- 著者
- Inamullah Khan Scott L. Parker Hansen Bow Ahilan Sivaganesan Jacquelyn S. Pennings Byron F. Stephens II Anthony M. Steinle Rishabh Gupta Clinton J. Devin
- 出版者
- The Japanese Society for Spine Surgery and Related Research
- 雑誌
- Spine Surgery and Related Research (ISSN:2432261X)
- 巻号頁・発行日
- pp.2021-0252, (Released:2022-04-12)
- 被引用文献数
- 3
Background: Surgical management of degenerative lumbar spine disorders is effective at improving patient pain, disability, and quality of life; however, obtaining a durable posterolateral fusion after decompression remains a challenge. Interbody fusion technologies are viable means of improving fusion rates in the lumbar spine, specifically various graft materials including autograft, structural allograft, titanium, and polyether ether ketone. This study assesses the effectiveness of Tritanium posterolateral cage in the treatment of degenerative disk disease.Methods: Nearest-neighbor 1:1 matched control transforaminal lumbar interbody fusion with PEEK vs. Tritanium posterior lumbar (PL) cage interbody fusion patients were identified using propensity scoring from patients that underwent elective surgery for degenerative disk diseases. Line graphs were generated to compare the trajectories of improvement in patient-reported outcomes (PROs) from baseline to 3 and 12 months postoperatively. The nominal data were compared via the χ2 test, while the continuous data were compared via Student's t-test.Results: The two groups had no difference regarding either the 3- or 12-month Euro-Qol-5D (EQ-5D), numeric rating scale (NRS) leg pain, and NRS back pain; however, the Tritanium interbody cage group had better Oswestry Disability Index (ODI) scores compared to the control group of the PEEK interbody cage at both 3 and 12 months (p = 0.013 and 0.048).Conclusions: Our results indicate the Tritanium cage is an effective alternative to the previously used PEEK cage in terms of PROs, surgical safety, and radiological parameters of surgical success. The Tritanium cohort showed better ODI scores, higher fusion rates, lower subsidence, and lower indirect costs associated with surgical management, when compared to the propensity-matched PEEK cohort.
- 著者
- William H. Waddell Benjamin M. Weisenthal Nicholas Golinvaux Abigail L. Henry Jacquelyn Pennings John P. Wanner Rishabh Gupta Toshitaka Yoshii Zhou Feifei Byron F. Stephens
- 出版者
- The Japanese Society for Spine Surgery and Related Research
- 雑誌
- Spine Surgery and Related Research (ISSN:2432261X)
- 巻号頁・発行日
- vol.6, no.5, pp.460-463, 2022-09-27 (Released:2022-09-27)
- 参考文献数
- 27
- 被引用文献数
- 2
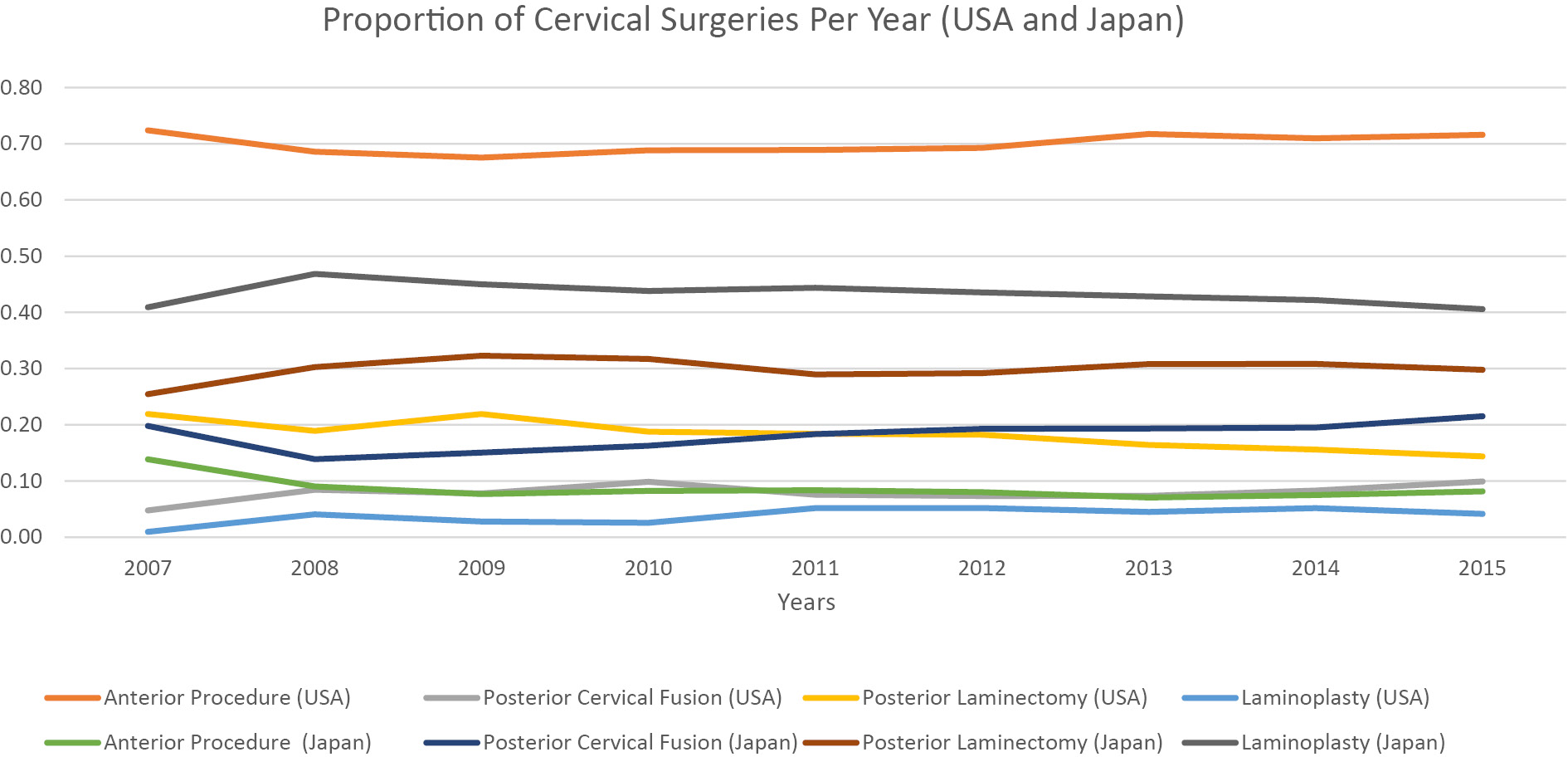
Introduction: Laminoplasty is a well-established technique used to manage cervical myelopathy (CM). Nevertheless, the degree to which United States surgeons have adopted laminoplasty from Japan to treat CM is less clear. The purpose of this study was to compare operative management strategies for CM in the United States (US) with Japan.Methods: This study used a retrospective cohort of 16,084 patients from the American College of Surgeons National Surgical Quality Improvement Program (ACS-NSQIP) database and 389,872 patients from the Japanese Diagnosis Procedure Combination (DPC) database from 2007 to 2015. Patients with the following diagnoses were collected: spondylosis with myelopathy (ICD-19; 721.1, ICD-10; M47.12) and disk herniation with myelopathy (ICD-9; 722.71, ICD-10; M50.00). The proportion of surgeries between Japan and the US was compared using a linear regression model controlling for year.Results: US surgeons utilized anterior procedures in 70% of cases compared to 9% in Japan (p<.001). In contrast, Japan had significantly more laminoplasties than the US (43% vs. 4%, respectively, p<.001). The percentage of laminoplasty in Japan (43%) relative to the percentage in the US (4%) was significantly different (p<.001). Accounting for increases in the number of total surgeries per year seen in the ACS-NSQIP and DPC databases, no specific surgery demonstrated a significant increase or decrease over the 8 years.Conclusions: Japanese surgeons employ laminoplasty to treat CM approximately ten times more frequently than US surgeons who prefer anterior procedures.