- 著者
- Shungo Imai Kenji Momo Hitoshi Kashiwagi Takayuki Miyai Mitsuru Sugawara Yoh Takekuma
- 出版者
- The Pharmaceutical Society of Japan
- 雑誌
- Biological and Pharmaceutical Bulletin (ISSN:09186158)
- 巻号頁・発行日
- vol.43, no.10, pp.1519-1525, 2020-10-01 (Released:2020-10-01)
- 参考文献数
- 37
- 被引用文献数
- 7
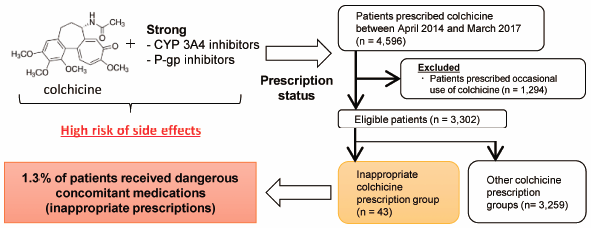
The anti-inflammatory agent colchicine may cause toxic effects such as rhabdomyolysis, pancytopenia, and acute respiratory distress syndrome in cases of overdose and when patients have renal or liver impairment. As colchicine is a substrate for CYP3A4 and P-glycoprotein (P-gp), drug–drug interactions are important factors that cause fatal colchicine-related side effects. Thus, we conducted a nation-wide survey to determine the status of inappropriate colchicine prescriptions in Japan. Patients prescribed the regular use of colchicine from April 2014 to March 2017 were identified using the Japanese large health insurance claims database. As the primary endpoint, we evaluated the concomitant prescription proportions of strong CYP3A4 and/or P-gp inhibitors classified as “contraindications for co-administration” with colchicine in patients with renal or liver impairment. We defined these cases as “inappropriate colchicine prescriptions.” Additionally, factors affecting inappropriate colchicine prescriptions were analyzed. Among the 3302 enrolled patients, 43 (1.30%) were inappropriately prescribed colchicine. Of these 43 patients, 11 had baseline renal and/or liver impairment. By multiple regression analysis, the primary diseases “gout” and “Behçet’s disease” were extracted as independent factors for inappropriate colchicine prescriptions with odds ratios of 0.40 (95% confidence interval: 0.19–0.84) and 4.93 (95% confidence interval: 2.12–11.5), respectively. We found that approximately 1% of patients had important colchicine interactions. Particularly, Behçet’s disease was a risk factor for inappropriate prescriptions, with approximately 25% of patients showing renal and/or liver impairment (classified as “contraindications for co-administration”). These findings may be useful for medical professionals who prescribe colchicine therapy.
- 著者
- Shungo Imai Yoh Takekuma Takayuki Miyai Mitsuru Sugawara
- 出版者
- The Pharmaceutical Society of Japan
- 雑誌
- Biological and Pharmaceutical Bulletin (ISSN:09186158)
- 巻号頁・発行日
- vol.43, no.1, pp.188-193, 2020-01-01 (Released:2020-01-01)
- 参考文献数
- 18
- 被引用文献数
- 22
This study aimed to construct an optimal algorithm for initial dose settings of vancomycin (VCM) using machine learning (ML) with decision tree (DT) analysis. Patients who were administered intravenous VCM and underwent therapeutic drug monitoring (TDM) at the Hokkaido University Hospital were enrolled. The study period was November 2011 to March 2019. In total, 654 patients were included in the study. Patients were divided into two groups, training (patients who received VCM from November 2011 to December 2017; n = 496) and testing (patients who received VCM from January 2018 to March 2019; n = 158) groups. For the training group, DT analysis of the classification and regression tree algorithm was performed to construct an algorithm (called DT algorithm) for the initial dose settings of VCM. For the testing group, the rates of attaining the VCM therapeutic range (trough value = 10–15 and 10–20 mg/L) with the DT algorithm and three conventional dose-setting methods were compared for model evaluation. The DT algorithm was constructed to be used for patients with estimated glomerular filtration rate ≥50 mL/min and body weight ≥40 kg. As a result, the recommended daily doses ranged from 20.0 to 58.1 mg/kg. In model evaluation, the DT algorithm obtained the highest rates of attaining the VCM therapeutic range compared to conventional dose-setting methods. Therefore, our DT algorithm can be applied to clinical practice. In addition, ML is useful for setting drug doses.
- 著者
- Shungo Imai Kenji Momo Hitoshi Kashiwagi Yuki Sato Takayuki Miyai Mitsuru Sugawara Yoh Takekuma
- 出版者
- Society for Clinical Epidemiology
- 雑誌
- Annals of Clinical Epidemiology (ISSN:24344338)
- 巻号頁・発行日
- vol.4, no.1, pp.6-10, 2022 (Released:2022-01-07)
- 参考文献数
- 15
- 著者
- Shungo Imai Yasuyuki Nasuhara Kenji Momo Hiromitsu Oki Hitoshi Kashiwagi Yuki Sato Takayuki Miyai Mitsuru Sugawara Yoh Takekuma
- 出版者
- The Pharmaceutical Society of Japan
- 雑誌
- Biological and Pharmaceutical Bulletin (ISSN:09186158)
- 巻号頁・発行日
- vol.44, no.10, pp.1499-1505, 2021-10-01 (Released:2021-10-01)
- 参考文献数
- 27
- 被引用文献数
- 4
A major adverse effect of benzbromarone is hepatotoxicity. Therefore, periodic liver function tests are required at least for the first 6 months of benzbromarone administration. However, it is not clear whether the relevant blood tests are implemented appropriately. Here, we performed a cross-sectional survey of the implementation status of liver function tests in patients who were newly prescribed benzbromarone, using the Japanese large claims database. Male patients who were newly prescribed benzbromarone from January 2010 to December 2016 were included. We targeted patients who continued benzbromarone during the observation period (up to 180 d from the start of administration). The primary endpoint was the proportion of patients in whom periodic liver function tests were implemented. A periodic liver function test was defined as one or more liver function tests performed during both 1–90 and 91–180 d of initial benzbromarone administration. We labeled the tests as a “periodic test” or “non-periodic test” based on whether periodic liver function tests were performed or not, respectively. Furthermore, factors influencing non-periodic test were analyzed. Periodic testing was implemented only in 28.7% of patients. Additionally, factors such as number of hospital beds ≤19 (compared to 100–199 beds) and duration of the first prescription of benzbromarone were associated with non-periodic testing. Our study revealed that periodic liver function tests are not performed sufficiently in Japan. Thus, clinicians prescribing benzbromarone should be educated about the test. Our blood-test-based approach should be applied to other drugs and countries in future research.
- 著者
- Shungo Imai Kenji Momo Hitoshi Kashiwagi Takayuki Miyai Mitsuru Sugawara Yoh Takekuma
- 出版者
- The Pharmaceutical Society of Japan
- 雑誌
- Biological and Pharmaceutical Bulletin (ISSN:09186158)
- 巻号頁・発行日
- vol.44, no.3, pp.448-452, 2021-03-01 (Released:2021-03-01)
- 参考文献数
- 23
Antibiotic-associated diarrhea (AAD) is a typical side effect of antibiotic treatment, especially in children. Amoxicillin (AMPC) and amoxicillin/clavulanate (AMPC/CVA) are associated with high risk of AAD; however, these antibiotics are important in the pediatric field. Recent research suggests that probiotics prevent pediatric AAD, including that caused by AMPC and AMPC/CVA. Indeed, guidelines for acute otitis media in children recommend the concomitant use of probiotics. However, the prescription status of probiotics for pediatric patients with otitis media receiving oral AMPC and AMPC/CVA remains unknown. We therefore conducted a survey to clarify the current status of these prescriptions and, in particular, to identify specific populations with a low proportion of probiotic prescriptions. Pediatric patients (≤15 years of age) newly prescribed oral AMPC or AMPC/CVA for otitis media between April 2016 and March 2017 were identified from a Japanese health insurance claims database. Eligible patients were divided into the AMPC (1303 patients) and AMPC/CVA (424 patients) groups, in which 659 (50.6%) and 293 (69.1%) patients were prescribed probiotics, respectively. Of the patients receiving probiotic prescriptions in the AMPC and AMPC/CVA groups, 632 (95.9%) and 286 (97.6%) patients received antibiotic-resistant probiotic prescriptions, respectively. When classified by the prescribing clinical department and patient age, the proportions of probiotic prescriptions in Internal Medicine and Pediatrics departments were lower than those in the Otorhinolaryngology department regardless of age. These results indicate the probability of insufficient probiotic prescriptions for pediatric patients with otitis media. Solving this issue may lead to the provision of safer antimicrobial therapy.