- 著者
- Yuhei Ito Takao Kojima Toru Kobayashi Naoki Sato Yutaka Konno Keiko Oda Masazumi Fujii
- 出版者
- The Japanese Society for Neuroendovascular Therapy
- 雑誌
- Journal of Neuroendovascular Therapy (ISSN:18824072)
- 巻号頁・発行日
- pp.oa.2023-0005, (Released:2023-05-10)
- 参考文献数
- 10
Objective: Most large-vessel occlusions (LVOs) amenable to acute recanalization occur in the internal carotid or middle cerebral artery. However, few LVOs with a multivessel disease can be difficult to treat. This study aimed to determine the outcomes of mechanical thrombectomy in patients with both anterior and middle cerebral artery occlusions.Methods: We retrospectively collected data for patients who had undergone mechanical thrombectomy since January 2016 at Fukushima Medical University and its affiliated institutions (10 institutions). Patients with occluded vessels in the anterior and middle cerebral arteries were selected, and patient background, treatment course, and outcomes were reviewed.Results: A total of 341 mechanical thrombectomies were performed during the study period. Seven patients had occlusions involving both anterior and middle cerebral arteries. In these seven patients, the median time from onset to imaging, imaging to puncture, and puncture to recanalization was 106, 60, and 74 min, respectively. Only one patient (14%) had a modified Rankin Scale of 0–2 at 90 days.Conclusion: Comorbid anterior cerebral artery occlusion may worsen the outcome of patients with middle cerebral artery occlusion.
- 著者
- Satoshi MAESAWA Daisuke NAKATSUBO Masazumi FUJII Kentaro IIJIMA Sachiko KATO Tomotaka ISHIZAKI Masashi SHIBATA Toshihiko WAKABAYASHI
- 出版者
- The Japan Neurosurgical Society
- 雑誌
- Neurologia medico-chirurgica (ISSN:04708105)
- 巻号頁・発行日
- vol.58, no.10, pp.442-452, 2018 (Released:2018-10-15)
- 参考文献数
- 38
- 被引用文献数
- 5 18
Epilepsy surgery aims to control epilepsy by resecting the epileptogenic region while preserving function. In some patients with epileptogenic foci in and around functionally eloquent areas, awake surgery is implemented. We analyzed the surgical outcomes of such patients and discuss the clinical application of awake surgery for epilepsy. We examined five consecutive patients, in whom we performed lesionectomy for epilepsy with awake craniotomy, with postoperative follow-up > 2 years. All patients showed clear lesions on magnetic resonance imaging (MRI) in the right frontal (n = 1), left temporal (n = 1), and left parietal lobe (n = 3). Intraoperatively, under awake conditions, sensorimotor mapping was performed; primary motor and/or sensory areas were successfully identified in four cases, but not in one case of temporal craniotomy. Language mapping was performed in four cases, and language areas were identified in three cases. In one case with a left parietal arteriovenous malformation (AVM) scar, language centers were not identified, probably because of a functional shift. Electrocorticograms (ECoGs) were recorded in all cases, before and after resection. ECoG information changed surgical strategy during surgery in two of five cases. Postoperatively, no patient demonstrated neurological deterioration. Seizure disappeared in four of five cases (Engel class 1), but recurred after 2 years in the remaining patient due to tumor recurrence. Thus, for patients with epileptogenic foci in and around functionally eloquent areas, awake surgery allows maximal resection of the foci; intraoperative ECoG evaluation and functional mapping allow functional preservation. This leads to improved seizure control and functional outcomes.
- 著者
- Satoshi MAESAWA Epifanio BAGARINAO Masazumi FUJII Miyako FUTAMURA Toshihiko WAKABAYASHI
- 出版者
- 社団法人 日本脳神経外科学会
- 雑誌
- Neurologia medico-chirurgica (ISSN:04708105)
- 巻号頁・発行日
- pp.ra.2015-0302, (Released:2016-02-29)
- 参考文献数
- 81
- 被引用文献数
- 9
Cutting-edge neuroimaging technologies can facilitate preoperative evaluation in various neurosurgical settings. Surgery for gliomas and epilepsy requires precise localization for resection due to the need to preserve (or perhaps improve) higher cognitive functions. Accordingly, a hodological approach should be taken that considers subcortical networks as well as cortical functions within various functional domains. Resting state functional magnetic resonance imaging (fMRI) has the potential to provide new insights that are valuable for this approach. In this review, we describe recent developments in network analysis using resting state fMRI related to factors in glioma and epilepsy surgery: the identification of functionally dominant areas, evaluation of cognitive function by alteration of resting state networks (RSNs), glioma grading, and epileptic focus detection. One particular challenge that is close to realization is using fMRI for the identification of sensorimotor- and language-dominant areas during a task-free resting state. Various RSNs representative of the default mode network demonstrated at least some alterations in both patient groups, which correlated with behavioral changes including cognition, memory, and attention, and the development of psychosis. Still challenging is the detection of epileptic foci and propagation pathways when using only network analysis with resting state fMRI; however, a combined method with simultaneous electroencephalography has produced promising results. Consequently, network analysis is expected to continue to advance as neuroimaging technology improves in the next decade, and preoperative evaluation for neurosurgical parameters through these techniques should improve parallel with them.
- 著者
- Yuhei ITO Takao KOJIMA Takuya MAEDA Masazumi FUJII
- 出版者
- The Japan Neurosurgical Society
- 雑誌
- NMC Case Report Journal (ISSN:21884226)
- 巻号頁・発行日
- vol.10, pp.299-302, 2023-12-31 (Released:2023-10-14)
- 参考文献数
- 13
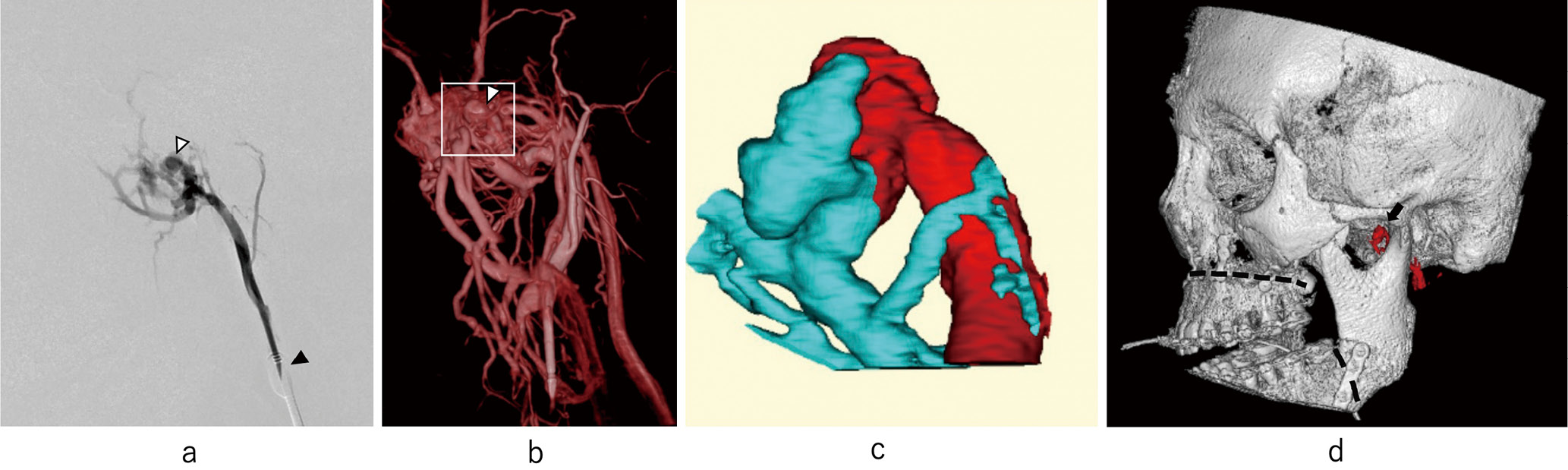
Le Fort I osteotomy is a common surgical technique for correcting jaw deformities. Although it is generally a safe procedure, there have been cases of postoperative vascular complications, which include arteriovenous fistulas. Published reports describe the development of arteriovenous fistulas that originate from the maxillary artery after this procedure; nevertheless, no cases of arteriovenous fistulas arising from the middle meningeal artery (MMA) have been reported. We present the case of a 19-year-old woman who developed pulsatile tinnitus immediately following a Le Fort I osteotomy. Angiography with proximal flow control of the external carotid artery showed an arteriovenous fistula between the extracranial portion of the MMA and the pterygoid venous plexus. The fistula was successfully treated using coil embolization, preserving the maxillary artery, which results in tinnitus resolution. In this report, the effectiveness of endovascular treatment for arteriovenous fistulas of the MMA that occur following a Le Fort I osteotomy was demonstrated. Angiography with proximal flow interruption was effective in shunt location detection.
- 著者
- Nobuo SUGO Sayaka TERAZONO Chie MATSUURA Yutaka FUCHINOUE Yuki SAKAEYAMA Mitsuyoshi ABE Masataka MIKAI Syuhei KUBOTA Kosuke KONDO Shoko SHIMOKAWA Taketoshi MAEHARA Hiroyoshi AKUTSU Fusao IKAWA Yukiko ENOMOTO Kazuko KAMIYA Satoshi KURODA Hideo TAKESHIMA Noriko TAMURA Tomohito HISHIKAWA Masazumi FUJII Takamitsu FUJIMAKI Tetsuyoshi HORIUCHI Junkoh YAMAMOTO Tetsuya YAMAMOTO Yoko KATO
- 出版者
- The Japan Neurosurgical Society
- 雑誌
- Neurologia medico-chirurgica (ISSN:04708105)
- 巻号頁・発行日
- pp.2023-0051, (Released:2023-07-25)
- 参考文献数
- 26
This study aims to evaluate the academic activities of female neurosurgeons at all branch meetings of the Japan Neurosurgical Society and identify related issues they encountered. The programs of all seven branch meetings of the Japan Neurosurgical Society (Hokkaido, Tohoku, Kanto, Chubu, Kinki, Chugoku/Shikoku, and Kyushu) were used to determine the number of presentations and chairpersons by sex. The covered period was from January 2008 to December 2020, which was available for viewing during the survey. Of note, only the Kinki branch used data from January 2008 to December 2019. The Neurologia Medico-chirurgica (NMC), the journal of the Japan Neurosurgical Society, was also reviewed to identify publication achievements during the same period. In all seven branches, the percentage of presentations given by female physicians increased from 7.9% in 2008 to 9.6% in 2020 (p < 0.05).Conversely, the percentage of female chairpersons in all branch meetings did not change over time and it was significantly lower (1.1%) than that of female presenters (7.9%) for all branch meetings combined in over 13 years (p < 0.01). In the NMC, the number of articles with female physicians as first authors did not increase or decrease over the years. We conclude that efforts to smoothly promote female neurosurgeons as chairpersons and increase the number of female first authors are necessary to facilitate their academic activities.
- 著者
- Masazumi FUJII Satoshi MAESAWA Sumio ISHIAI Kenichiro IWAMI Miyako FUTAMURA Kiyoshi SAITO
- 出版者
- The Japan Neurosurgical Society
- 雑誌
- Neurologia medico-chirurgica (ISSN:04708105)
- 巻号頁・発行日
- vol.56, no.7, pp.379-386, 2016 (Released:2016-07-15)
- 参考文献数
- 57
- 被引用文献数
- 24 41
The neural basis of language had been considered as a simple model consisting of the Broca’s area, the Wernicke’s area, and the arcuate fasciculus (AF) connecting the above two cortical areas. However, it has grown to a larger and more complex model based upon recent advancements in neuroscience such as precise imaging studies of aphasic patients, diffusion tensor imaging studies, functional magnetic resonance imaging studies, and electrophysiological studies with cortical and subcortical stimulation during awake surgery. In the present model, language is considered to be processed through two distinct pathways, the dorsal stream and the ventral stream. The core of the dorsal stream is the superior longitudinal fasciculus/AF, which is mainly associated with phonological processing. On the other hand, semantic processing is done mainly with the ventral stream consisting of the inferior fronto-occipital fasciculus and the intratemporal networks. The frontal aslant tract has recently been named the deep frontal tract connecting the supplementary motor area and the Broca’s area and it plays an important role in driving and initiating speech. It is necessary for every neurosurgeon to have basic knowledge of the neural basis of language. This knowledge is essential to plan safer surgery and preserve the above neural structures during surgery.