- 著者
- Koji Tamai Hidetomi Terai Akinobu Suzuki Hiroaki Nakamura Masaomi Yamashita Yawara Eguchi Shiro Imagama Kei Ando Kazuyoshi Kobayashi Morio Matsumoto Ken Ishii Tomohiro Hikata Shoji Seki Masaaki Aramomi Tetsuhiro Ishikawa Atsushi Kimura Hirokazu Inoue Gen Inoue Masayuki Miyagi Wataru Saito Kei Yamada Michio Hongo Kenji Endo Hidekazu Suzuki Atsushi Nakano Kazuyuki Watanabe Junichi Ohya Hirotaka Chikuda Yasuchika Aoki Masayuki Shimizu Toshimasa Futatsugi Keijiro Mukaiyama Masaichi Hasegawa Katsuhito Kiyasu Haku Iizuka Kotaro Nishida Kenichiro Kakutani Hideaki Nakajima Hideki Murakami Satoru Demura Satoshi Kato Katsuhito Yoshioka Takashi Namikawa Kei Watanabe Kazuyoshi Nakanishi Yukihiro Nakagawa Mitsunori Yoshimoto Hiroyasu Fujiwara Norihiro Nishida Masataka Sakane Masashi Yamazaki Takashi Kaito Takeo Furuya Sumihisa Orita Seiji Ohtori
- 出版者
- The Japanese Society for Spine Surgery and Related Research
- 雑誌
- Spine Surgery and Related Research (ISSN:2432261X)
- 巻号頁・発行日
- vol.1, no.4, pp.179-184, 2017-10-20 (Released:2017-11-27)
- 参考文献数
- 26
- 被引用文献数
- 3 3
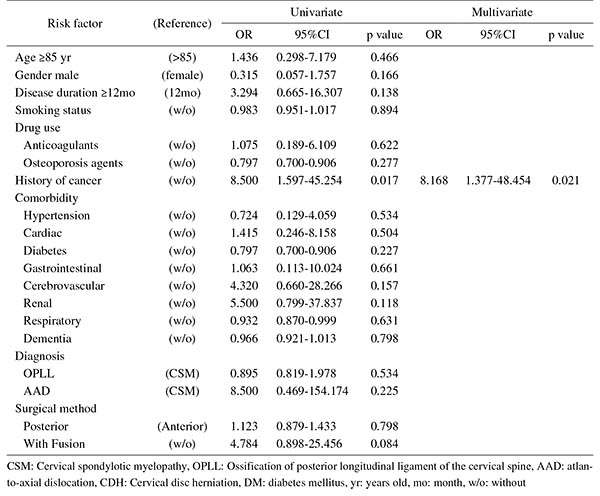
Introduction: With an aging population, the proportion of patients aged ≥80 years requiring cervical surgery is increasing. Surgeons are concerned with the high incidence of complications in this population, because "age" itself has been reported as a strong risk factor for complications. However, it is still unknown which factors represent higher risk among these elderly patients. Therefore, this study was conducted to identify the risk factors related to surgical complications specific to elderly patients by analyzing the registry data of patients aged ≥80 years who underwent cervical surgery.Methods: We retrospectively studied multicenter collected registry data using multivariate analysis. Sixty-six patients aged ≥80 years who underwent cervical surgery and were followed up for more than one year were included in this study. Preoperative patient demographic data, including comorbidities and postoperative complications, were collected from multicenter registry data. Complications were considered as major if they required invasive intervention, caused prolonged morbidity, or resulted in prolongation of hospital stay. Logistic regression analysis was performed to analyze the risk factors for complications. A p-value of <0.05 was considered as statistically significant.Results: The total number of patients with complications was 21 (31.8%), with seven major (10.6%) and 14 minor (21.2%) complications. Multivariate logistic regression analysis, after adjusting for age, revealed two significant risk factors: preoperative cerebrovascular disorders (OR, 6.337; p=0.043) for overall complications and cancer history (OR, 8.168; p=0.021) for major complications. Age, presence of diabetes mellitus, and diagnosis were not significant predictive factors for complications in this study.Conclusions: Preoperative cerebrovascular disorders and cancer history were risk factors for complications after cervical surgery in patients over 80 years old. Surgeons should pay attention to these specific risk factors before performing cervical surgery in elderly patients.
- 著者
- Tetsuya Tamaki Muneharu Ando Yukihiro Nakagawa Hiroshi Iwasaki Shunji Tsutsui Masanari Takami Hiroshi Yamada
- 出版者
- The Japanese Society for Spine Surgery and Related Research
- 雑誌
- Spine Surgery and Related Research (ISSN:2432261X)
- 巻号頁・発行日
- vol.5, no.3, pp.120-132, 2021-05-27 (Released:2021-05-27)
- 参考文献数
- 61
- 被引用文献数
- 6
An intraoperative functional spinal cord monitoring system is a technology used by spine and spinal cord surgeons to perform a safe surgery and to gain further surgical proficiency. However, no existing clinical neurophysiological method used in the operating room can monitor all complex spinal cord functions. Therefore, by observing the activities of certain neural action potentials transferred via limited neural tissues, surgeons need to deductively estimate the function of the whole spinal cord. Thus, as the number of spinal cord functions that need to be observed increases, spinal cord monitoring can be more reliable. However, in some situations, critical decision-making is affected by the limited capability of these methods. Nevertheless, good teamwork enables sharing of seamless information within the team composed of a surgeon, anesthesiologist, monitoring technician and nurses greatly contributes to making quick and accurate decisions. The surgeon, who is the person in charge of the team, should communicate with multidisciplinary team members using common technical terms. For this reason, spine and spinal cord surgeons must have appropriate knowledge of the methods currently used, especially of their utility and limitations. To date, at least six electrophysiological methods are available for clinical utilization: three are used to monitor sensory-related tracts, and three are used to monitor motor-related spinal cord functions. If surgeons perform electrode setting, utilizing their expertise, then the range of available methods is broadened, and more meticulous intraoperative functional spinal cord monitoring can be carried out. Furthermore, if the team members share information effectively by utilizing a clinically feasible judicious checklist or tools, then spinal cord monitoring will be more reliable.