- 著者
- Hiroyuki Tsutsui Mitsuaki Isobe Hiroshi Ito Hiroshi Ito Ken Okumura Minoru Ono Masafumi Kitakaze Koichiro Kinugawa Yasuki Kihara Yoichi Goto Issei Komuro Yoshikatsu Saiki Yoshihiko Saito Yasushi Sakata Naoki Sato Yoshiki Sawa Akira Shiose Wataru Shimizu Hiroaki Shimokawa Yoshihiko Seino Koichi Node Taiki Higo Atsushi Hirayama Miyuki Makaya Tohru Masuyama Toyoaki Murohara Shin-ichi Momomura Masafumi Yano Kenji Yamazaki Kazuhiro Yamamoto Tsutomu Yoshikawa Michihiro Yoshimura Masatoshi Akiyama Toshihisa Anzai Shiro Ishihara Takayuki Inomata Teruhiko Imamura Yu-ki Iwasaki Tomohito Ohtani Katsuya Onishi Takatoshi Kasai Mahoto Kato Makoto Kawai Yoshiharu Kinugasa Shintaro Kinugawa Toru Kuratani Shigeki Kobayashi Yasuhiko Sakata Atsushi Tanaka Koichi Toda Takashi Noda Kotaro Nochioka Masaru Hatano Takayuki Hidaka Takeo Fujino Shigeru Makita Osamu Yamaguchi Uichi Ikeda Takeshi Kimura Shun Kohsaka Masami Kosuge Masakazu Yamagishi Akira Yamashina on behalf of the Japanese Circulation Society and the Japanese Heart Failure Society Joint Working Group
- 出版者
- The Japanese Circulation Society
- 雑誌
- Circulation Journal (ISSN:13469843)
- 巻号頁・発行日
- vol.83, no.10, pp.2084-2184, 2019-09-25 (Released:2019-09-25)
- 参考文献数
- 608
- 被引用文献数
- 435
22 0 0 0 OA JCS/JHFS 2021 Guideline Focused Update on Diagnosis and Treatment of Acute and Chronic Heart Failure
- 著者
- Hiroyuki Tsutsui Tomomi Ide Hiroshi Ito Yasuki Kihara Koichiro Kinugawa Shintaro Kinugawa Miyuki Makaya Toyoaki Murohara Koichi Node Yoshihiko Saito Yasushi Sakata Wataru Shimizu Kazuhiro Yamamoto Yasuko Bando Yu-ki Iwasaki Yoshiharu Kinugasa Isamu Mizote Hitoshi Nakagawa Shogo Oishi Akiko Okada Atsushi Tanaka Takashi Akasaka Minoru Ono Takeshi Kimura Shun Kosaka Masami Kosuge Shin-ichi Momomura on behalf of the Japanese Circulation Society and the Japanese Heart Failure Society Joint Working Group
- 出版者
- The Japanese Circulation Society
- 雑誌
- Circulation Journal (ISSN:13469843)
- 巻号頁・発行日
- pp.CJ-21-0431, (Released:2021-09-29)
- 参考文献数
- 252
- 被引用文献数
- 84
- 著者
- Madoka Ihara Yuhei Nojima Hidenori Adachi Tetsuya Kurimoto Keita Okayama Yasushi Sakata Shinsuke Nanto
- 出版者
- The Japanese Circulation Society
- 雑誌
- Circulation Reports (ISSN:24340790)
- 巻号頁・発行日
- vol.2, no.2, pp.135-136, 2020-02-10 (Released:2020-02-10)
- 参考文献数
- 2
- 被引用文献数
- 1
- 著者
- Satomi Ishihara Shinya Hiramitsu Koshiro Kanaoka Mizuri Taki Hitoshi Nakagawa Tomoya Ueda Ayako Seno Taku Nishida Kenji Onoue Tsunenari Soeda Tomohito Ohtani Makoto Watanabe Rika Kawakami Yasushi Sakata Kazuomi Kario Yoshihiko Saito
- 出版者
- The Japanese Circulation Society
- 雑誌
- Circulation Journal (ISSN:13469843)
- 巻号頁・発行日
- pp.CJ-22-0032, (Released:2022-05-25)
- 参考文献数
- 33
- 被引用文献数
- 4
Background: Although B-type natriuretic peptide (BNP) and N-terminal (NT)-proBNP are commonly used markers of heart failure, a simple conversion formula between these peptides has not yet been developed for clinical use.Methods and Results: A total of 9,394 samples were obtained from Nara Medical University, Jichi Medical University, and Osaka University. We randomly selected 70% for a derivation set to investigate a conversion formula from BNP to NT-proBNP using estimated glomerular filtration rate (eGFR) and body mass index (BMI); the remaining 30% was used as the internal validation set and we used a cohort study from Nara Medical University as an external validation set. Multivariate linear regression analysis revealed a new conversion formula: log NT-proBNP = 1.21 + 1.03 × log BNP − 0.009 × BMI − 0.007 × eGFR (r2=0.900, P<0.0001). The correlation coefficients between the actual and converted values of log NT-proBNP in the internal and external validation sets were 0.942 (P<0.0001) and 0.891 (P<0.0001), respectively. We applied this formula to samples obtained from patients administered with sacubitril/valsartan. After treatment initiation, NT-proBNP levels decreased and actual BNP levels increased. However, the calculated BNP levels decreased roughly parallel to the NT-proBNP levels.Conclusions: This new and simple conversion formula of BNP and NT-proBNP with eGFR and BMI is potentially useful in clinical practice.
- 著者
- Minoru Ono Osamu Yamaguchi Tomohito Ohtani Koichiro Kinugawa Yoshikatsu Saiki Yoshiki Sawa Akira Shiose Hiroyuki Tsutsui Norihide Fukushima Goro Matsumiya Masanobu Yanase Kenji Yamazaki Kazuhiro Yamamoto Masatoshi Akiyama Teruhiko Imamura Kiyotaka Iwasaki Miyoko Endo Yoshihiko Ohnishi Takahiro Okumura Koichi Kashiwa Osamu Kinoshita Kaori Kubota Osamu Seguchi Koichi Toda Hiroshi Nishioka Tomohiro Nishinaka Takashi Nishimura Toru Hashimoto Masaru Hatano Haruhiko Higashi Taiki Higo Takeo Fujino Yumiko Hori Toru Miyoshi Motoharu Yamanaka Takayuki Ohno Takeshi Kimura Shunei Kyo Yasushi Sakata Takeshi Nakatani on behalf of the JCS/JSCVS/JATS/JSVS Joint Working Group
- 出版者
- The Japanese Circulation Society
- 雑誌
- Circulation Journal (ISSN:13469843)
- 巻号頁・発行日
- pp.CJ-21-0880, (Released:2022-04-05)
- 参考文献数
- 288
- 被引用文献数
- 10
- 著者
- Takashi Kuragaichi Yuma Kurozumi Shogo Ohishi Yasuo Sugano Akihiro Sakashita Norihiko Kotooka Makoto Suzuki Taiki Higo Dai Yumino Yasuko Takada Seiko Maeda Saori Yamabe Koichi Washida Tomonori Takahashi Tomohito Ohtani Yasushi Sakata Yukihito Sato
- 出版者
- The Japanese Circulation Society
- 雑誌
- Circulation Journal (ISSN:13469843)
- 巻号頁・発行日
- vol.82, no.5, pp.1336-1343, 2018-04-25 (Released:2018-04-25)
- 参考文献数
- 45
- 被引用文献数
- 16 26
Background:Palliative care for heart failure (HF) patients is recommended in Western guidelines, so this study aimed to clarify the current status of palliative care for HF patients in Japan.Methods and Results:A survey was sent to all Japanese Circulation Society-authorized cardiology training hospitals (n=1,004) in August 2016. A total of 544 institutions (54%) returned the questionnaire. Of them, 527 (98%) answered that palliative care is necessary for patients with HF. A total of 227 (42%) institutions held a palliative care conference for patients with HF, and 79% of the institutions had <10 cases per year. Drug therapy as palliative care was administered at 403 (76%) institutions; morphine (87%) was most frequently used. Among sedatives, dexmedetomidine (33%) was administered more often than midazolam (29%) or propofol (20%). Regarding the timing of end-of-life care, most institutions (84%) reported having considered palliative care when a patient reached the terminal stage of HF. Most frequently, the reason for the decision at the terminal stage was “difficulty in discontinuing cardiotonics.” A major impediment to the delivery of palliative care was “difficulty predicting an accurate prognosis.”Conclusions:This large-scale survey showed the characteristics of palliative care for HF in Japan. The present findings may aid in the development of effective end-of-life care systems.
- 著者
- Koshiro Kanaoka Yoshitaka Iwanaga Nagaharu Fukuma Michikazu Nakai Yoko Sumita Yuichi Nishioka Katsuki Okada Tatsuya Noda Yasushi Sakata Tomoaki Imamura Yoshihiro Miyamoto
- 出版者
- The Japanese Circulation Society
- 雑誌
- Circulation Journal (ISSN:13469843)
- 巻号頁・発行日
- pp.CJ-22-0095, (Released:2022-05-27)
- 参考文献数
- 31
- 被引用文献数
- 11
Background: Few studies have comprehensively evaluated the trends and factors associated with CR participation across major cardiovascular diseases in Japan.Methods and Results: This study performed a nationwide cross-sectional study using the National Database of Health Insurance Claims and Specific Health Checkups of Japan and the Japanese Registry of All Cardiac and Vascular Diseases and the Diagnosis Procedure Combination database. This study described the nationwide trends and evaluated patient- and hospital-level associated factors of CR participation for patients with acute heart failure (AHF), acute coronary syndrome (ACS), acute aortic dissection (AAD), peripheral artery disease (PAD), and after cardiovascular surgery using mixed-effect logistic regression analysis. Although the annual number of patients who underwent CR has increased during the study period, the total number of patients participating in outpatient CR was lower than that of inpatient CR. The outpatient CR participation rate was lower for patients with AHF (3.5%), AAD (3.2%), and PAD (1.7%), compared with ACS (7.9%) and after surgery (9.4%). Age, sex, body mass index, Barthel index, Charlson comorbidity index, and institutional capacity were identified as significant associated factors of CR participation in inpatient and outpatient settings.Conclusions: Participation in outpatient CR was still low, and higher age, multi-comorbidity, and low institutional capacity contributed to the lower outpatient CR participation rate. Identification of the associated factors may help cardiologists to increase CR participation.
- 著者
- Hirokai Kitaoka Hiroyuki Tsutsui Toru Kubo Tomomi Ide Taishiro Chikamori Keiichi Fukuda Noboru Fujino Taiki Higo Mitsuaki Isobe Chizuko Kamiya Seiya Kato Yasuki Kihara Koichiro Kinugawa Shintaro Kinugawa Shigetoyo Kogaki Issei Komuro Nobuhisa Hagiwara Minoru Ono Yuichiro Maekawa Shigeru Makita Yoshiro Matsui Shouji Matsushima Yasushi Sakata Yoshiki Sawa Wataru Shimizu Kunihiko Teraoka Miyuki Tsuchihashi-Makaya Hatsue Ishibashi-Ueda Masafumi Watanabe Michihiro Yoshimura Arata Fukusima Satoshi Hida Shungo Hikoso Teruhiko Imamura Hiroko Ishida Makoto Kawai Toshiro Kitagawa Takashi Kohno Satoshi Kurisu Yoji Nagata Makiko Nakamura Hiroyuki Morita Hitoshi Takano Tsuyoshi Shiga Yasuyoshi Takei Shinsuke Yuasa Teppei Yamamoto Tetsu Watanabe Takashi Akasaka Yoshinori Doi Takeshi Kimura Masafumi Kitakaze Masami Kosuge Morimasa Takayama Hitonobu Tomoike on behalf of the Japanese Circulation Society Joint Working Group
- 出版者
- The Japanese Circulation Society
- 雑誌
- Circulation Journal (ISSN:13469843)
- 巻号頁・発行日
- pp.CJ-20-0910, (Released:2021-07-22)
- 参考文献数
- 687
- 被引用文献数
- 47
- 著者
- Toshihisa Anzai Takuma Sato Yoshihiro Fukumoto Chisato Izumi Yoshiyuki Kizawa Masatoshi Koga Katsuji Nishimura Mitsuru Ohishi Akihiro Sakashita Yasushi Sakata Tsuyoshi Shiga Yasuchika Takeishi Satoshi Yasuda Kazuhiro Yamamoto Takahiro Abe Rie Akaho Yasuhiro Hamatani Hayato Hosoda Naoki Ishimori Mika Kato Yoshiharu Kinugasa Takuro Kubozono Toshiyuki Nagai Shogo Oishi Katsuki Okada Tatsuhiro Shibata Atsushi Suzuki Tsuyoshi Suzuki Masahito Takagi Yasuko Takada Kenkichi Tsuruga Akiomi Yoshihisa Dai Yumino Keiichi Fukuda Yasuki Kihara Yoshihiko Saito Yoshiki Sawa Hiroyuki Tsutsui Takeshi Kimura on behalf of the Japanese Circulation Society Joint Working Group
- 出版者
- The Japanese Circulation Society
- 雑誌
- Circulation Journal (ISSN:13469843)
- 巻号頁・発行日
- pp.CJ-20-1127, (Released:2021-03-26)
- 参考文献数
- 316
- 被引用文献数
- 19
- 著者
- Hiroyuki Tsutsui Shin-ichi Momomura Yoshihiko Saito Hiroshi Ito Kazuhiro Yamamoto Yasushi Sakata Tomomi Ohishi Pankaj Kumar Toshihito Kitamura
- 出版者
- The Japanese Circulation Society
- 雑誌
- Circulation Journal (ISSN:13469843)
- 巻号頁・発行日
- pp.CJ-23-0174, (Released:2023-08-26)
- 参考文献数
- 38
Background: The PARALLEL-HF study assessed the efficacy and safety of sacubitril/valsartan vs. enalapril in Japanese patients with chronic heart failure with reduced ejection fraction (HFrEF). This open-label extension (OLE) assessed long-term safety with sacubitril/valsartan.Methods and Results: This study enrolled 150 patients who received sacubitril/valsartan 50 or 100 mg, b.i.d., in addition to optimal background heart failure (HF) therapy. A dose level of sacubitril/valsartan 200 mg, b.i.d., was targeted by Week 8. At OLE baseline, higher concentrations of B-type natriuretic peptide (BNP) and urine cGMP, and lower concentrations of N-terminal pro B-type natriuretic peptide (NT-proBNP), were observed in the sacubitril/valsartan core group (patients who received sacubitril/valsartan in both the core and extension study) than in the enalapril core group (patients who received enalapril in the core study and were then transitioned to sacubitril/valsartan). The mean exposure to study drug was 98.9%. There was no trend of worsening of HF at Month 12. No obvious changes in cardiac biomarkers were observed, whereas BNP and urine cGMP increased and NT-proBNP decreased in the enalapril core group, which was evident at Weeks 2–4 and sustained to Month 12.Conclusions: Long-term sacubitril/valsartan at doses up to 200 mg, b.i.d., has a positive risk-benefit profile; it was safe and well tolerated in Japanese patients with chronic HFrEF.
7 0 0 0 OA Validity of Diagnostic Algorithms for Cardiovascular Diseases in Japanese Health Insurance Claims
- 著者
- Koshiro Kanaoka Yoshitaka Iwanaga Katsuki Okada Satoshi Terasaki Yuichi Nishioka Michikazu Nakai Daisuke Kamon Tomoya Myojin Tsunenari Soeda Tatsuya Noda Manabu Horii Yasushi Sakata Yoshihiro Miyamoto Yoshihiko Saito Tomoaki Imamura
- 出版者
- The Japanese Circulation Society
- 雑誌
- Circulation Journal (ISSN:13469843)
- 巻号頁・発行日
- vol.87, no.4, pp.536-542, 2023-03-24 (Released:2023-03-24)
- 参考文献数
- 22
- 被引用文献数
- 6
Background: We aimed to validate a claims-based diagnostic algorithm to identify hospitalized patients with acute major cardiovascular diseases (CVDs) from health insurance claims in Japan.Methods and Results: This retrospective multicenter validation study was conducted at 4 institutes, including Japanese Circulation Society-certified and uncertified hospitals in Japan. Data on patients with CVDs in departmental lists or with International Classification of Diseases, 10th Revision (ICD-10) codes for CVDs hospitalized between April 2018 and March 2019 were extracted. We examined the sensitivity and positive predictive value of a diagnostic algorithm using ICD-10 codes, medical examinations, and treatments for acute coronary syndrome (ACS), acute heart failure (HF), and acute aortic disease (AAD). We identified 409 patients with ACS (mean age 70.6 years; 24.7% female), 615 patients with acute HF (mean age 77.3 years; 46.2% female), and 122 patients with AAD (mean age 73.4 years; 36.1% female). The respective sensitivity and positive predictive value for the algorithm were 0.86 (95% confidence interval [CI] 0.82–0.89) and 0.95 (95% CI 0.92–0.97) for ACS; 0.74 (95% CI 0.70–0.77) and 0.79 (95% CI 0.76–0.83) for acute HF; and 0.86 (95% CI 0.79–0.92) and 0.83 (95% CI 0.76–0.89) for AAD.Conclusions: The validity of the diagnostic algorithm for Japanese claims data was acceptable. Our results serve as a foundation for future studies on CVDs using nationwide administrative data.
- 著者
- Hiroyuki Tsutsui Shin-ichi Momomura Yoshihiko Saito Hiroshi Ito Kazuhiro Yamamoto Yasushi Sakata Akshay Suvas Desai Tomomi Ohishi Takayuki Iimori Toshihito Kitamura Weinong Guo on behalf of the PARALLEL-HF Investigators
- 出版者
- The Japanese Circulation Society
- 雑誌
- Circulation Journal (ISSN:13469843)
- 巻号頁・発行日
- pp.CJ-20-0854, (Released:2021-03-16)
- 参考文献数
- 21
- 被引用文献数
- 37
Background:In the Prospective Comparison of angiotensin receptor neprilysin inhibitor (ARNI) With ACEi to Determine Impact on Global Mortality and Morbidity in Heart Failure (PARADIGM-HF) study, treatment with sacubitril/valsartan reduced the primary outcome of cardiovascular (CV) death and heart failure (HF) hospitalization compared with enalapril in patients with chronic HF and reduced ejection fraction (HFrEF). A prospective randomized trial was conducted to assess the efficacy and safety of sacubitril/valsartan in Japanese HFrEF patients.Methods and Results:In the Prospective comparison of ARNI with ACEi to determine the noveL beneficiaL trEatment vaLue in Japanese Heart Failure patients (PARALLEL-HF) study, 225 Japanese HFrEF patients (New York Heart Association [NYHA] class II–IV, left ventricular ejection fraction [LVEF] ≤35%) were randomized (1 : 1) to receive sacubitril/valsartan 200 mg bid or enalapril 10 mg bid. Over a median follow up of 33.9 months, no significant between-group difference was observed for the primary composite outcome of CV death and HF hospitalization (HR 1.09; 95% CI 0.65–1.82; P=0.6260). Early and sustained reductions in N-terminal pro-brain natriuretic peptide (NT-proBNP) from baseline were observed with sacubitril/valsartan compared with enalapril (between-group difference: Week 2: 25.7%, P<0.01; Month 6: 18.9%, P=0.01, favoring sacubitril/valsartan). There was no significant difference in the changes in NYHA class and Kansas City Cardiomyopathy Questionnaire (KCCQ) clinical summary score at Week 8 and Month 6. Sacubitril/valsartan was well tolerated with fewer study drug discontinuations due to adverse events, although the sacubitril/valsartan group had a higher proportion of patients with hypotension.Conclusions:In Japanese patients with HFrEF, there was no difference in reduction in the risk of CV death or HF hospitalization between sacubitril/valsartan and enalapril, and sacubitril/valsartan was safe and well tolerated.
- 著者
- Hiroyuki Tsutsui Shin-ichi Momomura Yoshihiko Saito Hiroshi Ito Kazuhiro Yamamoto Yasushi Sakata Tomomi Ohishi Takayuki Iimori Toshihito Kitamura on behalf of the PARALLEL-HF Investigators
- 出版者
- The Japanese Circulation Society
- 雑誌
- Circulation Journal (ISSN:13469843)
- 巻号頁・発行日
- pp.CJ-23-0349, (Released:2023-11-21)
- 参考文献数
- 18
Background: Lower systolic blood pressure (SBP) is known to be associated with poor prognosis in heart failure (HF). We evaluated the efficacy and safety of sacubitril/valsartan according to baseline SBP tertiles in Japanese patients from the PARALLEL-HF study.Methods and Results: In all, 223 patients were stratified into tertiles according to baseline SBP (≤114 mmHg: n=75; >114 and ≤130 mmHg: n=76; and >130 mmHg: n=72). Patients with lower SBP (≤114 mmHg) had the highest median N-terminal pro B-type natriuretic peptide (NT-proBNP) concentrations at baseline (P=0.0184). No significant difference was observed between sacubitril/valsartan and enalapril for the composite outcome of cardiovascular death and HF hospitalization across SBP tertiles (P-interaction=0.2682). Although the P-interaction value was not significant (0.2106), a greater reduction in NT-proBNP with sacubitril/valsartan compared with enalapril was observed in patients with SBP >130 mmHg (P=0.0076). The incidence of hypotension-related events and reduction or discontinuation of treatment due to hypotension-related events was higher in the lower SBP subgroup, and these events were more frequent in the sacubitril/valsartan than enalapril group.Conclusions: The efficacy of sacubitril/valsartan compared with enalapril was consistent across baseline SBP tertiles in Japanese patients from the PARALLEL-HF study. Hypotension-related events were more common in patients treated with sacubitril/valsartan with lower SBP.
- 著者
- Koichiro Kinugawa Yasushi Sakata Minoru Ono Shinichi Nunoda Koichi Toda Norihide Fukushima Akira Shiose Shogo Oishi Dai Yumino Teruhiko Imamura Miyoko Endo Yumiko Hori Koichi Kashiwa Kaoruko Aita Hiroyuki Kojin Yutaka Tejima Yoshiki Sawa
- 出版者
- The Japanese Circulation Society
- 雑誌
- Circulation Journal (ISSN:13469843)
- 巻号頁・発行日
- vol.85, no.10, pp.1906-1917, 2021-09-24 (Released:2021-09-24)
- 参考文献数
- 21
- 被引用文献数
- 11
Destination therapy (DT) is the indication to implant a left ventricular assist device (LVAD) in a patient with stage D heart failure who is not a candidate for heart transplantation. The implantable LVAD has been utilized in Japan since 2011 under the indication of bridge to transplant (BTT). After almost 10 year lag, DT has finally been approved and reimbursed in May 2021 in Japan. To initiate the DT program in Japan, revision of the LVAD indication from BTT is necessary. Also, in-depth discussion of caregiver issues as well as end-of-life care is indispensable. For that purpose, we assembled a DT committee of multidisciplinary members in August 2020, and started monthly discussions via web-based communication during the COVID-19 pandemic. This is a summary of the consensus reached after 6 months’ discussion, and we have included as many relevant topics as possible. Clinical application of DT has just started, and we are willing to revise this consensus to meet the forthcoming issues raised during real-world clinical experience.
- 著者
- Toshiyuki Nagai Takayuki Inomata Takashi Kohno Takuma Sato Atsushi Tada Toru Kubo Kazufumi Nakamura Noriko Oyama-Manabe Yoshihiko Ikeda Takeo Fujino Yasuhide Asaumi Takahiro Okumura Toshiyuki Yano Kazuko Tajiri Hiroyuki Matsuura Yuichi Baba Haruki Sunami Shingo Tsujinaga Yasutoshi Ota Keiko Ohta-Ogo Yusuke Ishikawa Hideo Matama Nobutaka Nagano Kimi Sato Kazushi Yasuda Yasushi Sakata Koichiro Kuwahara Tohru Minamino Minoru Ono Toshihisa Anzai on behalf of the Japanese Circulation Society Joint Working Group
- 出版者
- The Japanese Circulation Society
- 雑誌
- Circulation Journal (ISSN:13469843)
- 巻号頁・発行日
- pp.CJ-22-0696, (Released:2023-03-10)
- 被引用文献数
- 17
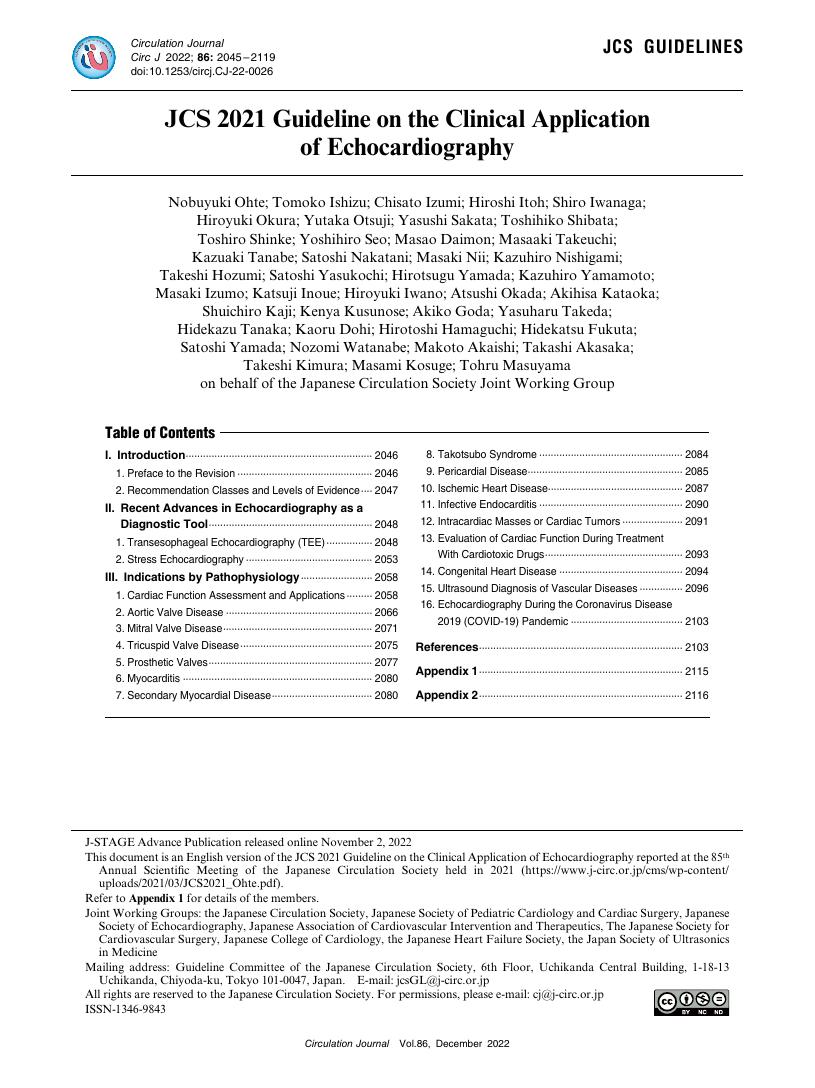
- 著者
- Nobuyuki Ohte Tomoko Ishizu Chisato Izumi Hiroshi Itoh Shiro Iwanaga Hiroyuki Okura Yutaka Otsuji Yasushi Sakata Toshihiko Shibata Toshiro Shinke Yoshihiro Seo Masao Daimon Masaaki Takeuchi Kazuaki Tanabe Satoshi Nakatani Masaki Nii Kazuhiro Nishigami Takeshi Hozumi Satoshi Yasukochi Hirotsugu Yamada Kazuhiro Yamamoto Masaki Izumo Katsuji Inoue Hiroyuki Iwano Atsushi Okada Akihisa Kataoka Shuichiro Kaji Kenya Kusunose Akiko Goda Yasuharu Takeda Hidekazu Tanaka Kaoru Dohi Hirotoshi Hamaguchi Hidekatsu Fukuta Satoshi Yamada Nozomi Watanabe Makoto Akaishi Takashi Akasaka Takeshi Kimura Masami Kosuge Tohru Masuyama on behalf of the Japanese Circulation Society Joint Working Group
- 出版者
- The Japanese Circulation Society
- 雑誌
- Circulation Journal (ISSN:13469843)
- 巻号頁・発行日
- vol.86, no.12, pp.2045-2119, 2022-11-25 (Released:2022-11-25)
- 参考文献数
- 460
- 被引用文献数
- 16
5 0 0 0 OA Efficacy and Safety of Ivabradine in Japanese Patients With Chronic Heart Failure ― J-SHIFT Study ―
- 著者
- Hiroyuki Tsutsui Shin-ichi Momomura Akira Yamashina Hiroaki Shimokawa Yasuki Kihara Yoshihiko Saito Nobuhisa Hagiwara Hiroshi Ito Masafumi Yano Kazuhiro Yamamoto Junya Ako Takayuki Inomata Yasushi Sakata Takashi Tanaka Yasushi Kawasaki on behalf of the J-SHIFT Study Investigators
- 出版者
- The Japanese Circulation Society
- 雑誌
- Circulation Journal (ISSN:13469843)
- 巻号頁・発行日
- pp.CJ-19-0227, (Released:2019-08-08)
- 参考文献数
- 18
- 被引用文献数
- 24 49
Background:Increased heart rate (HR) is an independent risk factor for cardiovascular outcomes in chronic heart failure (HF). Ivabradine, anIfinhibitor, improved outcomes in patients with HF and reduced ejection fraction (HFrEF) in the SHIFT study. We evaluated its efficacy and safety in Japanese HFrEF patients in a randomized, double-blind, placebo-controlled phase III study: the J-SHIFT study. The main objective was to confirm a hazard ratio of <1 in the primary composite endpoint of cardiovascular death or hospital admission for worsening HF.Methods and Results:Patients with NYHA functional class II–IV, left ventricular EF ≤35%, and resting HR ≥75 beats/min in sinus rhythm under optimal medical therapy received ivabradine (n=127) or placebo (n=127). Mean reduction in resting HR was significantly greater in the ivabradine group (15.2 vs. 6.1 beats/min, P<0.0001). However, symptomatic bradycardia did not occur. A total of 26 (20.5%) patients in the ivabradine group and 37 (29.1%) patients in the placebo group had the primary endpoint event (hazard ratio 0.67, 95% CI 0.40–1.11, P=0.1179) during median follow-up of 589 days. Mild phosphenes were reported in 8 (6.3%) patients in the ivabradine group and 4 (3.1%) patients in the placebo group (P=0.3760).Conclusions:The J-SHIFT study supported the efficacy and safety of ivabradine for Japanese HFrEF patients, in accord with the SHIFT study.
- 著者
- Takashi Kuragaichi Yuma Kurozumi Shogo Ohishi Yasuo Sugano Akihiro Sakashita Norihiko Kotooka Makoto Suzuki Taiki Higo Dai Yumino Yasuko Takada Seiko Maeda Saori Yamabe Koichi Washida Tomonori Takahashi Tomohito Ohtani Yasushi Sakata Yukihito Sato
- 出版者
- The Japanese Circulation Society
- 雑誌
- Circulation Journal (ISSN:13469843)
- 巻号頁・発行日
- pp.CJ-17-1305, (Released:2018-03-10)
- 参考文献数
- 45
- 被引用文献数
- 26
Background:Palliative care for heart failure (HF) patients is recommended in Western guidelines, so this study aimed to clarify the current status of palliative care for HF patients in Japan.Methods and Results:A survey was sent to all Japanese Circulation Society-authorized cardiology training hospitals (n=1,004) in August 2016. A total of 544 institutions (54%) returned the questionnaire. Of them, 527 (98%) answered that palliative care is necessary for patients with HF. A total of 227 (42%) institutions held a palliative care conference for patients with HF, and 79% of the institutions had <10 cases per year. Drug therapy as palliative care was administered at 403 (76%) institutions; morphine (87%) was most frequently used. Among sedatives, dexmedetomidine (33%) was administered more often than midazolam (29%) or propofol (20%). Regarding the timing of end-of-life care, most institutions (84%) reported having considered palliative care when a patient reached the terminal stage of HF. Most frequently, the reason for the decision at the terminal stage was “difficulty in discontinuing cardiotonics.” A major impediment to the delivery of palliative care was “difficulty predicting an accurate prognosis.”Conclusions:This large-scale survey showed the characteristics of palliative care for HF in Japan. The present findings may aid in the development of effective end-of-life care systems.
- 著者
- Teruhiko Imamura Koichiro Kinugawa Takashi Nishimura Koichi Toda Yoshikatsu Saiki Hiroshi Niinami Shinichi Nunoda Goro Matsumiya Motonobu Nishimura Hirokuni Arai Masanobu Yanase Norihide Fukushima Takeshi Nakatani Akira Shiose Ikuko Shibasaki Yasushi Sakata Minoru Ono J-MACS Investigators
- 出版者
- The Japanese Circulation Society
- 雑誌
- Circulation Journal (ISSN:13469843)
- 巻号頁・発行日
- pp.CJ-23-0264, (Released:2023-06-01)
- 参考文献数
- 18
- 被引用文献数
- 2
Background: Recently, destination therapy (DT) was approved in Japan, and patients ineligible for heart transplantation may now receive durable left ventricular assist devices (LVADs). Several conventional risk scores are available, but a risk score that is best to select optimal candidates for DT in the Japanese population remains unestablished.Methods and Results: A total of 1,287 patients who underwent durable LVAD implantation and were listed for the Japanese registry for Mechanically Assisted Circulatory Support (J-MACS) were eligible for inclusion. Finally, 494 patients were assigned to the derivation cohort and 487 patients were assigned to the validation cohort. According to the time-to-event analyses, J-MACS risk scores were newly constructed to predict 3-year mortality rate, consisting of age, history of cardiac surgery, serum creatinine level, and central venous pressure to pulmonary artery wedge pressure ratio >0.71. The J-MACS risk score had the highest predictability of 3-year death compared with other conventional scores in the validation cohort, including HeartMate II risk score and HeartMate 3 risk score.Conclusions: We constructed the J-MACS risk score to estimate 3-year mortality rate after durable LVAD implantation using large-scale multicenter Japanese data. The clinical utility of this scoring to guide the indication of DT should be validated in the next study.
- 著者
- Junya Tanabe Hiraku Murakami Yasuhiro Akazawa Daisuke Nakamura Fusako Sera Takahumi Oka Kentaro Fukushima Tomohito Ohtani Naoki Hosen Yasushi Sakata
- 出版者
- The Japanese Circulation Society
- 雑誌
- Circulation Reports (ISSN:24340790)
- 巻号頁・発行日
- pp.CR-23-0023, (Released:2023-05-31)