- 著者
- Kento TAKAHARA Satoshi TAKAHASHI Utaro HINO Takashi HORIGUCHI Masahiro TODA
- 出版者
- The Japan Neurosurgical Society
- 雑誌
- NMC Case Report Journal (ISSN:21884226)
- 巻号頁・発行日
- vol.9, pp.377-382, 2022-12-31 (Released:2022-11-09)
- 参考文献数
- 19
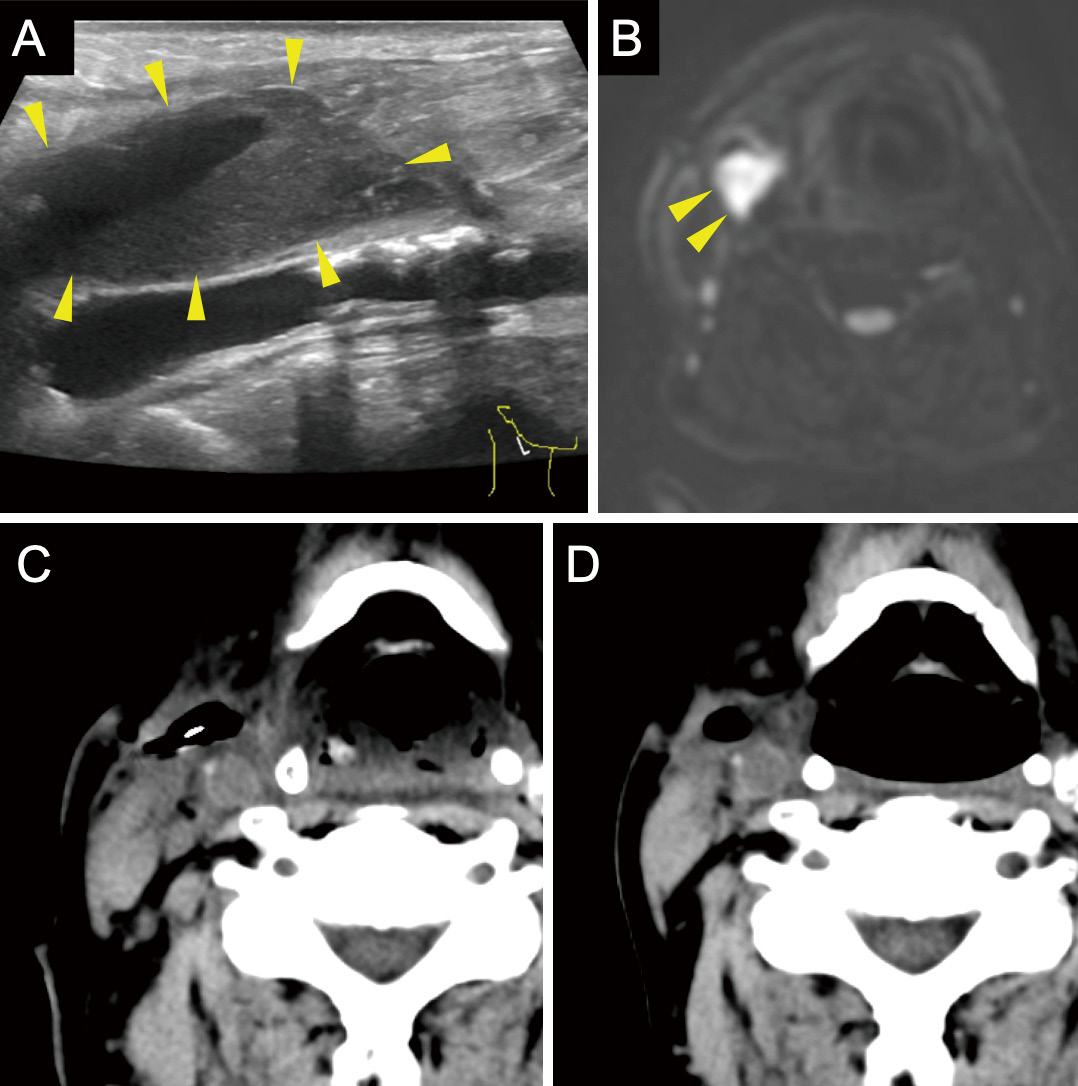
Carotid endarterectomy (CEA) and carotid artery stenting (CAS) for internal carotid artery (ICA) stenosis have specific risks. Therefore, the accurate evaluation and management of each risk factor are important, especially for patients who are at high risk for both CEA and CAS.We report the case of a 77-year-old man with right ICA stenosis that progressed despite optimal medical treatment. In addition, he had several risk factors for both CEA and CAS, including previous cervical radiation therapy, contralateral ICA occlusion, chronic kidney insufficiency, and severe aortic valve stenosis. CEA was performed with priority given to aortic valve stenosis without complications, and the patient was discharged 10 days postoperatively, without neurological sequelae. However, a pericarotid cervical abscess was detected by carotid echo, computed tomography (CT), and magnetic resonance imaging (MRI) 1 month after CEA that required surgical drainage. The infection was thought to be odontogenic because the pathogen was identified as normal oral bacterial flora, and a wound infection was not apparent. Teeth extraction and abscess drainage, in combination with antibiotic therapy, successfully cured the infection without additional complications.Odontogenic cervical abscesses after CEA can occur, especially if the patient is at risk of infection. Therefore, both preoperative and postoperative dental evaluation and management are recommended. As in this case, a cervical abscess can occur without wound infection, and the abscess diagnosis is sometimes difficult from wound inspection alone. Cervical echocardiogram and CT were useful for detecting fluid collection, whereas MRI was useful for qualitatively evaluating the lesion.
- 著者
- Yuta Horikoshi Tetsu Kimura Toshiaki Nishikawa Takashi Horiguchi Koji Sato Masahiko Ohbuchi
- 出版者
- 日本蘇生学会
- 雑誌
- 蘇生 (ISSN:02884348)
- 巻号頁・発行日
- vol.34, no.1, pp.14-21, 2015-04-14 (Released:2015-05-21)
- 参考文献数
- 31
Background:Both dexmedetomidine and hypothermia are known to reduce brain injury following ischemia. We examined whether a combination of dexmedetomidine and hypothermia reduce brain injury after asphyxial cardiac arrest in rats to a greater extent than either treatment. Methods:Male SD rats were assigned to one of four groups(n = 7 each);control (C, saline and temporal muscle temperature 37.5℃), dexmedetomidine (D, dexmedetomidine 10μg/kg and 37.5℃), hypothermia (H, saline and 35.0℃), and dexmedetomidine - hypothermia (DH, dexmedetomidine 10μg/kg and 35.0℃). Dexmedetomidine or saline was administered intraperitoneally 30 min before insult. Predetermined temperature was maintained from 30 min before asphyxia until 60 min after resuscitation. Cerebral ischemia was induced with asphyxia of 5 min, resulting in cardiac arrest of about 2 min. Rats were resuscitated by chest compression and intravenous epinephrine. Neurological score was assessed at 24, 48, and 72 hours after insult, and brain was fixed and stained with hematoxylin and eosin. Results:Neurological scores were greater in groups H and DH than groups C and D at 24 hours after insult (P < 0.05), whereas they were similar at 48 and 72 hours. Percentages of intact neurons in hippocampal CA1 were greater in groups D, H, and DH than group C (P < 0.05). Conclusions:Dexmedetomidine and hypothermia improved histologic outcome compared with the control group after asphyxial cardiac arrest, whereas the combination of dexmedetomidine and hypothermia provided comparable neuroprotection with either of two therapies alone.