- 著者
- Koji Tamai Hidetomi Terai Akinobu Suzuki Hiroaki Nakamura Masaomi Yamashita Yawara Eguchi Shiro Imagama Kei Ando Kazuyoshi Kobayashi Morio Matsumoto Ken Ishii Tomohiro Hikata Shoji Seki Masaaki Aramomi Tetsuhiro Ishikawa Atsushi Kimura Hirokazu Inoue Gen Inoue Masayuki Miyagi Wataru Saito Kei Yamada Michio Hongo Kenji Endo Hidekazu Suzuki Atsushi Nakano Kazuyuki Watanabe Junichi Ohya Hirotaka Chikuda Yasuchika Aoki Masayuki Shimizu Toshimasa Futatsugi Keijiro Mukaiyama Masaichi Hasegawa Katsuhito Kiyasu Haku Iizuka Kotaro Nishida Kenichiro Kakutani Hideaki Nakajima Hideki Murakami Satoru Demura Satoshi Kato Katsuhito Yoshioka Takashi Namikawa Kei Watanabe Kazuyoshi Nakanishi Yukihiro Nakagawa Mitsunori Yoshimoto Hiroyasu Fujiwara Norihiro Nishida Masataka Sakane Masashi Yamazaki Takashi Kaito Takeo Furuya Sumihisa Orita Seiji Ohtori
- 出版者
- The Japanese Society for Spine Surgery and Related Research
- 雑誌
- Spine Surgery and Related Research (ISSN:2432261X)
- 巻号頁・発行日
- vol.1, no.4, pp.179-184, 2017-10-20 (Released:2017-11-27)
- 参考文献数
- 26
- 被引用文献数
- 3 3
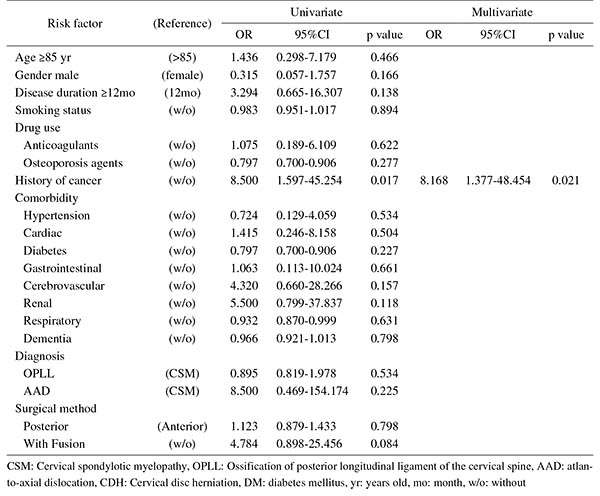
Introduction: With an aging population, the proportion of patients aged ≥80 years requiring cervical surgery is increasing. Surgeons are concerned with the high incidence of complications in this population, because "age" itself has been reported as a strong risk factor for complications. However, it is still unknown which factors represent higher risk among these elderly patients. Therefore, this study was conducted to identify the risk factors related to surgical complications specific to elderly patients by analyzing the registry data of patients aged ≥80 years who underwent cervical surgery.Methods: We retrospectively studied multicenter collected registry data using multivariate analysis. Sixty-six patients aged ≥80 years who underwent cervical surgery and were followed up for more than one year were included in this study. Preoperative patient demographic data, including comorbidities and postoperative complications, were collected from multicenter registry data. Complications were considered as major if they required invasive intervention, caused prolonged morbidity, or resulted in prolongation of hospital stay. Logistic regression analysis was performed to analyze the risk factors for complications. A p-value of <0.05 was considered as statistically significant.Results: The total number of patients with complications was 21 (31.8%), with seven major (10.6%) and 14 minor (21.2%) complications. Multivariate logistic regression analysis, after adjusting for age, revealed two significant risk factors: preoperative cerebrovascular disorders (OR, 6.337; p=0.043) for overall complications and cancer history (OR, 8.168; p=0.021) for major complications. Age, presence of diabetes mellitus, and diagnosis were not significant predictive factors for complications in this study.Conclusions: Preoperative cerebrovascular disorders and cancer history were risk factors for complications after cervical surgery in patients over 80 years old. Surgeons should pay attention to these specific risk factors before performing cervical surgery in elderly patients.
- 著者
- Gen Inoue Takashi Kaito Yukihiro Matsuyama Toshihiko Yamashita Mamoru Kawakami Kazuhisa Takahashi Munehito Yoshida Shiro Imagama Seiji Ohtori Toshihiko Taguchi Hirotaka Haro Hiroshi Taneichi Masashi Yamazaki Kotaro Nishida Hiroshi Yamada Daijiro Kabata Ayumi Shintani Motoki Iwasaki Manabu Ito Naohisa Miyakoshi Hideki Murakami Kazuo Yonenobu Tomoyuki Takura Joji Mochida
- 出版者
- The Japanese Society for Spine Surgery and Related Research
- 雑誌
- Spine Surgery and Related Research (ISSN:2432261X)
- 巻号頁・発行日
- pp.2020-0083, (Released:2020-11-20)
- 被引用文献数
- 2
Introduction: Chronic low back pain (CLBP) is a leading cause of disability, yet there is limited high-quality evidence to identify the most suitable pharmacological therapy. The purpose of this Japanese nationwide, multicenter, prospective study was to compare the effectiveness of four representative drug therapies—acetaminophen, celecoxib, loxoprofen, and a tramadol and acetaminophen (T+A) combination drug—to establish evidence for a drug of choice for CLBP.Methods: Patients with CLBP (N = 471) received one of the four treatments and were evaluated, prospectively and comprehensively, once every month for six months using a visual analog scale (VAS) for LBP, the Japanese Orthopedic Association (JOA) score, the JOA Back Pain Evaluation Questionnaire (JOABPEQ), the Roland–Morris Disability Questionnaire (RDQ), the EuroQol five-dimensions three-levels (EQ-5D-3L), and the Short Form-8 item health survey (SF-8). We conducted multivariable linear regression analyses of the four drugs at 1 and 6 months after drug allocation. Differences with P < 0.05 were considered statistically significant.Results: Patients who received acetaminophen showed a significant improvement from baseline in the mental health subscale of the JOABPEQ at one month (P = 0.02) and the JOA score at six months (P < 0.01). None of the other outcome measures among the four drugs differed significantly. Across groups, all outcome measures, except the mental component summary (MCS) score of the SF-8, improved equivalently, although most measurements showed no obvious cumulative effect over six months. The MCS score of the SF-8 decreased gradually over six months in all groups.Conclusions: Most of the outcome measures among the treated groups were not significantly different, indicating similar treatment effects of the four drugs for CLBP. Our study indicated the limit of each outcome measure for evaluating the patient status, suggesting that a single outcome measure is insufficient to reflect treatment effectiveness.