2 0 0 0 OA Barbed Suture Versus Interrupted Suture in Posterior Cervical Spine Surgery: Are They Equivalent?
- 著者
- Alan R. Tang Anthony M. Steinle Hani Chanbour Godwin Emeka-Ibe Byron F. Stephens Scott L. Zuckerman Amir M. Abtahi
- 出版者
- The Japanese Society for Spine Surgery and Related Research
- 雑誌
- Spine Surgery and Related Research (ISSN:2432261X)
- 巻号頁・発行日
- pp.2022-0076, (Released:2022-06-28)
- 被引用文献数
- 2
Introduction: Posterior cervical spine approaches have been associated with increased rates of wound complications compared to anterior approaches. While barbed suture wound closure for lumbar spine surgery has been shown to be safe and efficacious, there is no literature regarding its use in posterior cervical spine surgery. In a cohort of patients undergoing elective posterior cervical spine surgery, we sought to compare postoperative complication rates between barbed and traditional interrupted suture closure.Methods: A retrospective review of demographics, past medical history, and operative and postoperative variables collected from a prospective registry between July 1, 2016, and June 30, 2020 was undertaken. All patients 18 years old and above undergoing elective posterior cervical fusion were included. The primary outcome of interest was wound complications, including surgical site infection (SSI), dehiscence, or hematoma. In addition, numerical rating scale (NRS) neck pain (NP), NRS arm pain (AP), Neck Disability Index (NDI), and operative time were collected. A variety of statistical tests were used to compare the two suture groups.Results: Of 117 patients undergoing posterior cervical fusion, 89 (76%) were closed with interrupted suture and 28 (24%) with barbed suture. The interrupted cohort were more likely to have >1 comorbidity (p < 0.001), diabetes mellitus (p = 0.013), and coronary artery disease (p = 0.002). No difference in postoperative wound complications between interrupted/barbed sutures was observed after univariate (OR 1.07, 95% CI: 0.27–4.25, p = 0.927) and multivariable logistic regression analysis (OR 0.77, 95% CI: 0.15–4.00, p = 0.756). Univariate logistic regression revealed no differences in achieving minimal clinically important difference (MCID) NRS-NP (OR 0.73, 95% CI: 0.28–1.88, p = 0.508) or NRS-AP (OR 0.68, 95% CI: 0.25–1.90, p = 0.464) at 3 months between suture groups. The interrupted suture group was less likely to achieve MCID NDI at 3 months (OR 0.29, 95% CI: 0.11–0.80, p = 0.016)Conclusions: Barbed suture closure in posterior cervical spine surgery does not lead to higher rates of postoperative wound complications/SSI compared to traditional interrupted fascial closure.
- 著者
- Inamullah Khan Scott L. Parker Hansen Bow Ahilan Sivaganesan Jacquelyn S. Pennings Byron F. Stephens II Anthony M. Steinle Rishabh Gupta Clinton J. Devin
- 出版者
- The Japanese Society for Spine Surgery and Related Research
- 雑誌
- Spine Surgery and Related Research (ISSN:2432261X)
- 巻号頁・発行日
- pp.2021-0252, (Released:2022-04-12)
- 被引用文献数
- 3
Background: Surgical management of degenerative lumbar spine disorders is effective at improving patient pain, disability, and quality of life; however, obtaining a durable posterolateral fusion after decompression remains a challenge. Interbody fusion technologies are viable means of improving fusion rates in the lumbar spine, specifically various graft materials including autograft, structural allograft, titanium, and polyether ether ketone. This study assesses the effectiveness of Tritanium posterolateral cage in the treatment of degenerative disk disease.Methods: Nearest-neighbor 1:1 matched control transforaminal lumbar interbody fusion with PEEK vs. Tritanium posterior lumbar (PL) cage interbody fusion patients were identified using propensity scoring from patients that underwent elective surgery for degenerative disk diseases. Line graphs were generated to compare the trajectories of improvement in patient-reported outcomes (PROs) from baseline to 3 and 12 months postoperatively. The nominal data were compared via the χ2 test, while the continuous data were compared via Student's t-test.Results: The two groups had no difference regarding either the 3- or 12-month Euro-Qol-5D (EQ-5D), numeric rating scale (NRS) leg pain, and NRS back pain; however, the Tritanium interbody cage group had better Oswestry Disability Index (ODI) scores compared to the control group of the PEEK interbody cage at both 3 and 12 months (p = 0.013 and 0.048).Conclusions: Our results indicate the Tritanium cage is an effective alternative to the previously used PEEK cage in terms of PROs, surgical safety, and radiological parameters of surgical success. The Tritanium cohort showed better ODI scores, higher fusion rates, lower subsidence, and lower indirect costs associated with surgical management, when compared to the propensity-matched PEEK cohort.
- 著者
- William H. Waddell Benjamin M. Weisenthal Nicholas Golinvaux Abigail L. Henry Jacquelyn Pennings John P. Wanner Rishabh Gupta Toshitaka Yoshii Zhou Feifei Byron F. Stephens
- 出版者
- The Japanese Society for Spine Surgery and Related Research
- 雑誌
- Spine Surgery and Related Research (ISSN:2432261X)
- 巻号頁・発行日
- vol.6, no.5, pp.460-463, 2022-09-27 (Released:2022-09-27)
- 参考文献数
- 27
- 被引用文献数
- 2
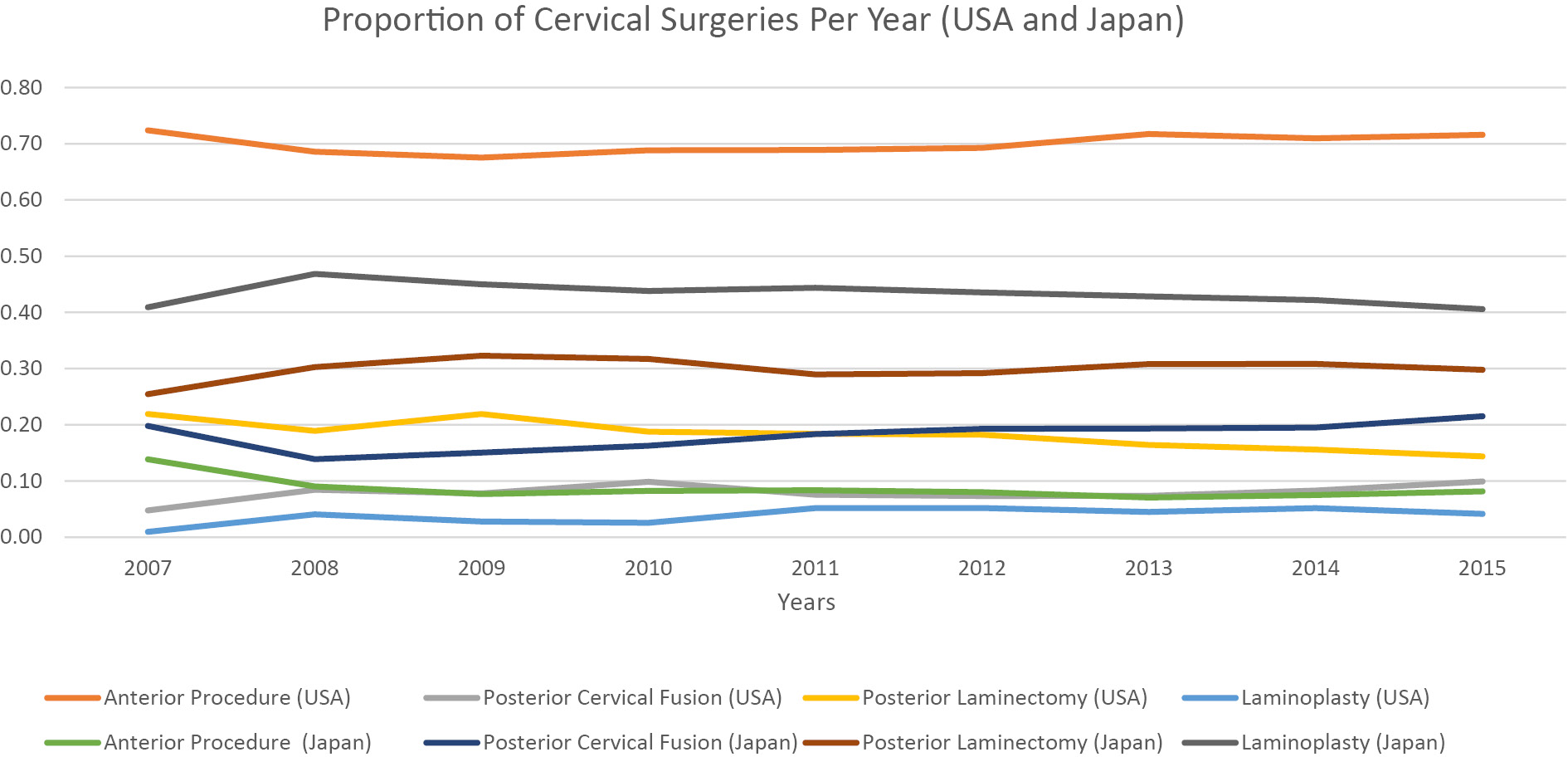
Introduction: Laminoplasty is a well-established technique used to manage cervical myelopathy (CM). Nevertheless, the degree to which United States surgeons have adopted laminoplasty from Japan to treat CM is less clear. The purpose of this study was to compare operative management strategies for CM in the United States (US) with Japan.Methods: This study used a retrospective cohort of 16,084 patients from the American College of Surgeons National Surgical Quality Improvement Program (ACS-NSQIP) database and 389,872 patients from the Japanese Diagnosis Procedure Combination (DPC) database from 2007 to 2015. Patients with the following diagnoses were collected: spondylosis with myelopathy (ICD-19; 721.1, ICD-10; M47.12) and disk herniation with myelopathy (ICD-9; 722.71, ICD-10; M50.00). The proportion of surgeries between Japan and the US was compared using a linear regression model controlling for year.Results: US surgeons utilized anterior procedures in 70% of cases compared to 9% in Japan (p<.001). In contrast, Japan had significantly more laminoplasties than the US (43% vs. 4%, respectively, p<.001). The percentage of laminoplasty in Japan (43%) relative to the percentage in the US (4%) was significantly different (p<.001). Accounting for increases in the number of total surgeries per year seen in the ACS-NSQIP and DPC databases, no specific surgery demonstrated a significant increase or decrease over the 8 years.Conclusions: Japanese surgeons employ laminoplasty to treat CM approximately ten times more frequently than US surgeons who prefer anterior procedures.