemide group), and furosemide in 174 (furosemide group). We constructed Cox models for a composite of cardiac death, non-fatal myocardial infarction, non-fatal stroke, and HF hospitalization (primary endpoints). During a median follow-up of 317 days (IQR, 174–734 days), the primary endpoint occurred in 112 patients (37.2%). On multivariate inverse probability of treatment weighted (IPTW) Cox modeling, the azosemide group had a significantly lower incidence of adverse events than the furosemide group (hazard ratio [HR], 0.46; 95% confidence interval [CI]: 0.27–0.80; P=0.006). Furthermore, on multivariate IPTW Cox modeling for the secondary endpoints, cardiac death (HR, 0.38; 95% CI: 0.17–0.89; P=0.025) and unplanned hospitalization for decompensated HF (HR, 0.50; 95% CI: 0.28–0.89; P=0.018) were also reduced in the azosemide group. Conclusions: Azosemide significantly reduced the risk of adverse events compared with furosemide in HFpEF patients.