1 0 0 0 OA Morphological Analysis of the Sylvian Fissure Stem to Guide a Safe Trans-sylvian Fissure Approach
- 著者
- Yasutaka IMADA Chie MIHARA Hitoshi KAWAMOTO Kaoru KURISU
- 出版者
- The Japan Neurosurgical Society
- 雑誌
- Neurologia medico-chirurgica (ISSN:04708105)
- 巻号頁・発行日
- vol.62, no.11, pp.502-512, 2022-11-15 (Released:2022-11-15)
- 参考文献数
- 37
- 被引用文献数
- 1
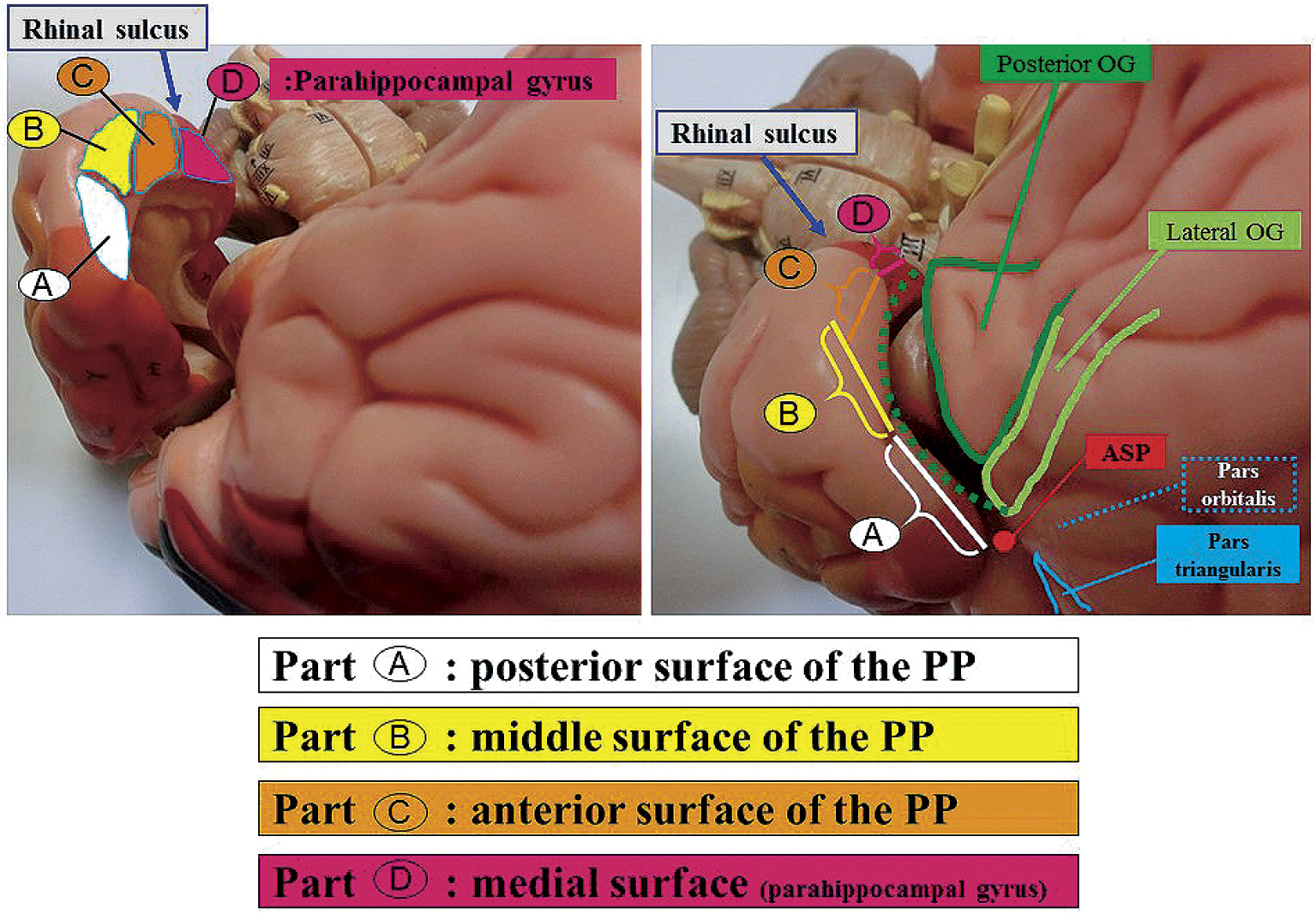
The sylvian fissure stem and its deep cisternal part (SDCP) consist mainly of the orbital gyrus (OG) and anterior medial portion of the temporal lobe. SDCP's adhesion has been found to make a trans-sylvian approach difficult due to the various patterns of adhesion. Thus, in this study, we aim to clarify the morphological features of the SDCP, and to guide a safe trans-sylvian approach. We retrospectively classified the morphology of the SDCP in 81 patients into 3 types (tight, moderate, loose type) according to the degree of adhesion of the arachnoid membrane and analyzed the morphological features of the OG and the temporal lobe using intraoperative video images. In addition, we have retrospectively measured each width of the SDCP's subarachnoid space at the three points (Point A, lateral superior portion; Point B, downward portion; Point C, medial inferior portion of SDCP) and analyzed their relationship to the degree of adhesion using the preoperative coronal three-dimensional computed tomography angiography (3D-CTA) images of 44 patients. As per the results, SDCP's adhesions were determined to be significantly tighter in cases with large OG and young cases. The temporal lobe had four surfaces (posterior, middle, anterior, and medial) that adhered to the OG in various patterns. The tighter the adhesion between the OG and each of the three distal surfaces of the temporal lobe, the narrower the width of the subarachnoid space at each point (A, B, C). Understanding of the morphological features of the SDCP, and estimating its adhesion preoperatively are useful in developing a surgical strategy and obtaining correct intraoperative orientation in the trans-sylvian approach.
- 著者
- Shingo MATSUDA Fusao IKAWA Hideo OHBA Michitsura YOSHIYAMA Toshikazu HIDAKA Kaoru KURISU Susumu MIYAMOTO Isao DATE Hiroyuki NAKASE
- 出版者
- The Japan Neurosurgical Society
- 雑誌
- Neurologia medico-chirurgica (ISSN:04708105)
- 巻号頁・発行日
- vol.59, no.6, pp.197-203, 2019 (Released:2019-06-15)
- 参考文献数
- 42
- 被引用文献数
- 1 7
Various guidelines regarding surgical site infection (SSI) have recently been established. However, perioperative management of the wound and use of antibiotics have never been standardized completely in departments of neurosurgery in Japan. This survey investigated current perioperative management and administration of surgical antibiotic prophylaxis (SAP) and compared with guidelines intended to reduce SSI associated with neurosurgery in Japan. Questionnaires were distributed to members of the conference on Neurosurgical Techniques and Tools and the Japan Society of Aesthetic Neurosurgery via internet. The questionnaires asked about methods of perioperative management. A total of 255 members returned answers to the questionnaires. The questionnaires revealed that partial or no removal of the hair and hair shampooing at the day before surgery were performed in 96.1% and 88.1% of each institute following the World Health Organization (WHO) guidelines. Use of SAP at just before, during, and after surgery were 65.0%, 86.2%, and 63.0%, respectively. The postoperative period of use of intravenous SAP prolonged beyond 24 h in 80.0% against the recommendation of WHO. Perioperative management of wounds and use of SAP varies in institutes in Japan and some procedures were far different from the WHO guidelines. Japanese neurosurgeons should notice the prolonged SAP and comply with the WHO guidelines.
- 著者
- Yasutaka IMADA Kaoru KURISU Toru TAKUMI Hirohiko AOYAMA Takashi SADATOMO Keisuke MIGITA Kiyoshi YUKI
- 出版者
- The Japan Neurosurgical Society
- 雑誌
- Neurologia medico-chirurgica (ISSN:04708105)
- 巻号頁・発行日
- vol.59, no.7, pp.264-270, 2019 (Released:2019-07-15)
- 参考文献数
- 24
- 被引用文献数
- 1 9
In this study, we used 45 adult cadaveric cerebral hemispheres to investigate the anatomical classification of the superficial middle cerebral vein (SMCV) based on the number of stems, course, and anastomosis at the distal portion. We classified the SMCVs into five types based on embryological concept. Type A (18 cases, 40.0%) is that the frontosylvian veins (FSVs) merge with the vein of Trolard (VT) and the vein of Labbé (VL) at the distal portion of the sylvian fissure. Type B (5 cases, 11.1%) is that the temporosylvian veins (TSVs) merge with the VT and the VL at the distal portion. Type C (13 cases, 28.9%) is that no vein merge with the VT and the VL at the distal portion. The VT merges with the SMCV from the FSV and the VL merges with the SMCV from the TSV. They course along the sylvian fissure and merge at the proximal portion. In Type D (eight cases: 17.8%), the VT and the VL merge at the distal portion, and the SMCV from the FSV and the SMCV from the TSV join their confluence without merging. Type E (one case, 2.2%) show an undeveloped SMCV. Formation rate of intravenous anastomoses or bridging veins(BVs) at the distal portion between the frontosylvian trunk (FST) and the temporosylvian trunk (TST), between the FST and the temporal lobe, and between the TST and the frontal lobe was very low, because these formation may be difficult to occur during the embryological process in which the SMCV is formed from the telencephalic vein.
- 著者
- Yasutaka IMADA Kaoru KURISU Toru TAKUMI Hirohiko AOYAMA Takashi SADATOMO Keisuke MIGITA Kiyoshi YUKI
- 出版者
- The Japan Neurosurgical Society
- 雑誌
- Neurologia medico-chirurgica (ISSN:04708105)
- 巻号頁・発行日
- pp.oa.2018-0284, (Released:2019-05-11)
- 参考文献数
- 24
- 被引用文献数
- 9
In this study, we used 45 adult cadaveric cerebral hemispheres to investigate the anatomical classification of the superficial middle cerebral vein (SMCV) based on the number of stems, course, and anastomosis at the distal portion. We classified the SMCVs into five types based on embryological concept. Type A (18 cases, 40.0%) is that the frontosylvian veins (FSVs) merge with the vein of Trolard (VT) and the vein of Labbé (VL) at the distal portion of the sylvian fissure. Type B (5 cases, 11.1%) is that the temporosylvian veins (TSVs) merge with the VT and the VL at the distal portion. Type C (13 cases, 28.9%) is that no vein merge with the VT and the VL at the distal portion. The VT merges with the SMCV from the FSV and the VL merges with the SMCV from the TSV. They course along the sylvian fissure and merge at the proximal portion. In Type D (eight cases: 17.8%), the VT and the VL merge at the distal portion, and the SMCV from the FSV and the SMCV from the TSV join their confluence without merging. Type E (one case, 2.2%) show an undeveloped SMCV. Formation rate of intravenous anastomoses or bridging veins(BVs) at the distal portion between the frontosylvian trunk (FST) and the temporosylvian trunk (TST), between the FST and the temporal lobe, and between the TST and the frontal lobe was very low, because these formation may be difficult to occur during the embryological process in which the SMCV is formed from the telencephalic vein.