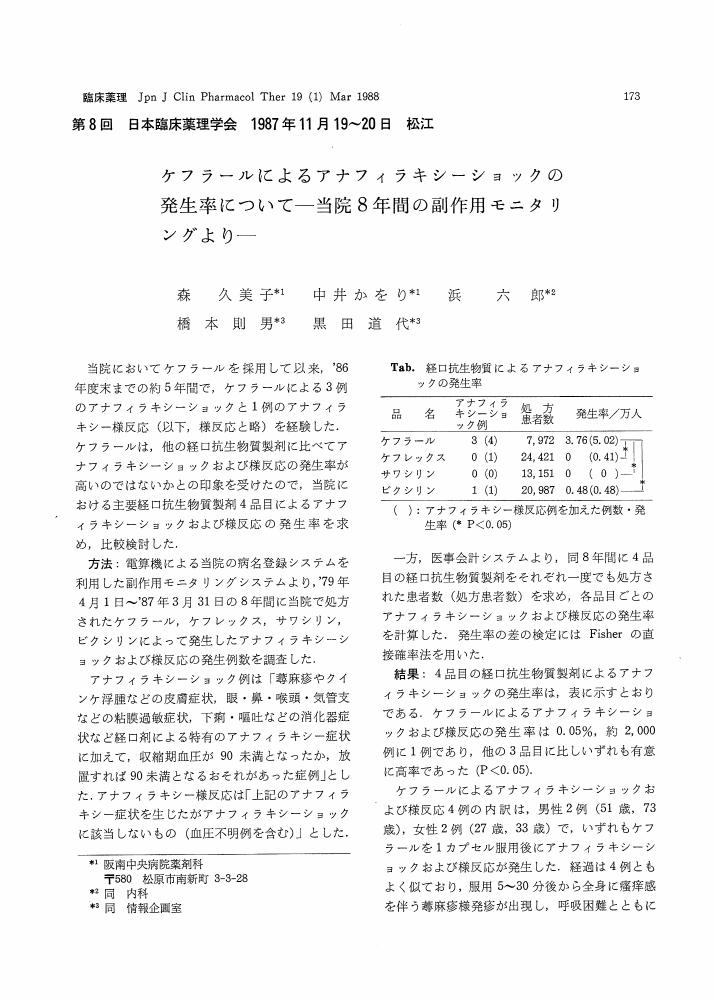
3 0 0 0 OA ケフラールによるアナフィラキシーショックの発生率について
- 著者
- 森 久美子 中井 かをり 浜 六郎 橋本 則男 黒田 道代
- 出版者
- 一般社団法人 日本臨床薬理学会
- 雑誌
- 臨床薬理 (ISSN:03881601)
- 巻号頁・発行日
- vol.19, no.1, pp.173-174, 1988-03-31 (Released:2010-06-28)
- 参考文献数
- 2
2 0 0 0 OA 糖尿病者にスタチンは禁忌―緊急提言
- 著者
- 奥山 治美 浜崎 智仁 大櫛 陽一 浜 六郎 内野 元 渡邊 浩幸 橋本 道男
- 出版者
- 日本脂質栄養学会
- 雑誌
- 脂質栄養学 (ISSN:13434594)
- 巻号頁・発行日
- vol.22, no.2, pp.173-186, 2013 (Released:2013-10-01)
- 参考文献数
- 60
- 被引用文献数
- 1 1
Statins have been recognized clinically to raise blood glucose and glycated protein (HbA1c) levels enhancing the development of insulin resistance. However, most clinicians appear to adopt the interpretation that the benefit (prevention of CHD) outweighs the risk (new-onset of diabetes mellitus). Consistently, "Japan Atherosclerosis Society Guidelines for the Prevention of Atherosclerotic Cardiovascular Diseases 2012" recommends diabetics to maintain LDL-C levels below 120 mg/dL; 40 mg/dL lower than the value for those without risky complications. This recommendation necessitates many diabetics to use statins. However, we pointed out that statins exhibited no significant benefit for the prevention of CHD in the trials performed by scientists independent of industries after 2004, when a new regulation on clinical trials took effect in EU (Cholesterol Guidelines for Longevity, 2010). Here, we reviewed clinical evidence that statins could induce diabetes mellitus, and biochemical evidence that statins are toxic to mitochondria; they suppress electron transport and ATP generation through decreased prenyl-intermediate levels. They also inhibit seleno-protein synthesis and dolichol-mediated glycation of insulin receptor leading to insulin resistance and cardiac failure, similarly to the case of Se-deficiency. These mechanisms of statin actions are consistent with clinically observed decreases in blood ketone body, mitochondrial dysfunctions and enhanced glucose intolerance. Based on these lines of evidence, we urgently propose that statins are contraindicant to diabetics and their prescription should be restricted to special cases* for which medical doctors rationally decide to be necessary.
- 著者
- 浜崎 智仁 奥山 治美 浜 六郎 大櫛 陽一
- 出版者
- 日本脂質栄養学会
- 雑誌
- 脂質栄養学 (ISSN:13434594)
- 巻号頁・発行日
- vol.23, no.1, pp.71-78, 2014 (Released:2014-05-01)
- 参考文献数
- 8
- 被引用文献数
- 1
The risk chart of NIPPON DATA80 showing the absolute mortality from coronary heart disease (CHD) is the only chart of this type widely used in the medical field in Japan. In this chart, there are 240 frames for men with casual blood glucose of ≥200 mg/dL (the right side of the chart); these frames are separated according to smoking status, age, systolic blood pressure, and total cholesterol. The absolute CHD mortality during 10 years in these 240 frames ranges from <0.5% to ≥10% (more than 20 times difference). However, we estimated that there were only 5 CHD deaths at most in these 240 diabetic frames during the study period of NIPPON DATA80. The left (non-diabetic; another 240 frames) part of the chart was adopted for the Guidelines by Japan Atherosclerosis Society after excluding 60 frames for those in their 70s (180 frames as a whole), but those 180 frames were estimated to have only 35 CHD deaths despite the risk difference being more than 10. Furthermore, statistical values such as p value and confidence interval were not found either in the paper introducing the risk chart or in the referred paper for methodology. We, therefore, could not statistically estimate appropriateness of the risk chart. In conclusion, the NIPPON DATA80 risk chart for CHD mortality is not suitable for guidelines or education.
1 0 0 0 OA 日本の薬剤疫学の課題を考える
- 著者
- 浜 六郎
- 出版者
- 一般社団法人 日本薬剤疫学会
- 雑誌
- 薬剤疫学 (ISSN:13420445)
- 巻号頁・発行日
- vol.1, no.2, pp.87-95, 1996-10-31 (Released:2011-02-28)
- 参考文献数
- 43
Objectives : To find the most important problems to be addressed by pharmacoepidemiology in Japan. My view presented in this article is personal conceived after having witnessed several drug-induced disasters (e.g., the SMON affair in 1970 and the Sorivudine case in 1993) and carried out a number of epidemiological studies while practicing as an internist.Methods : Preventive measures taken after having experienced major drug-induced disasters as well as the relationship between these measures and pharmacoepidemiology are compared between the foreign developed countries and Japan. The comparison is conducted based on my belief that pharmacoepidemiology must examine the major epidemic drug-related diseases, and find and verify the effective measures to prevent them.Results and Conclusion : It is found that in the USA and England, the drug-induced disasters have led the following effective countermeasures : revising the methods of approval of new drugs including the introduction of licensing for clinical trials of investigational products and improving postmarketingsurveillance according to the concept of “event monitoring”. Pharmacoepidemiology has been developed in association with those reforms. On the contrary, many measures posed after the drug disasters seen to have not worked well in Japan. Pharmacoepidemiology in Japan should have a more active role in (1) planning the measures to prevent drug disasters, (2) monitoring the methods and individual processes of approval of new drugs, (3) evaluating the investigational products particularly with respect to the safety (toxicity), and (4) carrying out orthodox pharmacoepidemiology researches including drug utilization studies, case-control studies, prescription-event monitoring, long term randomized controlled studies, pharmacoeconomic studies and so on.
- 著者
- 浜崎 智仁 奥山 治美 大櫛 陽一 浜 六郎
- 出版者
- 日本脂質栄養学会
- 雑誌
- 脂質栄養学 (ISSN:13434594)
- 巻号頁・発行日
- vol.22, no.1, pp.69-76, 2013 (Released:2013-05-01)
On September 8, 2012, the panel discussion “The Rethinking of Cholesterol Issues” was held in Sagamihara City, Japan. This paper is the summary of that panel discussion. Four discussants expressed their skeptical views against the cholesterol hypothesis. The whole discussion will be freely seen on the net. Also a similar editorial written by the four discussants will be published in English (Ann Nutr Metab 2013;62:32-36, a free PDF file is already available on the internet). Because Japan Atherosclerosis Society Guidelines for Prevention of Atherosclerotic Cardiovascular Diseases 2012 (JASG 2012) has recently been published, the main part of this paper is focused on serious flaws found in JASG 2012. Dr Harumi Okuyama discusses the differences between JASG 2012 and our guidelines indicating that high cholesterol levels are a good index of longevity; the most important point is that the statin trials that have been performed after 2004, when the new EU law regulating clinical trials became in effect, are all negative. Dr Yoichi Ogushi claims that JASG 2012 intentionally omits some good aspects of cholesterol; cholesterol is a negative risk factor of stroke. His own data also show that cholesterol is good for stroke. He also claims that to properly treat patients with diabetes, we need to reject the cholesterol hypothesis and to reduce carbohydrate rather than cholesterol. Dr Tomohito Hamazaki points out unforgivable flaws in JASG 2012. It does not disclose any COI. It does not contain any relationship between cholesterol levels and all-cause mortality in Japan. Pharmaceutical companies spend 600 billion yen (7 billion US$) per year for advertisement in Japan. This works as “devil’s insurance” (withdrawal of advertisement is a real threat to the mass media). The last discussant, Dr Rokuro Hama, explains the mistake made by JAS (liver disease causes both death and depression of cholesterol levels, and low cholesterol levels are not the cause of death). Hepatitis C virus (HCV) enters hepatic cells via LDL receptors, and low cholesterol levels are one of the major risk factors of HCV infection and chronic hepatitis. Hence, death from liver disease could be the result of low cholesterol levels.
1 0 0 0 OA 薬価の国際比較 薬剤別薬価比および数量重み付け薬価比
- 著者
- 浜 六郎 別府 宏圀 坂上 章子 森 久美子 坂口 啓子
- 出版者
- 一般社団法人 日本臨床薬理学会
- 雑誌
- 臨床薬理 (ISSN:03881601)
- 巻号頁・発行日
- vol.26, no.1, pp.385-386, 1995-03-31 (Released:2010-06-28)
- 被引用文献数
- 1 1
1 0 0 0 OA アニラセタム (サープル, ドラガノン) の効能・効果は証明されていない
- 著者
- 橋本 健太郎 林 敬次 柳 元和 梅田 忠斎 浜 六郎
- 出版者
- 一般社団法人 日本臨床薬理学会
- 雑誌
- 臨床薬理 (ISSN:03881601)
- 巻号頁・発行日
- vol.30, no.1, pp.199-200, 1999-01-31 (Released:2010-06-28)
- 参考文献数
- 4
- 著者
- 奥山 治美 浜 六郎 大櫛 陽一 浜崎 智仁 内野 元
- 出版者
- 日本脂質栄養学会
- 雑誌
- 脂質栄養学 (ISSN:13434594)
- 巻号頁・発行日
- vol.27, no.1, pp.30-38, 2018 (Released:2018-07-16)
An open-label, randomized controlled trial in type 2 diabetics with hypertension, dyslipidemia, or both was reported (J-DOIT3 study).The participants were randomly assigned to receive conventional or intensive therapy with respect to HbA1c, blood pressure and LDL-C (n=1,271 in each group),and were followed for 8.5 years at 81 clinical sites. Both the participants and doctors in charge were aware of the group assigned. The experimental design was essentially as recommended in the [Comprehensive risk management chart for the prevention of cerebro- and cardiovascular diseases 2015] from the Joint Committee consisted of 13 internal medicine-related societies in Japan, and the Japan Atherosclerotic Society Guidelines 2017. Therefore, the conclusion from the J-DOIT3 study is expected in medical field to affect the current and future medications for the prevention of atherosclerotic cerebro- and cardiovascular diseases (ASCVD).While analyzing the results of this study,we encountered serious problems associated with the methodology, logics and its interpretations, which were summarized in this review. The follow-up study appears to be in progress as described in the Discussion, but we interpret that the intensive therapy used in the J-DOIT3 study is risky in view of currently available evidence. We propose the authors of the study to let the participants know of the results on its objective endpoint, and newly obtain Informed Consents including the potential risks of the intensive intervention based on the progress in this field after the start of this study.
1 0 0 0 OA 糖尿病合併症予防研究(JDCS) ―その追加解析にもとづく批判的総説
- 著者
- 大櫛 陽一 浜 六郎 浜崎 智仁 内野 元
- 出版者
- 日本脂質栄養学会
- 雑誌
- 脂質栄養学 (ISSN:13434594)
- 巻号頁・発行日
- vol.27, no.1, pp.39-47, 2018 (Released:2018-07-16)
A nationwide multicenter randomized controlled study (JDCS) was performed in type-2 diabetes patients. The conventional (CON) group received usual care including anti-diabetic, anti-hypertensive and anti-hyperlipidemic agents to maintain their targeted levels, and the intervention (INT) group additionally received intensive education on lifestyle modifications and adherence to treatment by telephone counselling and at each time outpatient clinic visit for 8 years. The JDCS appears to be based on an assumption that usual treatment of diabetes is appropriate for the prevention of diabetes complications, and that the lack of patients’ compliance is the major cause of unsuccessful treatments. No significant differences between the two groups were found in most of the test results (BMI, blood pressure, fasting glucose level, TC, HDL, lipoprotein-a), use of agents, life style (energy intake, smoking and alcohol intake) at 4 years of intervention. The exercise level was higher at 5 years of intervention, and triglyceride level was lower at 8 years. The incidence of coronary heart disease, retinopathy and neuropathy did not differ significantly between the two groups, but stroke incidence was lower in the INT group. We conducted new analyses on the changes of some explanatory variables in each group. The proportion of participants with pharmacological treatment including insulin significantly increased in both groups except sulfonylureas which about 60% of the participants used at the baseline. On the other hand, those without pharmacological treatment decreased from 19% to 4% in both groups. These indicate that both groups failed in diabetes treatment together. As for the exercise and the smoking cessation, these may prevent stroke, but do not contribute to improvement of diabetes. It is not convincing enough for us to support the validity of publicizing the treatment of diabetes patients used in the JDCS study performed at 59 universities and general hospitals in Japan.
- 著者
- 橋本 健太郎 林 敬次 柳 元和 梅田 忠斎 浜 六郎
- 出版者
- The Japanese Society of Clinical Pharmacology and Therapeutics
- 雑誌
- 臨床薬理 (ISSN:03881601)
- 巻号頁・発行日
- vol.30, no.1, pp.199-200, 1999-01-31