- 著者
- Madoka NAKAJIMA Shigeki YAMADA Masakazu MIYAJIMA Kazunari ISHII Nagato KURIYAMA Hiroaki KAZUI Hideki KANEMOTO Takashi SUEHIRO Kenji YOSHIYAMA Masahiro KAMEDA Yoshinaga KAJIMOTO Mitsuhito MASE Hisayuki MURAI Daisuke KITA Teruo KIMURA Naoyuki SAMEJIMA Takahiko TOKUDA Mitsunobu KAIJIMA Chihiro AKIBA Kaito KAWAMURA Masamichi ATSUCHI Yoshihumi HIRATA Mitsunori MATSUMAE Makoto SASAKI Fumio YAMASHITA Shigeki AOKI Ryusuke IRIE Hiroji MIYAKE Takeo KATO Etsuro MORI Masatsune ISHIKAWA Isao DATE Hajime ARAI The research committee of idiopathic normal pressure hydrocephalus
- 出版者
- The Japan Neurosurgical Society
- 雑誌
- Neurologia medico-chirurgica (ISSN:04708105)
- 巻号頁・発行日
- vol.61, no.2, pp.63-97, 2021 (Released:2021-02-15)
- 参考文献数
- 286
- 被引用文献数
- 88 211
Among the various disorders that manifest with gait disturbance, cognitive impairment, and urinary incontinence in the elderly population, idiopathic normal pressure hydrocephalus (iNPH) is becoming of great importance. The first edition of these guidelines for management of iNPH was published in 2004, and the second edition in 2012, to provide a series of timely, evidence-based recommendations related to iNPH. Since the last edition, clinical awareness of iNPH has risen dramatically, and clinical and basic research efforts on iNPH have increased significantly. This third edition of the guidelines was made to share these ideas with the international community and to promote international research on iNPH. The revision of the guidelines was undertaken by a multidisciplinary expert working group of the Japanese Society of Normal Pressure Hydrocephalus in conjunction with the Japanese Ministry of Health, Labour and Welfare research project. This revision proposes a new classification for NPH. The category of iNPH is clearly distinguished from NPH with congenital/developmental and acquired etiologies. Additionally, the essential role of disproportionately enlarged subarachnoid-space hydrocephalus (DESH) in the imaging diagnosis and decision for further management of iNPH is discussed in this edition. We created an algorithm for diagnosis and decision for shunt management. Diagnosis by biomarkers that distinguish prognosis has been also initiated. Therefore, diagnosis and treatment of iNPH have entered a new phase. We hope that this third edition of the guidelines will help patients, their families, and healthcare professionals involved in treating iNPH.
- 著者
- Nobuyuki MITSUI Manabu KINOSHITA Junji NAKAZAWA Hirokazu OZAKI Teruo KIMURA
- 出版者
- The Japan Neurosurgical Society
- 雑誌
- NMC Case Report Journal (ISSN:21884226)
- 巻号頁・発行日
- vol.10, pp.279-283, 2023-12-31 (Released:2023-10-14)
- 参考文献数
- 12
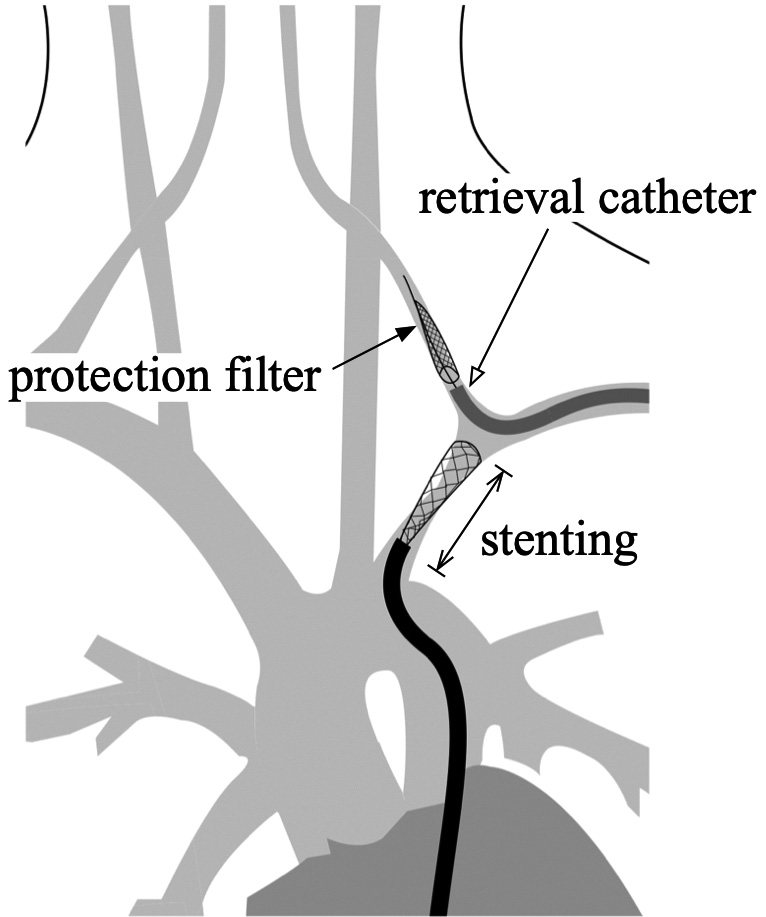
Endovascular treatment is a standard procedure for subclavian artery stenosis or obstruction. However, great care should be taken to avoid embolic complications to the vertebral artery, and several methods have previously been reported. Hence, as surgical procedures become increasingly complicated, unintended issues may arise during treatment. Here, the authors report a case where the filter-type protection device was caught in the stent because the patient moved during treatment, leading to open surgery to recover the filter-type protection device. A 78-year-old female suffering from a left subclavian steal syndrome underwent stenting due to subclavian artery stenosis. The stenotic lesion was approached via the transfemoral route, and a filter-type protection device was advanced to the vertebral artery via the transbrachial route to prevent embolic complications. As the procedure was performed under local anesthesia, the patient moved during stent deployment proximally to the left vertebral artery origin, and the stent unintentionally advanced distally, covering the vertebral artery and obstructing the retrieval catheter for the filter-type protection device to advance. Failed attempts in recovering the filter-type protection device required open surgery for retrieval. Fortunately, there was no postoperative neurological and radiographic complication, ameliorating her chief complaint. The retriever catheter for the protection device should be advanced beyond the vertebral artery orifice just proximal to the protection device before stenting to avoid such complications while also thoroughly considering the type of anesthesia during treatment.