- 著者
- Ji Woong Roh SungA Bae Thomas W. Johnson Seok-Jae Heo Yongcheol Kim Deok-Kyu Cho Jung-Sun Kim Byeong-Keuk Kim Donghoon Choi Myeong-Ki Hong Yangsoo Jang Myung Ho Jeong on behalf of the KAMIR-NIH Investigators
- 出版者
- The Japanese Circulation Society
- 雑誌
- Circulation Journal (ISSN:13469843)
- 巻号頁・発行日
- pp.CJ-23-0189, (Released:2023-05-30)
- 参考文献数
- 21
- 被引用文献数
- 3
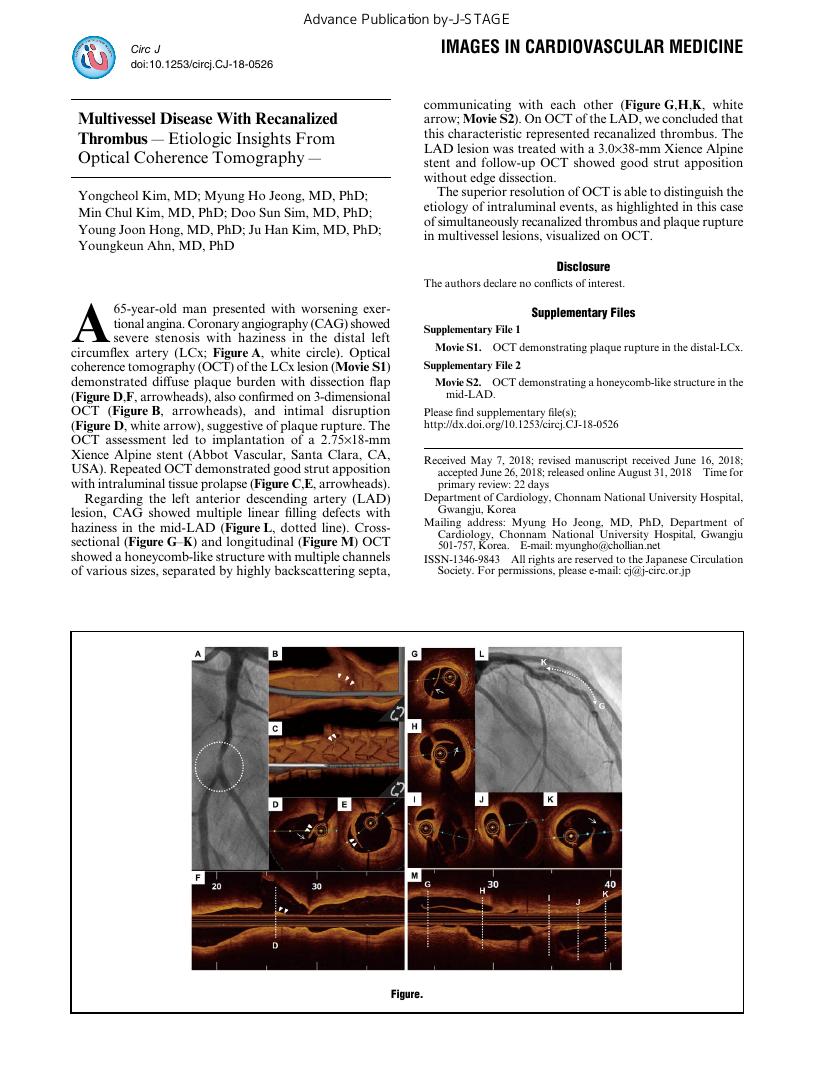
Background: In the setting of acute myocardial infarction (AMI), there are no data regarding the benefits of intravascular ultrasound (IVUS) for chronic kidney disease (CKD) patients.Methods and Results: This study used data from the Korea Acute Myocardial Infarction Registry, a large, multicenter prospective cohort. We evaluated 1,759 patients with AMI and CKD, defined as estimated glomerular filtration rate (eGFR) <60 mL/min/1.73 m2, and patients were classified into 2 groups: with and without IVUS. The primary outcome was target lesion failure (TLF) at 3 years. The hazard ratio (HR) of TLF according to eGFR was also analyzed. A total of 1,759 patients with AMI and CKD who underwent IVUS-guided PCI (19.2%) had a significantly lower risk of TLF at 3 years (8.9% vs. 15.3%; HR 0.55; 95% confidence interval [CI]: 0.38 to 0.81; P=0.002) than those who underwent angiography-guided PCI, regardless of their eGFR and the presence of end-stage renal disease (ESRD). The results were consistent after confounder adjustment and inversed probability weighting.Conclusions: In patients with CKD and AMI who underwent PCI with 2nd-generation DES implantation, the use of IVUS guidance was associated with a significant reduction in 3-year TLF and showed consistently favorable outcomes regardless of eGFR and ESRD.
- 著者
- Doyeon Hwang Hyun Kuk Kim Joo Myung Lee Ki Hong Choi Jihoon Kim Tae-Min Rhee Jonghanne Park Taek Kyu Park Jeong Hoon Yang Young Bin Song Jin-Ho Choi Joo-Yong Hahn Seung-Hyuk Choi Bon-Kwon Koo Young Jo Kim Shung Chull Chae Myeong Chan Cho Chong Jin Kim Hyeon-Cheol Gwon Myung Ho Jeong Hyo-Soo Kim The KAMIR Investigators
- 出版者
- The Japanese Circulation Society
- 雑誌
- Circulation Journal (ISSN:13469843)
- 巻号頁・発行日
- pp.CJ-17-1221, (Released:2018-02-28)
- 参考文献数
- 31
- 被引用文献数
- 14
Background:There has been debate regarding the added benefit of high-intensity statins compared with low-moderate-intensity statins, especially in patients with acute myocardial infarction (AMI).Methods and Results:The Korea Acute Myocardial Infarction Registry-National Institutes of Health consecutively enrolled 13,104 AMI patients. Of these, a total of 12,182 patients, who completed 1-year follow-up, were included in this study, and all patients were classified into 3 groups (no statin; low-moderate-intensity statin; and high-intensity statin). The primary outcome was major adverse cardiac event (MACE) including cardiac death, non-fatal MI, and repeat revascularization at 1 year. Both low-moderate-intensity and high-intensity statin significantly reduced low-density lipoprotein cholesterol (LDL-C; all P<0.001). Compared with the no statin group, both statin groups had significantly lower risk of MACE (low-moderate intensity: HR, 0.506; 95% CI: 0.413–0.619, P<0.001; high intensity: HR, 0.464; 95% CI: 0.352–0.611, P<0.001). The risk of MACE, however, was similar between the low-moderate- and high-intensity statin groups (HR, 0.917; 95% CI: 0.760–1.107, P=0.368). Multivariable adjustment, propensity score matching, and inverse probability weighted analysis also produced the same results.Conclusions:When adequate LDL-C level is achieved, patients on a low-moderate-intensity statin dose have similar cardiovascular outcomes to those on high-intensity statins.
- 著者
- Albert Youngwoo Jang Minsu Kim Pyung Chun Oh Soon Yong Suh Kyounghoon Lee Woong Chol Kang Ki Hong Choi Young Bin Song Hyeon-Cheol Gwon Hyo-Soo Kim Woo Jung Chun Seung-Ho Hur Seung-Woon Rha In-Ho Chae Jin-Ok Jeong Jung Ho Heo Junghan Yoon Soon Jun Hong Jong-Seon Park Myeong-Ki Hong Joon-Hyung Doh Kwang Soo Cha Doo-Il Kim Sang Yeub Lee Kiyuk Chang Byung-Hee Hwang So-Yeon Choi Myung Ho Jeong Chang-Wook Nam Bon-Kwon Koo Seung Hwan Han
- 出版者
- The Japanese Circulation Society
- 雑誌
- Circulation Journal (ISSN:13469843)
- 巻号頁・発行日
- vol.86, no.9, pp.1365-1375, 2022-08-25 (Released:2022-08-25)
- 参考文献数
- 17
- 被引用文献数
- 1 1
Background: Differences in the impact of the 1- or 2-stent strategy in similar coronary bifurcation lesion conditions are not well understood. This study investigated the clinical outcomes and its predictors between 1 or 2 stents in propensity score-matched (PSM) complex bifurcation lesions.Methods and Results: We analyzed the data of patients with bifurcation lesions, obtained from a multicenter registry of 2,648 patients (median follow up, 53 months). The patients were treated by second generation drug-eluting stents (DESs). The primary outcome was target lesion failure (TLF), composite of cardiac death, target vessel myocardial infarction (TVMI), and ischemia-driven target lesion revascularization (TLR). PSM was performed to balance baseline clinical and angiographic discrepancies between 1 and 2 stents. After PSM (N=333 from each group), the 2-stent group had more TLRs (hazard ratio [HR] 3.14, 95% confidence interval [CI] 1.42–6.97, P=0.005) and fewer hard endpoints (composite of cardiac death and TVMI; HR 0.44, 95% CI 0.19–1.01, P=0.054), which resulted in a similar TLF rate (HR 1.40, 95% CI 0.83–2.37, P=0.209) compared to the 1-stent group. Compared with 1-stent, the 2-stent technique was more frequently associated with less TLF in the presence of main vessel (pinteraction=0.008) and side branch calcification (pinteraction=0.010).Conclusions: The 2-stent strategy should be considered to reduce hard clinical endpoints in complex bifurcation lesions, particularly those with calcifications.
- 著者
- Yongcheol Kim Myung Ho Jeong Min Chul Kim Doo Sun Sim Young Joon Hong Ju Han Kim Youngkeun Ahn
- 出版者
- The Japanese Circulation Society
- 雑誌
- Circulation Journal (ISSN:13469843)
- 巻号頁・発行日
- pp.CJ-18-0526, (Released:2018-08-31)
- 著者
- Doo Sun Sim Youngkeun Ahn Myung Ho Jeong Young Jo Kim Shung Chull Chae Taek Jong Hong In Whan Seong Jei Keon Chae Chong Jin Kim Myeong Chan Cho Ki Bae Seung
- 出版者
- 一般社団法人 インターナショナル・ハート・ジャーナル刊行会
- 雑誌
- International Heart Journal (ISSN:13492365)
- 巻号頁・発行日
- vol.54, no.4, pp.185-191, 2013 (Released:2013-08-06)
- 参考文献数
- 21
- 被引用文献数
- 8 21
The clinical outcome of patients with acute myocardial infarction (MI) with unprotected left main coronary artery (LMCA) stenosis is not fully understood. We sought to assess the outcomes of patients with acute MI who underwent percutaneous coronary intervention (PCI) for unprotected LMCA stenosis. A total of 587 patients enrolled in the Korea Acute Myocardial Infarction Registry with LMCA stenosis were analyzed. Patients with culprit LMCA had higher inhospital mortality than patients with non-culprit LMCA (16.0% versus 8.9%, P = 0.008), but had similar clinical outcomes during a 12-month follow-up. Compared to CABG, PCI using drug-eluting stents (DES) was more frequently performed with similar early and 12-month clinical outcomes. The efficacy of sirolimus-eluting stents, paclitaxel-eluting stents, and zotarolimus-eluting stents were comparable at 12-month clinical follow-up. Predictors of 12-month mortality included mechanical ventilation, cardiogenic shock, age > 65 years, and ejection fraction < 40%. Patients with acute MI and culprit LMCA have higher early mortality than patients with non-culprit LMCA. PCI with DES is frequently performed and the clinical outcome is similar between the 3 types of first-generation DES.