- 著者
- Ichiro Nakagawa Masashi Kotsugi Shohei Yokoyama Ryosuke Maeoka Tomoya Okamoto Hiromitsu Sasaki Kenta Nakase Ai Okamoto Yudai Morisaki
- 出版者
- The Japanese Society for Neuroendovascular Therapy
- 雑誌
- Journal of Neuroendovascular Therapy (ISSN:18824072)
- 巻号頁・発行日
- pp.ra.2023-0018, (Released:2023-05-26)
- 参考文献数
- 50
Anterior cranial fossa (ACF) dural arteriovenous fistula (DAVF) is a rare lesion among cerebral DAVFs. This lesion shows significant bleeding risk because of the angioarchitecture, involving direct leptomeningeal retrograde venous drainage, as a nonsinus-type DAVF. Over the years, direct surgery has been considered the primary treatment for ACF DAVF, offering favorable clinical outcomes compared to a low complete obliteration rate with endovascular treatment and the relatively high risk of blindness due to central retinal artery occlusion with transophthalmic artery embolization. In recent years, however, significant improvements in DSA and 3D reconstruction imaging quality have allowed a much more precise understanding of the angioarchitecture of the shunt and vascular access route. In addition, advances in endovascular devices, including catheters and embolic materials, have facilitated microcatheter navigation into more distal vessels and more reliable closure of the fistulous point. Supported by such technological innovations, endovascular approaches to the treatment of ACF DAVF have been becoming successful first-line treatments. This article reviews the evolution of treatment strategies and the current status of endovascular treatment for ACF DAVF, with a particular focus on transarterial embolization.
- 著者
- Kenta NAKASE Ryosuke MATSUDA Tomoya OKAMOTO Ichiro NAKAGAWA Maiko TAKEDA Katsumi SAKATA Hiroyuki NAKASE
- 出版者
- The Japan Neurosurgical Society
- 雑誌
- NMC Case Report Journal (ISSN:21884226)
- 巻号頁・発行日
- vol.10, pp.315-320, 2023-12-31 (Released:2023-11-11)
- 参考文献数
- 30
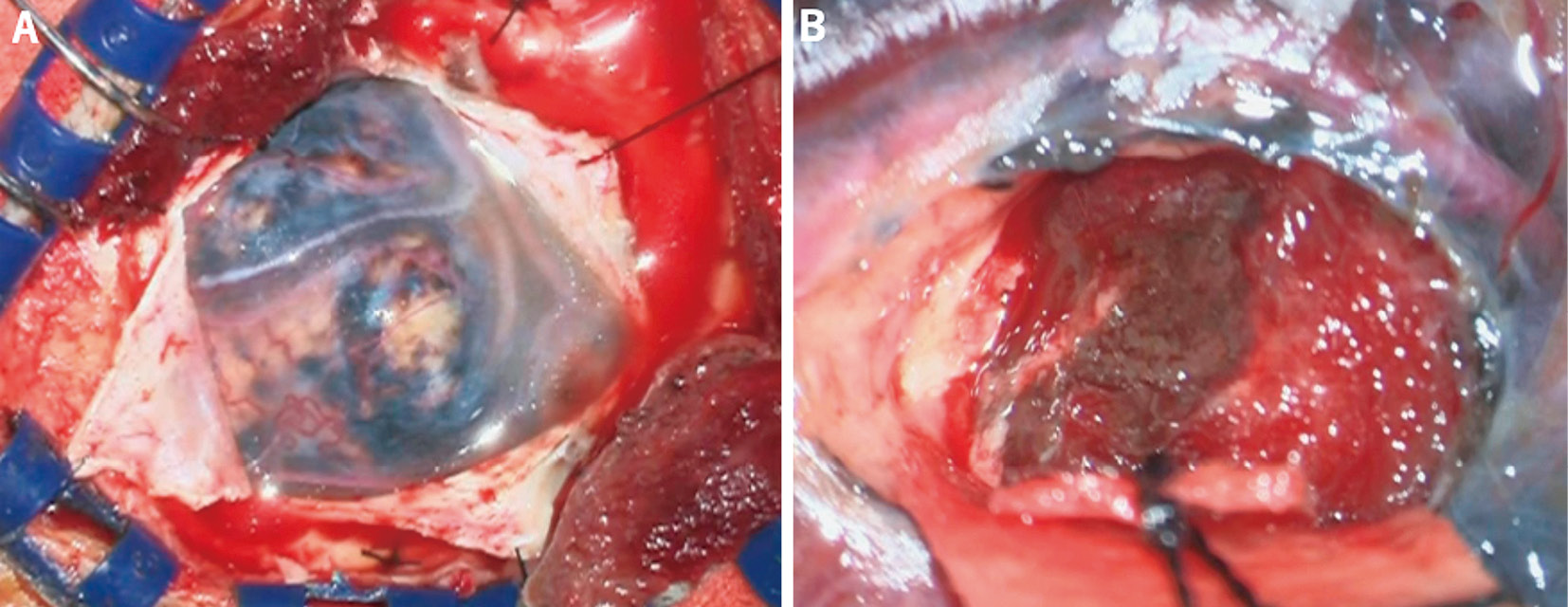
Meningeal melanocytomas of the central nervous system, although typically benign, rarely undergo malignant transformations. A 46-year-old man presented with headache and nausea 4 years after gross total resection of a craniovertebral junction meningeal melanocytoma at another hospital. The initial clinical course was previously reported.1) Computed tomography revealed the presence of multiple intracranial mass lesions. Furthermore, magnetic resonance imaging showed multiple intracranial lesions and meningeal dissemination. A biopsy was performed for a circumflex lesion located in the right frontal lobe. Pathological examination showed anaplastic changes and a Ki-67 index of 33%. Based on the pleomorphic changes and high mitotic activity, the patient was diagnosed with primary cerebral malignant melanoma. The patient received four cycles of nivolumab (80 mg) and ipilimumab (165 mg), followed by whole-brain radiotherapy (37.5 Gy). However, the disease progressed after the third cycle. Genome analysis revealed GNAQ Q209P and SF3B1 R625C mutations, but no treatments related to these gene mutations were available. Despite the seven cycles of nivolumab therapy, the patient eventually passed away 9 months after surgery. This case was a rare example of malignant transformation and leptomeningeal melanomatosis in a meningeal melanocytoma. It highlights the importance of careful follow up after gross total resection. Identification of molecular alterations can lead to better detection of melanocytic melanomas with poor prognosis and high risk of recurrence and metastasis. It can also facilitate the development of novel therapeutic options for these patients.