- 著者
- Yoshitaka NAGASHIMA Yusuke NISHIMURA Tokumi KANEMURA Nobuhiro HATA Kotaro SATAKE Sho AKAHORI Motonori ISHII Takafumi TANEI Masakazu TAKAYASU Ryuta SAITO
- 出版者
- The Japan Neurosurgical Society
- 雑誌
- Neurologia medico-chirurgica (ISSN:04708105)
- 巻号頁・発行日
- pp.2023-0064, (Released:2023-10-18)
- 参考文献数
- 31
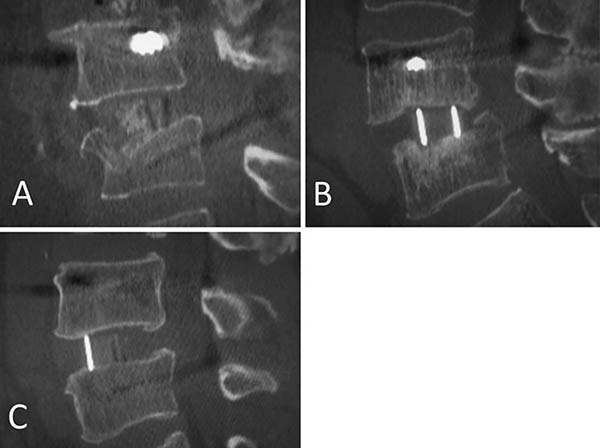
There is a lack of agreement on whether minimally invasive lateral lumbar intervertebral fusion (LLIF) is a suitable treatment option for vertebral fragility fractures (VFFs). Hence, we sought to evaluate the efficacy and safety of LLIF in the management of VFF with neurological deficits in the lumbar spine. Between April 2015 and March 2020, we conducted a retrospective observational study of patients with VFF treated with three-level or less LLIF. The participants had previously received conservative treatment but had not been able to control their neurological symptoms. To assess the outcomes of the LLIF procedures, the patients were followed up for a minimum of 1 year. Clinical and radiological results, which include the timing and location of the bony fusion, were analyzed. The study involved 19 patients with 23 vertebral fracture levels. The residual height of the fractured vertebra was found to be 57.0 ± 12.3% of the height of the adjacent level. The mean Japanese Orthopedic Association score significantly improved postoperatively. Postoperative radiological parameters were significantly maintained at 1 year, and lumbar lordosis was maintained at the last follow-up (45.0 ± 26.7). In total 31 LLIF levels, bone fusion was observed in four levels at 6 months postoperatively, in 16 levels at 1 year, and in 23 levels at the last follow-up. The facet joint had the highest bony fusion location. LLIF within three levels can be safely performed in certain VFF cases with sufficient residual vertebral height.
- 著者
- Kotaro Satake Tokumi Kanemura Hiroaki Nakashima Hidetoshi Yamaguchi Naoki Segi Jun Ouchida
- 出版者
- The Japanese Society for Spine Surgery and Related Research
- 雑誌
- Spine Surgery and Related Research (ISSN:2432261X)
- 巻号頁・発行日
- vol.1, no.4, pp.203-210, 2017-10-20 (Released:2017-11-27)
- 参考文献数
- 23
- 被引用文献数
- 27 32
Introduction: Few studies have investigated the influence of cage subsidence patterns (intraoperative endplate injury or late-onset cage settling) on bony fusion and clinical outcomes in lateral interbody fusion (LIF). This retrospective study was performed to compare the fusion rate and clinical outcomes of cage subsidence patterns in LIF at one year after surgery.Methods: Participants included 93 patients (aged 69.0±0.8 years; 184 segments) who underwent LIF with bilateral pedicle screw fixation. All segments were evaluated by computed tomography and classified into three groups: Segment E (intraoperative endplate injury, identified immediately postoperatively); Segment S (late-onset settling, identified at 3 months or later); or Segment N (no subsidence). We compared patient characteristics, surgical parameters and fusion status at 1 year for the three subsidence groups. Patients were classified into four groups: Group E (at least one Segment E), Group S (at least one Segment S), Group ES (both Segments E and S), or Group N (Segment N alone). Visual analog scales (VASs) and the Japanese Orthopedic Association Back Pain Evaluation Questionnaire (JOABPEQ) were compared for the four patient groups.Results: 184 segments were classified: 31 as Segment E (16.8%), 21 as Segment S (11.4%), and 132 as Segment N (71.7%). Segment E demonstrated significantly lower bone mineral density (-1.7 SD of T-score, p=0.003). Segment S demonstrated a significantly higher rate of polyetheretherketone (PEEK) cages (100%, p=0.03) and a significantly lower fusion rate (23.8%, p=0.01). There were no significant differences in VAS or in any of the JOABPEQ domains among the four patient groups.Conclusions: Intraoperative endplate injury was significantly related to bone quality, and late-onset settling was related to PEEK cages. Late-onset settling demonstrated a worse fusion rate. However, there were no significant differences in clinical outcomes among the subsidence patterns.
- 著者
- Satoshi YOSHIKAWA Yusuke NISHIMURA Yoshitaka NAGASHIMA Hiroshi ITO Takahiro OYAMA Tomoya NISHII Tomomi GONDA Hiroshi RYU Kei NOMURA Masahito HARA Masakazu TAKAYASU Howard J GINSBERG Tokumi KANEMURA Ryuta SAITO
- 出版者
- The Japan Neurosurgical Society
- 雑誌
- Neurologia medico-chirurgica (ISSN:04708105)
- 巻号頁・発行日
- pp.2021-0390, (Released:2023-03-01)
- 参考文献数
- 28
The goal of this study is to perform correlation analysis of Computed tomography (CT) and magnetic resonance imaging (MRI) results in posterior ligament complex (PLC) injury and define the morphological traits of thoracolumbar (TL) burst fractures connected to PLC injury. Forty patients with surgically repaired TL burst fractures between January 2013 and December 2020 were retrospectively analyzed. The patients were split into two groups for comparison based on MRI (Group P: patients with a confirmed or suspected PLC injury; Group N: patients with PLC injury denied). The radiographic morphological examination based on CT scans and clinical evaluation was performed and compared between two groups. The thoracolumbar injury classification and severity score (TLICS), the load sharing classification (LSC) scores, and the number of patients with neurological impairments were considerably greater in Group P. Loss of height of the fracture (loss height), local kyphosis of the fracture (local kyphosis), and supraspinous distance were significantly higher in Group P and significantly associated with PLC injuries indicating severe vertebral body destruction and traumatic kyphosis in multivariate logistic analysis [odds ratio: 1.90, 1.06, and 1.13, respectively]. Cutoff value for local kyphosis obtained from the receiver operating characteristic curve was 18.8. If local kyphosis is greater than 18.8 degrees on CT scans, we should take into account the probability of the highly damaged burst fracture associated with PLC injury. In this situation, we should carefully assess MRI to identify the spinal cord injury or spinal cord compression in addition to PLC injury because these instances likely present with neurological abnormalities.
- 著者
- Mitsuru Yagi Nobuyuki Fujita Tomohiko Hasegawa Gen Inoue Yoshihisa Kotani Seiji Ohtori Sumihisa Orita Yasushi Oshima Daisuke Sakai Toshinori Sakai Hiroshi Taneichi Daisuke Togawa Kazuo Nakanishi Hiroaki Nakashima Toshitaka Yoshii Masaya Nakamura Motoki Iwasaki Masahiko Watanabe Hirotaka Haro Tokumi Kanemura Naobumi Hosogane New Technology Assessment Committee of The Japanese Society for Spine Surgery and Related Research
- 出版者
- The Japanese Society for Spine Surgery and Related Research
- 雑誌
- Spine Surgery and Related Research (ISSN:2432261X)
- 巻号頁・発行日
- pp.2022-0194, (Released:2022-12-12)
- 被引用文献数
- 1
IntroductionLateral lumbar interbody fusion (LLIF) has been introduced in Japan in 2013. Despite the effectiveness of this procedure, several considerable complications have been reported. This study reported the results of a nationwide survey performed by the Japanese Society for Spine Surgery and Related Research (JSSR) on the complications associated with LLIF performed in Japan.MethodsJSSR members conducted a web-based survey following LLIF between 2015 and 2020. Any complications meeting the following criteria were included: (1) major vessel, (2) urinary tract, (3) renal, (4) visceral organ, (5) lung, (6) vertebral, (7) nerve, and (8) anterior longitudinal ligament injury; (9) weakness of psoas; (10) motor and (11) sensory deficit; (12) surgical site infection; and (13) other complications. The complications were analyzed in all LLIF patients, and the differences in incidence and type of complications between the transpsoas (TP) and prepsoas (PP) approaches were compared.ResultsAmong the 13,245 LLIF patients (TP 6,198 patients [47%] and PP 7,047 patients [53%]), 389 complications occurred in 366 (2.76%) patients. The most common complication was sensory deficit (0.5%), followed by motor deficit (0.43%) and weakness of psoas muscle (0.22%). Among the patient cohort, 100 patients (0.74%) required revision surgery during the survey period. Almost half of the complications developed in patients with spinal deformity (183 patients [47.0%]). Four patients (0.03%) died from complications. Statistically more frequent complications occurred in the TP approach than in the PP approach (TP vs. PP, 220 patients [3.55%] vs. 169 patients [2.40%]; p < 0.001).ConclusionsThe overall complication rate was 2.76%, and 0.74% of the patients required revision surgery because of complications. Four patients died from complications. LLIF may be beneficial for degenerative lumbar conditions with acceptable complications; however, the indication for spinal deformity should be carefully determined by the experience of the surgeon and the extent of the deformity.