- 著者
- Kaeko Hirai Rika Kawakami Maki Nogi Satomi Ishihara Yukihiro Hashimoto Yasuki Nakada Hitoshi Nakagawa Tomoya Ueda Taku Nishida Kenji Onoue Tsunenari Soeda Satoshi Okayama Makoto Watanabe Hiroyuki Okura Yoshihiko Saito
- 出版者
- The Japanese Circulation Society
- 雑誌
- Circulation Reports (ISSN:24340790)
- 巻号頁・発行日
- vol.3, no.7, pp.388-395, 2021-07-09 (Released:2021-07-09)
- 参考文献数
- 28
- 被引用文献数
- 1
Background:Atrial fibrillation (AF) and mitral regurgitation (MR) are frequently combined in patients with heart failure (HF). However, the effect of AF on the prognosis of patients with HF and MR remains unknown.Methods and Results:We studied 867 patients (mean age 73 years; 42.7% female) with acute decompensated HF (ADHF) in the NARA-HF registry. Patients were divided into 4 groups based on the presence or absence of AF and MR at discharge. Patients with severe MR were excluded. The primary endpoint was the composite of cardiovascular (CV) death and HF-related readmission. During the median follow-up of 621 days, 398 patients (45.9%) reached the primary endpoint. In patients with MR, AF was associated with a higher incidence of the primary endpoint regardless of left ventricular function; however, in patients without MR, AF was not associated with CV events. Cox multivariate analyses showed that the incidence of CV events was significantly higher in patients with AF and MR than in patients with MR but without AF (hazard ratio 1.381, P=0.036). Similar findings were obtained in subgroup analysis of patients with AF and only mild MR.Conclusions:The present study demonstrated that AF is associated with poor prognosis in patients with ADHF with mild to moderate MR, but not in those without MR.
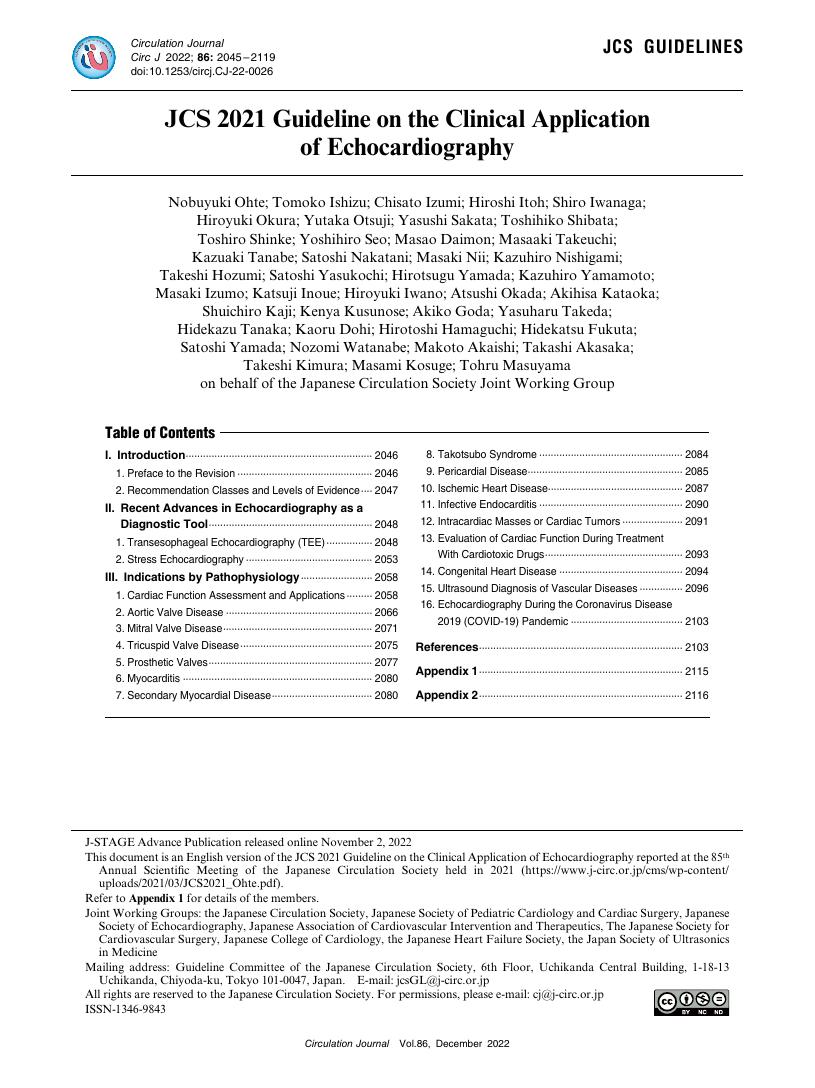
- 著者
- Nobuyuki Ohte Tomoko Ishizu Chisato Izumi Hiroshi Itoh Shiro Iwanaga Hiroyuki Okura Yutaka Otsuji Yasushi Sakata Toshihiko Shibata Toshiro Shinke Yoshihiro Seo Masao Daimon Masaaki Takeuchi Kazuaki Tanabe Satoshi Nakatani Masaki Nii Kazuhiro Nishigami Takeshi Hozumi Satoshi Yasukochi Hirotsugu Yamada Kazuhiro Yamamoto Masaki Izumo Katsuji Inoue Hiroyuki Iwano Atsushi Okada Akihisa Kataoka Shuichiro Kaji Kenya Kusunose Akiko Goda Yasuharu Takeda Hidekazu Tanaka Kaoru Dohi Hirotoshi Hamaguchi Hidekatsu Fukuta Satoshi Yamada Nozomi Watanabe Makoto Akaishi Takashi Akasaka Takeshi Kimura Masami Kosuge Tohru Masuyama on behalf of the Japanese Circulation Society Joint Working Group
- 出版者
- The Japanese Circulation Society
- 雑誌
- Circulation Journal (ISSN:13469843)
- 巻号頁・発行日
- vol.86, no.12, pp.2045-2119, 2022-11-25 (Released:2022-11-25)
- 参考文献数
- 460
- 被引用文献数
- 16
- 著者
- Yuki Sahashi Tatsuma Serge Yanagimoto Susumu Endo Hiroaki Ushikoshi Hiroyuki Okura
- 出版者
- The Japanese Society of Internal Medicine
- 雑誌
- Internal Medicine (ISSN:09182918)
- 巻号頁・発行日
- pp.4123-19, (Released:2020-03-12)
- 参考文献数
- 10
- 被引用文献数
- 1
We herein report a 26-year-old woman with sudden cardiac arrest who had no remarkable medical history. While resuscitation was successfully performed with adrenalin administration and extracorporeal membrane oxygenation, the cause of cardiac arrest could not be determined for over two weeks. Given the presence of autoimmune disease along with the findings of refractory renal insufficiency and thrombocytopenia, a kidney biopsy and blood examinations, including lupus anticoagulant testing, were performed, which proved the presence of antiphospholipid syndrome. The patient was successfully treated with steroid pulse therapy. This drastic case scenario highlighted the fact that autoimmune disease can be the cause of sudden cardiac arrest.
- 著者
- Ayako Sekine Takatomo Watanabe Genki Naruse Ayae Takada Shingo Fujimoto Noriko Ozawa Koichi Shinoda Yuzuru Nohisa Hiroyuki Okura
- 出版者
- The Japanese Circulation Society
- 雑誌
- Circulation Journal (ISSN:13469843)
- 巻号頁・発行日
- vol.85, no.1, pp.78, 2020-12-25 (Released:2020-12-25)
- 参考文献数
- 1
- 著者
- Yasuki Nakada Rika Kawakami Shouji Matsushima Tomomi Ide Koshiro Kanaoka Tomoya Ueda Satomi Ishihara Taku Nishida Kenji Onoue Tsunenari Soeda Satoshi Okayama Makoto Watanabe Hiroyuki Okura Miyuki Tsuchihashi-Makaya Hiroyuki Tsutsui Yoshihiko Saito
- 出版者
- The Japanese Circulation Society
- 雑誌
- Circulation Journal (ISSN:13469843)
- 巻号頁・発行日
- vol.83, no.5, pp.1019-1024, 2019-04-25 (Released:2019-04-25)
- 参考文献数
- 22
- 被引用文献数
- 8 13
Background: Prognosis after acute decompensated heart failure (ADHF) is poor. An appropriate risk score that would allow for improved care and treatment of ADHF patients after discharge, however, is lacking. Methods and Results: We used 2 HF cohorts, the NARA-HF study and JCARE-CARD, as derivation and validation cohorts, respectively. The primary endpoint was all-cause death during the 2-year follow-up, excluding in-hospital death. Age, hemoglobin (Hb), and brain natriuretic peptide (BNP) at discharge were identified as independent risk factors. We determined 3 categorizations on the basis of these parameters, termed A2B score: age (<65 years, 0; 65–74 years, 1; ≥75 years, 2), anemia (Hb <10 g/dL, 2; 10–11.9 g/dL, 1; ≥12 g/dL, 0) and BNP (<200 pg/mL, 0; 200–499 pg/mL, 1; ≥500 pg/mL, 2). We divided patients into 4 groups according to A2B score (extremely low, 0; low, 1–2; medium, 3–4; high, 5–6). For the extremely low-risk group, the 2-year survival rate was 97.8%, compared with 84.5%, 66.1%, and 45.2% for the low-, medium-, and high-risk groups, respectively. Using the JCARE-CARD as a validation model, for the extremely low-risk group, the 2-year survival was 95.4%, compared with 90.2%, 75.0%, and 55.6% for the low-, medium-, and high-risk groups, respectively. Conclusions: The user-friendly A2B score is useful for estimating survival rate in ADHF patients at discharge.
- 著者
- Koshiro Kanaoka Satoshi Okayama Michikazu Nakai Yoko Sumita Kunihiro Nishimura Rika Kawakami Hiroyuki Okura Yoshihiro Miyamoto Satoshi Yasuda Hiroyuki Tsutsui Issei Komuro Hisao Ogawa Yoshihiko Saito
- 出版者
- The Japanese Circulation Society
- 雑誌
- Circulation Journal (ISSN:13469843)
- 巻号頁・発行日
- vol.83, no.5, pp.1025-1031, 2019-04-25 (Released:2019-04-25)
- 参考文献数
- 21
- 被引用文献数
- 31 46
Background: With aging of the population, the economic burden associated with heart failure (HF) is expected to increase. However, little is known about the hospitalization costs associated with HF in Japan. Methods and Results: In this cross-sectional study, using data from The Japanese Registry of All Cardiac and Vascular Diseases (JROAD) and JROAD-Diagnosis Procedure Combination databases between 2012 and 2014, we evaluated hospitalization costs for acute cardiovascular diseases (CVDs), including HF. A total of $1,187 million/year (44% of the hospitalization costs for acute CVDs) was spent on patients with HF. We identified 273,865 patients with HF and the median cost per patient was $8,089 ($5,362–12,787) per episode. The top 1% of spenders accounted for 8% ($80 million/year), and the top 5% of spenders accounted for 22% ($229 million/year) of the entire cost associated with HF. The costs associated with HF for patients over 75 years of age accounted for 68% of the total cost. Conclusions: The costs associated with HF were higher than the hospitalization cost for any other acute CVD in Japan. Understanding how the total hospitalization cost is distributed may allow health providers to utilize limited resources more effectively for patients with HF.
- 著者
- Takahiro ANDO Takatomo WATANABE Saori MATSUO Tomoki SAMEJIMA Junya YAMAGISHI Takanobu BITO Genki NARUSE Akihiro YOSHIDA Shingo MINATOGUCHI Haruhiko AKIYAMA Kazuhiko NISHIGAKI Shinya MINATOGUCHI Hiroyuki OKURA
- 出版者
- Japanese Society of Physical Therapy
- 雑誌
- Physical Therapy Research (ISSN:21898448)
- 巻号頁・発行日
- vol.25, no.1, pp.18-25, 2022-04-20 (Released:2022-04-20)
- 参考文献数
- 26
Objective: To examine the Cardiac Rehabilitation Gifu Network (CR-GNet) feasibility in managing diseases and assisting patients in attaining physical fitness, and its impact on long-term outcomes after acute coronary syndrome (ACS). Methods: In this prospective observational study, we enrolled 47 patients with ACS registered in the CR-GNet between February 2016 and September 2019. 37, 29, and 21 patients underwent follow-up assessments for exercise capacity (peak oxygen uptake) at 3 months, 6 months, and 1 year after discharge, respectively. Major adverse cardiac events (MACE) were compared with controls not registered in the CR-GNet. Results: The coronary risk factors, except blood pressure, improved at 3 and 6 months, and 1 year after discharge. These risk factors in each patient significantly reduced from 2.9 at admission to 1.6, 1.4, and 1.9 at 3 months, 6 months, and 1 year after discharge (p<0.05), respectively. Peak oxygen uptake was significantly higher at 3 months (17.5±4.9 ml/kg/min), 6 months (17.9±5.1 ml/kg/min), and 1 year (17.5±5.5 ml/kg/min) after discharge than that at discharge (14.7±3.6 ml/kg/min) (p<0.05). During follow-up, there was no significant difference; MACE did not occur in any patients in the CR-GNet but occurred in controls. Conclusion: CR-GNet is a feasible option for the long-term management of ACS patients.
- 著者
- Hiroyuki Okura
- 出版者
- The Japanese Circulation Society
- 雑誌
- Circulation Journal (ISSN:13469843)
- 巻号頁・発行日
- pp.CJ-21-0692, (Released:2021-09-15)
- 参考文献数
- 15
- 著者
- Ryotaro Yamada Hiroyuki Okura Teruyoshi Kume Yoji Neishi Takahiro Kawamoto Yoshinori Miyamoto Koichiro Imai Ken Saito Tetsuo Tsuchiya Akihiro Hayashida Kiyoshi Yoshida
- 出版者
- The Japanese Circulation Society
- 雑誌
- Circulation Journal (ISSN:13469843)
- 巻号頁・発行日
- vol.74, no.8, pp.1658-1662, 2010 (Released:2010-07-23)
- 参考文献数
- 30
- 被引用文献数
- 18 16
Background: Several reports suggest that virtual histology intravascular ultrasound (VH-IVUS) assessment could predict microvascular damage during percutaneous coronary intervention (PCI). A novel index of microcirculatory resistance (IMR) has been developed as a reproducible and less hemodynamic-dependent index. The purpose of this study was to investigate the relationship between thin-cap fibroatheroma (TCFA) defined by VH-IVUS and a change in the IMR during PCI in patients with angina pectoris (AP). Methods and Results: The study investigated 30 lesions from 28 AP patients. VH-IVUS imaging was performed before PCI. TCFA was defined as the presence of confluent necrotic core (>10%) without detectable overlying fibrous cap segment. Patients were divided into 2 groups according to the presence of TCFA. Using a pressure guidewire, IMR were measured before and after PCI. After successful PCI, patients were prospectively followed up clinically. TCFA was detected in 9 lesions (30%). IMR tended to improve after PCI in the non-TCFA group, but tended to worsen in the TCFA group. ΔIMR (=IMR after PCI-IMR before PCI) was significantly higher in the TCFA group compared with the non-TCFA group (13.2±29.9 vs -4.4±16.0, P=0.04). During follow-up (mean 20 months), survival free of major adverse cardiac events was significantly less in the TCFA group than in the non-TCFA group. Conclusions: Target lesion TCFA may be related to both microvascular injury and the long-term clinical outcome after successful PCI in patients with AP. (Circ J 2010; 74: 1658 - 1662)
- 著者
- Atsushi Kyodo Makoto Watanabe Akihiko Okamura Saki Iwai Azusa Sakagami Kazutaka Nogi Daisuke Kamon Yukihiro Hashimoto Tomoya Ueda Tsunenari Soeda Hiroyuki Okura Yoshihiko Saito
- 出版者
- The Japanese Circulation Society
- 雑誌
- Circulation Journal (ISSN:13469843)
- 巻号頁・発行日
- pp.CJ-20-0759, (Released:2021-01-27)
- 参考文献数
- 33
- 被引用文献数
- 4
Background:The association between unfavorable post-stent optical coherence tomography (OCT) findings and subsequent stent thrombosis (ST) remains unclear. This study investigated the ST-related characteristics of post-stent OCT findings at index percutaneous coronary intervention (PCI).Methods and Results:Fifteen patients with ST onset after OCT-guided PCI (ST group) were retrospectively enrolled. Post-stent OCT findings in the ST group were compared with those in 70 consecutive patients (reference group) without acute coronary syndrome onset for at least 5 years after OCT-guided PCI. The incidence of acute myocardial infarction (AMI) was higher in the ST than reference group (60.0% vs. 17.1%, respectively; P=0.0005). The incidence of incomplete stent apposition (93.3% vs. 55.7%; P=0.0064), irregular protrusion (IP; 93.3% vs. 62.8%; P=0.0214), and thrombus (93.3% vs. 51.4%; P=0.0028) was significantly higher in the ST than reference group. The maximum median (interquartile range) IP arc was significantly larger in the ST than reference group (265° [217°–360°] vs. 128° [81.4°–212°], respectively; P<0.0001). In AMI patients, the incidence of a maximum IP arc >180° was significantly higher in the ST than reference group (100% vs. 58.3%, respectively; P=0.0265).Conclusions:IP with a large arc was a significant feature on post-stent OCT in patients with ST.
- 著者
- Junko Naito Hiroshige Ohashi Michiya Ohno Masafumi Sugiyama Kazuyoshi Hayakawa Akihisa Kunishima Nobuyuki Takada Tatsuya Kariya Koshi Goto Hisato Takatsu Toshiki Ohira Koji Nakahara Ichijiro Murata Shingo Minatoguchi Gakuro Yoshida Hiroyuki Okura Shinya Minatoguchi
- 出版者
- The Japanese Circulation Society
- 雑誌
- Circulation Reports (ISSN:24340790)
- 巻号頁・発行日
- vol.1, no.11, pp.508-516, 2019-11-08 (Released:2019-11-08)
- 参考文献数
- 31
- 被引用文献数
- 2
Background:Levocarnitine has been reported to improve the left ventricular (LV) systolic function and decrease LV hypertrophy in hemodialysis (HD) patients. Its effect on LV diastolic dysfunction, however, has not yet been clarified.Methods and Results:HD patients (n=88) were given levocarnitine i.v. 1,000 mg for 12 months at the end of every dialysis session through the dialysis circuit of the venous site. LV ejection fraction (EF), E/A, E/e’, left atrial volume index (LAVI) and LV mass index (LVMI) were measured before and 3, 6, 9, and 12 months after the start of levocarnitine on echocardiography. We regarded E/A≤0.8, E/e’>14 and LAVI>34 mL/m2as LV diastolic dysfunction, and LVEF<55% as LV systolic dysfunction. We also investigated the effect of levocarnitine on HFpEF. Plasma brain natriuretic peptide, total carnitine, free carnitine, and acyl-carnitine and biochemistry parameters were measured. Levocarnitine significantly improved LV diastolic function in HD patients with LV diastolic dysfunction, but did not affect LV diastolic function in those with normal LV diastolic function. Levocarnitine significantly improved HFpEF. Levocarnitine significantly improved the LV systolic function in HD patients with LV systolic dysfunction but did not affect the LV systolic function in those with normal LV systolic function. Levocarnitine significantly decreased LVMI and increased plasma total, free, and acyl-carnitine.Conclusions:Levocarnitine ameliorates LV diastolic as well as LV systolic dysfunction in HD patients.