- 著者
- Masashi Uehara Shota Ikegami Takashi Takizawa Hiroki Oba Noriaki Yokogawa Takeshi Sasagawa Kei Ando Hiroaki Nakashima Naoki Segi Toru Funayama Fumihiko Eto Akihiro Yamaji Kota Watanabe Satoshi Nori Kazuki Takeda Takeo Furuya Sumihisa Orita Hideaki Nakajima Tomohiro Yamada Tomohiko Hasegawa Yoshinori Terashima Ryosuke Hirota Hidenori Suzuki Yasuaki Imajo Hitoshi Tonomura Munehiro Sakata Ko Hashimoto Yoshito Onoda Kenichi Kawaguchi Yohei Haruta Nobuyuki Suzuki Kenji Kato Hiroshi Uei Hirokatsu Sawada Kazuo Nakanishi Kosuke Misaki Hidetomi Terai Koji Tamai Eiki Shirasawa Gen Inoue Kenichiro Kakutani Yuji Kakiuchi Katsuhito Kiyasu Hiroyuki Tominaga Hiroto Tokumoto Yoichi Iizuka Eiji Takasawa Koji Akeda Norihiko Takegami Haruki Funao Yasushi Oshima Takashi Kaito Daisuke Sakai Toshitaka Yoshii Tetsuro Ohba Bungo Otsuki Shoji Seki Masashi Miyazaki Masayuki Ishihara Seiji Okada Yasuchika Aoki Katsumi Harimaya Hideki Murakami Ken Ishii Seiji Ohtori Shiro Imagama Satoshi Kato
- 出版者
- The Japanese Society for Spine Surgery and Related Research
- 雑誌
- Spine Surgery and Related Research (ISSN:2432261X)
- 巻号頁・発行日
- pp.2021-0183, (Released:2021-12-27)
- 被引用文献数
- 2
Background: In elderly patients with cervical spinal cord injury, comorbidities such as cardiovascular and cerebrovascular diseases are common, with frequent administration of antiplatelet/anticoagulant (APAC) drugs. Such patients may bleed easily or unexpectedly during surgery despite prior withdrawal of APAC medication. Few reports have examined the precise relationship between intraoperative blood loss and history of APAC use regarding surgery for cervical spine injury in the elderly.The presentmulticenter database survey aimed to answer the question of whether the use of APAC drugs affected the amount of intraoperative blood loss in elderly patients with cervical spinal cord trauma.Methods: The case histories of 1512 patients with cervical spine injury at 33 institutes were retrospectively reviewed. After excluding cases without spinal surgery or known blood loss volume, 797 patients were enrolled. Blood volume loss was the outcome of interest. We calculated propensity scores using the inverse probability of treatment weighting (IPTW) method. As an alternative sensitivity analysis, linear mixed model analyses were conducted as well.Results: Of the 776 patients (mean age: 75.1 ± 6.4 years) eligible for IPTW calculation, 157 (20.2%) were taking APAC medications before the injury. After weighting, mean estimated blood loss was 204 mL for non-APAC patients and 215 mL for APAC patients. APAC use in elderly patients was not significantly associated with surgical blood loss according to the IPTW method with propensity scoring or linear mixed model analyses. Thus, it appeared possible to perform surgery expecting comparable blood loss in APAC and non-APAC cases.Conclusions: This multicenter study revealed no significant increase in surgical blood loss in elderly patients with cervical trauma taking APAC drugs. Surgeons may be able to prioritize patient background, complications, and preexisting conditions over APAC use before injury when examining the surgical indications for cervical spine trauma in the elderly.
- 著者
- Yoshiharu Kawaguchi Masato Nakano Taketoshi Yasuda Shoji Seki Kayo Suzuki Yasuhito Yahara Hiroto Makino Masahiko Kanamori Tomoatsu Kimura
- 出版者
- The Japanese Society for Spine Surgery and Related Research
- 雑誌
- Spine Surgery and Related Research (ISSN:2432261X)
- 巻号頁・発行日
- vol.1, no.4, pp.174-178, 2017-10-20 (Released:2017-11-27)
- 参考文献数
- 13
- 被引用文献数
- 1 1
Introduction: In more than 20 years' follow-up after cervical laminoplasty, some patients died at an early stage, within 5 years postoperatively. The details remain unclear. This study was conducted to elucidate the clinical features in patients who died at an early stage after cervical laminoplasty to determine possible preventive measures against early death after surgery.Methods: A total of 74 patients who died with the follow-up period were included. The patients were divided into two groups: patients with a short survival period (S group, died ≤5 years after surgery) and patients with a long survival period (L group, died >5 years after surgery). Diseases, gender, age, causes of the death, general complications before surgery, and the pre- and postoperative JOA scores were compared between the two groups.Results: Eleven patients (15%) died within 5 years after laminoplasty. The average age at death in the S group was 68.7 years which was considerably younger than that in the L group (80.2 years). The ratio of pneumonia was higher in the S group, compared to that in the L group. Postoperative JOA score in the S group was lower than that in the L group.Conclusions: 11 patients out of 74 patients (15%) died within 5 years after laminoplasty. The average age at the death in the S group was much younger than that in the L group. The postoperative JOA score in the S group was lower than that in the L group. As pneumonia was more prevalent in the S group, it might be reasonable to give the information for the protection of pneumonia after cervical laminoplasty.
- 著者
- Koji Tamai Hidetomi Terai Akinobu Suzuki Hiroaki Nakamura Masaomi Yamashita Yawara Eguchi Shiro Imagama Kei Ando Kazuyoshi Kobayashi Morio Matsumoto Ken Ishii Tomohiro Hikata Shoji Seki Masaaki Aramomi Tetsuhiro Ishikawa Atsushi Kimura Hirokazu Inoue Gen Inoue Masayuki Miyagi Wataru Saito Kei Yamada Michio Hongo Kenji Endo Hidekazu Suzuki Atsushi Nakano Kazuyuki Watanabe Junichi Ohya Hirotaka Chikuda Yasuchika Aoki Masayuki Shimizu Toshimasa Futatsugi Keijiro Mukaiyama Masaichi Hasegawa Katsuhito Kiyasu Haku Iizuka Kotaro Nishida Kenichiro Kakutani Hideaki Nakajima Hideki Murakami Satoru Demura Satoshi Kato Katsuhito Yoshioka Takashi Namikawa Kei Watanabe Kazuyoshi Nakanishi Yukihiro Nakagawa Mitsunori Yoshimoto Hiroyasu Fujiwara Norihiro Nishida Masataka Sakane Masashi Yamazaki Takashi Kaito Takeo Furuya Sumihisa Orita Seiji Ohtori
- 出版者
- The Japanese Society for Spine Surgery and Related Research
- 雑誌
- Spine Surgery and Related Research (ISSN:2432261X)
- 巻号頁・発行日
- vol.1, no.4, pp.179-184, 2017-10-20 (Released:2017-11-27)
- 参考文献数
- 26
- 被引用文献数
- 3 3
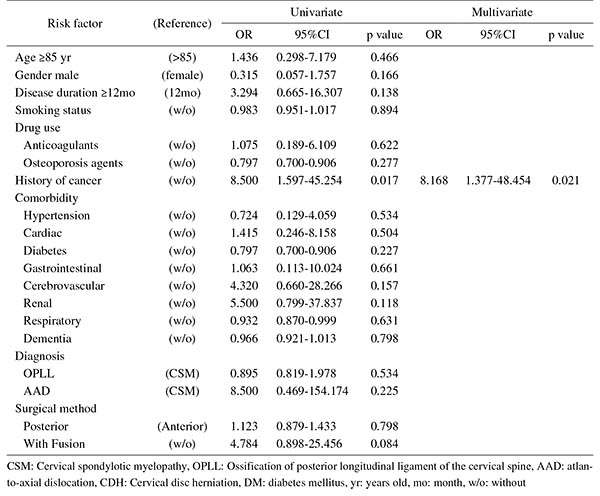
Introduction: With an aging population, the proportion of patients aged ≥80 years requiring cervical surgery is increasing. Surgeons are concerned with the high incidence of complications in this population, because "age" itself has been reported as a strong risk factor for complications. However, it is still unknown which factors represent higher risk among these elderly patients. Therefore, this study was conducted to identify the risk factors related to surgical complications specific to elderly patients by analyzing the registry data of patients aged ≥80 years who underwent cervical surgery.Methods: We retrospectively studied multicenter collected registry data using multivariate analysis. Sixty-six patients aged ≥80 years who underwent cervical surgery and were followed up for more than one year were included in this study. Preoperative patient demographic data, including comorbidities and postoperative complications, were collected from multicenter registry data. Complications were considered as major if they required invasive intervention, caused prolonged morbidity, or resulted in prolongation of hospital stay. Logistic regression analysis was performed to analyze the risk factors for complications. A p-value of <0.05 was considered as statistically significant.Results: The total number of patients with complications was 21 (31.8%), with seven major (10.6%) and 14 minor (21.2%) complications. Multivariate logistic regression analysis, after adjusting for age, revealed two significant risk factors: preoperative cerebrovascular disorders (OR, 6.337; p=0.043) for overall complications and cancer history (OR, 8.168; p=0.021) for major complications. Age, presence of diabetes mellitus, and diagnosis were not significant predictive factors for complications in this study.Conclusions: Preoperative cerebrovascular disorders and cancer history were risk factors for complications after cervical surgery in patients over 80 years old. Surgeons should pay attention to these specific risk factors before performing cervical surgery in elderly patients.