- 著者
- Tomoo Inoue
- 出版者
- Information Processing Society of Japan
- 雑誌
- Journal of Information Processing (ISSN:18826652)
- 巻号頁・発行日
- vol.26, pp.169-169, 2018 (Released:2018-02-15)
- 著者
- Arata NAGAI Yasuhiro SUZUKI Tomohisa ISHIDA Yoshimichi SATO Tomoo INOUE Teiji TOMINAGA
- 出版者
- The Japan Neurosurgical Society
- 雑誌
- Neurologia medico-chirurgica (ISSN:04708105)
- 巻号頁・発行日
- pp.2022-0155, (Released:2022-10-13)
- 参考文献数
- 31
- 被引用文献数
- 1
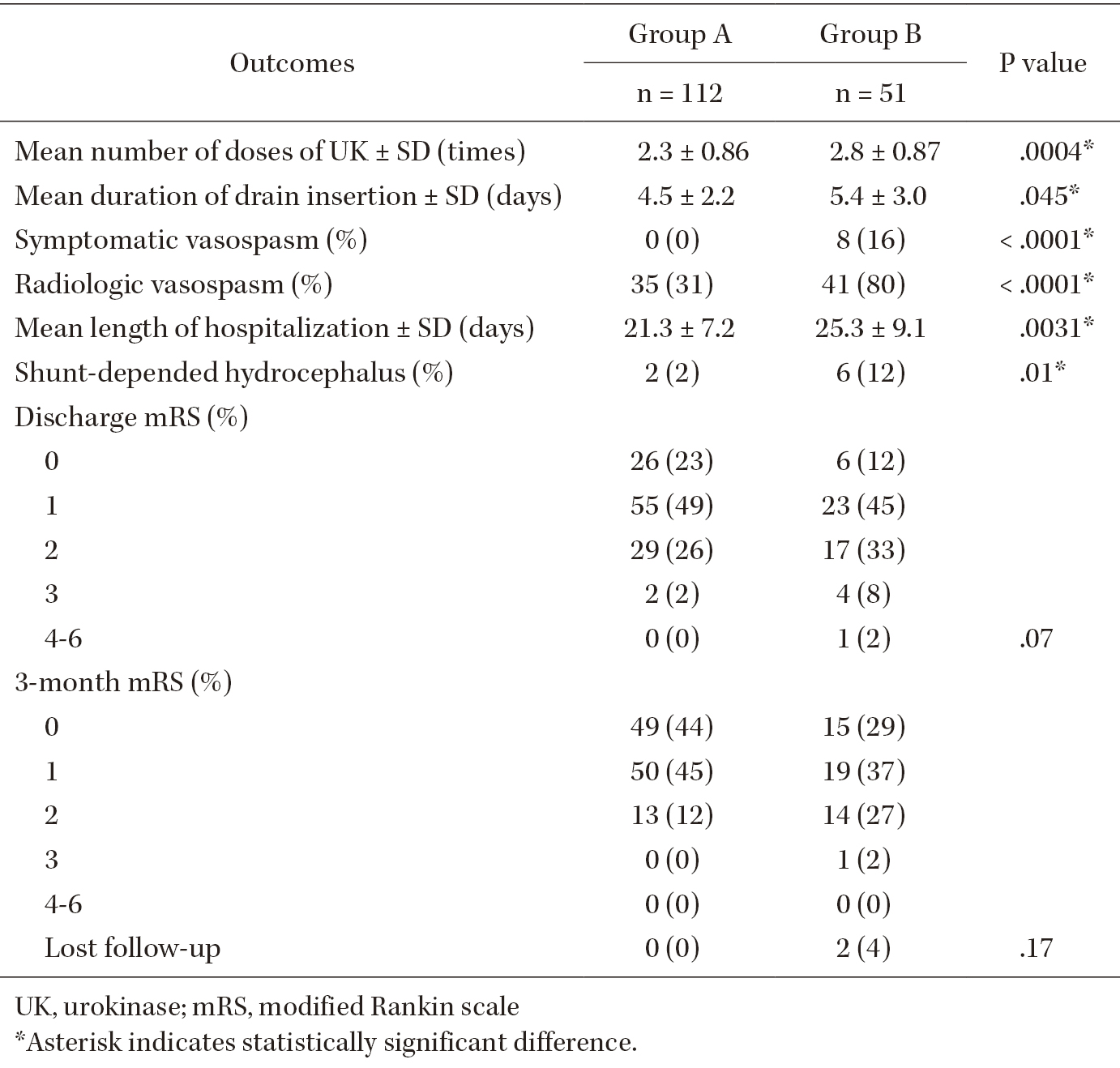
Delayed cerebral vasospasms after subarachnoid hemorrhage (SAH) are a risk factor for poor prognosis after successful treatment of ruptured intracranial aneurysms. Different strategies to remove clots from the subarachnoid space and prevent vasospasms have different outcomes. Intrathecal urokinase infusion therapy combined with endovascular treatment (EVT) can reduce the incidence of symptomatic vasospasms. To analyze the relationship between symptomatic vasospasms and residual SAHs after urokinase infusion therapy, we retrospectively reviewed the records of 348 consecutive patients managed with EVT and intrathecal urokinase infusion therapy for aneurysmal SAH at our institution between 2010 and 2021. Among them, 163 patients met the study criteria and were classified into two groups according to the presence of residual SAH in the cisterns, Sylvian fissures, and frontal interhemispheric fissure. The incidence of symptomatic vasospasms and the clinical outcomes were assessed. In total, eight (5.0%) patients developed symptomatic vasospasms. Patients with symptomatic vasospasms had a significantly higher incidence of residual SAH in the Sylvian or frontal interhemispheric fissures than those without (P <.0001). No patient with SAHs resolved by urokinase infusion therapy developed symptomatic vasospasms. However, the two groups did not differ significantly in terms of modified Rankin scale scores at discharge. Treatment with intrathecal urokinase infusion after EVT for aneurysmal SAH can substantially reduce the risk of clinically evident vasospasms.
1 0 0 0 OA Ventriculo-atrial Conduction in Patients with Normal and Impaired Atrio-ventricular Conduction
- 著者
- Tomoo INOUE Katsuya KOBAYASHI Hisashi FUKUZAKI
- 出版者
- International Heart Journal Association
- 雑誌
- Japanese Heart Journal (ISSN:00214868)
- 巻号頁・発行日
- vol.26, no.5, pp.707-714, 1985 (Released:2008-12-09)
- 参考文献数
- 16
- 被引用文献数
- 4 4
Ventriculo-atrial (VA) conduction was studied in 133 patients with various kinds of arrhythmias using intracardiac electrograms and programmed stimulation. One-to-one V A conduction was observed during RV pacing at the rate just above the sinus rate in 6 of 31 patients (19.4%) with advanced AV block, in 7 of 26 patients (26.9%) with impaired AV nodal conduction, in 25 of 71 patients (35.2%) with normal AV nodal conduction and 3 of 5 patients (60%) with enhanced AV nodal conduction. However, the differences between these groups were not significant. There was no significant difference in either the AH block rate during RA pacing or the antegrade functional refractory period (FRP) of the AV node in patients with or without VA conduction, and the VA block rate during RV pacing was not significantly correlated with the AH block rate or the FRP of the AV node. VA conduction time (S-HRA) also showed no significant differences between these groups. The mean. VA conduction time during RV pacing at rates of 60 to 80 bpm was 208±87 msec, ranging from 100 to 395 msec. In conclusion, AV conduction disturbances may influence VA conduction, but VA conduction cannot be predicted from antegrade conductivity.