- 著者
- Yuki Ebisudani Kenji Sugiu Satoshi Murai Jun Haruma Masafumi Hiramatsu Tomohito Hishikawa Isao Date
- 出版者
- The Japanese Society for Neuroendovascular Therapy
- 雑誌
- Journal of Neuroendovascular Therapy (ISSN:18824072)
- 巻号頁・発行日
- pp.ra.2022-0062, (Released:2023-07-21)
- 参考文献数
- 21
Objective: Simulation training has focused on education and practical training. However, the adoption rate of neurointerventional simulation training in Japan is unknown. Therefore, we sent a questionnaire survey form to consulting specialists from the Japanese Society for Neuroendovascular Therapy (JSNET) to clarify the actual simulation training situation and compare the differences between university hospitals and general hospitals in Japan.Methods: The questionnaire survey was conducted in 243 neurosurgical training facilities that had JSNET consulting specialists between May 31, 2021 and July 31, 2021. The questionnaire survey forms were distributed by Google Forms.Results: A total of 162 facilities responded to the survey (response rate: 66.7%; 35.2% from university hospitals and 64.8% from general hospitals). The adoption rate for simulation training was 53.7%, and it was significantly higher in the university hospitals than in the general hospitals (64.9% vs. 47.6%, p = 0.035). On the simulation effectiveness survey, more than 80% of respondents answered that the simulation training was a useful tool for upskill training. The open-ended question on interventional simulation training showed that there are limiting factors such as financial constraints. Additionally, respondents expressed a desire for a standard neurointerventional simulation training and education program.Conclusion: The adoption rate for simulation training was 53.7% in the training facilities of JSNET, and it was higher in the university hospitals than in the general hospitals. Most of the respondents answered that simulation training is an effective tool to improve neurointerventional skills. They also requested the establishment of simulation training programs and simulation tools.
- 著者
- Takayuki KAKIMOTO Satoshi MURAI Noboru KUSAKA Fukiko BABA Yohei INOUE Hayato MIYAKE Masato KAWAKAMI Yukei SHINJI Hisakazu ITAMI Shinji OTSUKA Tsukasa NISHIURA Kenji KAWAMOTO Tsuyoshi YAMAMOTO Nobuhiko KIMURA Kotaro OGIHARA
- 出版者
- The Japan Neurosurgical Society
- 雑誌
- NMC Case Report Journal (ISSN:21884226)
- 巻号頁・発行日
- vol.10, pp.21-25, 2023-12-31 (Released:2023-02-23)
- 参考文献数
- 11
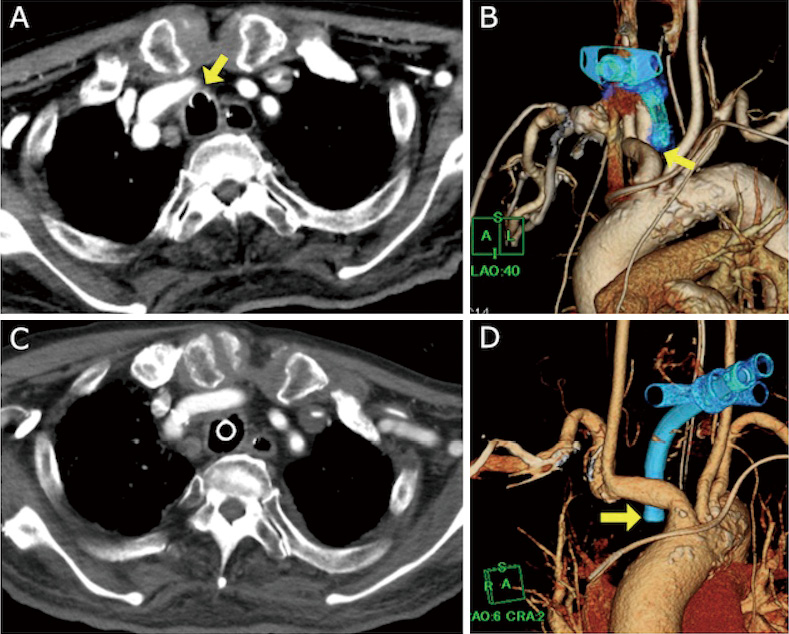
A 78-year-old man underwent a tracheostomy after embolization for a dural arteriovenous fistula. Seventy days after tracheostomy, arterial bleeding appeared through the tracheal stoma. The bleeding stopped spontaneously. However, two days later, arterial bleeding reappeared, and he was diagnosed with a tracheo-innominate artery fistula (TIF). He then underwent urgent endovascular covered stent placement. After the procedure, there was no bleeding. TIF can be a fatal complication after tracheostomy and it is generally treated with open chest surgery. However, a successful endovascular treatment for TIF has recently been reported and may yield better results.
- 著者
- Takao YASUHARA Satoshi MURAI Nobuhiro MIKUNI Susumu MIYAMOTO Isao DATE
- 出版者
- The Japan Neurosurgical Society
- 雑誌
- Neurologia medico-chirurgica (ISSN:04708105)
- 巻号頁・発行日
- vol.60, no.7, pp.337-350, 2020 (Released:2020-07-15)
- 参考文献数
- 14
- 被引用文献数
- 4 5
Cranial implants are commonly used throughout the world, yet the data on complications remain partly clarified. The aim of this study was to gather real data in 2018 on complications related to cranial implants in neurosurgery. The survey population consisted of 1103 institutes supplying neurosurgical treatment. The survey consisted of two-stage questionnaire. First the incidence of complications was investigated, then the secondary questionnaire was e-mailed to the respondents about the detailed of the complications. As the result, the annual incidence of complications related to cranial implants was 0.558% in Japan. Titanium plate and mesh were used predominantly in craniotomy and cranioplasty, respectively. The second survey collected data on 449 cases with complications (infection: 63%, implant exposure: 46%, multiple answer). Postoperative infection was associated with male sex, brain tumor, short interval between surgery and complication, usage of ceramics, hydroxyapatite, resin, and artificial dura, hyponutrition, multiple surgeries, dirty wound, and sinusitis as patient factors, and CSF leakage, ruptured sutures, and sinus maltreatment as surgery factors. Meanwhile, long hospital stay was associated with age, male sex, mRS 3–5 before complication, short interval between initial surgery and complication, large craniotomy, long operative time, usage of ceramics and artificial dura, multiple surgeries and dirty wound as patient factors, ruptured suture as a surgical factor, and bacterial infection, especially MRSA infection, as the complication and treatment consisting of removal as complication factors. In conclusion, this is the first Japanese national survey on complications related to cranial implants in neurosurgery. It is important to recall that complications may arise years after surgery and to be aware of the risk factors associated with complications.
- 著者
- Satoru YABUNO Takao YASUHARA Satoshi MURAI Tetsuya YUMOTO Hiromichi NAITO Atsunori NAKAO Isao DATE
- 出版者
- The Japan Neurosurgical Society
- 雑誌
- Neurologia medico-chirurgica (ISSN:04708105)
- 巻号頁・発行日
- vol.62, no.10, pp.465-474, 2022-10-15 (Released:2022-10-15)
- 参考文献数
- 61
- 被引用文献数
- 2
Intensive care unit (ICU) survivors after traumatic brain injury (TBI) frequently have serious disabilities with subsequent difficulty in reintegration into society. We aimed to investigate outcomes for ICU survivors after moderate to severe TBI (msTBI) and to identify predictive factors of return home (RH) and return to work (RTW). This single-center retrospective cohort study was conducted on all trauma patients admitted to the emergency ICU of our hospital between 2013 and 2017. Of these patients, adult (age ≥ 18 years) msTBI patients with head Abbreviated Injury Scale ≥ 3 were extracted. We performed univariate/multivariate logistic regression analyses to explore the predictive factors of RH and RTW. Among a total of 146 ICU survivors after msTBI, 107 were included (median follow-up period: 26 months). The RH and RTW rates were 78% and 35%, respectively. Multivariate analyses revealed that the predictive factors of RH were age < 65 years (P < 0.001), HR < 76 bpm (P = 0.015), platelet count ≥ 19× 104/μL (P = 0.0037), D-dimer < 26 μg/mL (P = 0.034), and Glasgow Coma Scale (GCS) score > 8 (P = 0.0015). Similarly, the predictive factors of RTW were age < 65 years (P < 0.001) and GCS score > 8 (P = 0.0039). This study revealed that "age" and "GCS score on admission" affected RH and RTW for ICU survivors after msTBI.