- 著者
- Yoshitaka NAGASHIMA Yusuke NISHIMURA Tokumi KANEMURA Nobuhiro HATA Kotaro SATAKE Sho AKAHORI Motonori ISHII Takafumi TANEI Masakazu TAKAYASU Ryuta SAITO
- 出版者
- The Japan Neurosurgical Society
- 雑誌
- Neurologia medico-chirurgica (ISSN:04708105)
- 巻号頁・発行日
- pp.2023-0064, (Released:2023-10-18)
- 参考文献数
- 31
There is a lack of agreement on whether minimally invasive lateral lumbar intervertebral fusion (LLIF) is a suitable treatment option for vertebral fragility fractures (VFFs). Hence, we sought to evaluate the efficacy and safety of LLIF in the management of VFF with neurological deficits in the lumbar spine. Between April 2015 and March 2020, we conducted a retrospective observational study of patients with VFF treated with three-level or less LLIF. The participants had previously received conservative treatment but had not been able to control their neurological symptoms. To assess the outcomes of the LLIF procedures, the patients were followed up for a minimum of 1 year. Clinical and radiological results, which include the timing and location of the bony fusion, were analyzed. The study involved 19 patients with 23 vertebral fracture levels. The residual height of the fractured vertebra was found to be 57.0 ± 12.3% of the height of the adjacent level. The mean Japanese Orthopedic Association score significantly improved postoperatively. Postoperative radiological parameters were significantly maintained at 1 year, and lumbar lordosis was maintained at the last follow-up (45.0 ± 26.7). In total 31 LLIF levels, bone fusion was observed in four levels at 6 months postoperatively, in 16 levels at 1 year, and in 23 levels at the last follow-up. The facet joint had the highest bony fusion location. LLIF within three levels can be safely performed in certain VFF cases with sufficient residual vertebral height.
- 著者
- Kotaro Satake Tokumi Kanemura Hiroaki Nakashima Hidetoshi Yamaguchi Naoki Segi Jun Ouchida
- 出版者
- The Japanese Society for Spine Surgery and Related Research
- 雑誌
- Spine Surgery and Related Research (ISSN:2432261X)
- 巻号頁・発行日
- vol.1, no.4, pp.203-210, 2017-10-20 (Released:2017-11-27)
- 参考文献数
- 23
- 被引用文献数
- 27 32
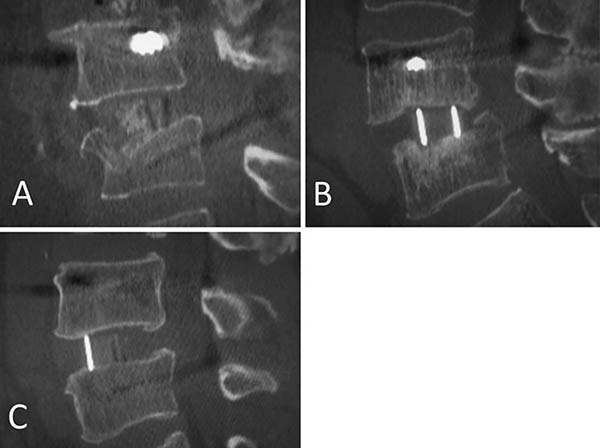
Introduction: Few studies have investigated the influence of cage subsidence patterns (intraoperative endplate injury or late-onset cage settling) on bony fusion and clinical outcomes in lateral interbody fusion (LIF). This retrospective study was performed to compare the fusion rate and clinical outcomes of cage subsidence patterns in LIF at one year after surgery.Methods: Participants included 93 patients (aged 69.0±0.8 years; 184 segments) who underwent LIF with bilateral pedicle screw fixation. All segments were evaluated by computed tomography and classified into three groups: Segment E (intraoperative endplate injury, identified immediately postoperatively); Segment S (late-onset settling, identified at 3 months or later); or Segment N (no subsidence). We compared patient characteristics, surgical parameters and fusion status at 1 year for the three subsidence groups. Patients were classified into four groups: Group E (at least one Segment E), Group S (at least one Segment S), Group ES (both Segments E and S), or Group N (Segment N alone). Visual analog scales (VASs) and the Japanese Orthopedic Association Back Pain Evaluation Questionnaire (JOABPEQ) were compared for the four patient groups.Results: 184 segments were classified: 31 as Segment E (16.8%), 21 as Segment S (11.4%), and 132 as Segment N (71.7%). Segment E demonstrated significantly lower bone mineral density (-1.7 SD of T-score, p=0.003). Segment S demonstrated a significantly higher rate of polyetheretherketone (PEEK) cages (100%, p=0.03) and a significantly lower fusion rate (23.8%, p=0.01). There were no significant differences in VAS or in any of the JOABPEQ domains among the four patient groups.Conclusions: Intraoperative endplate injury was significantly related to bone quality, and late-onset settling was related to PEEK cages. Late-onset settling demonstrated a worse fusion rate. However, there were no significant differences in clinical outcomes among the subsidence patterns.