- 著者
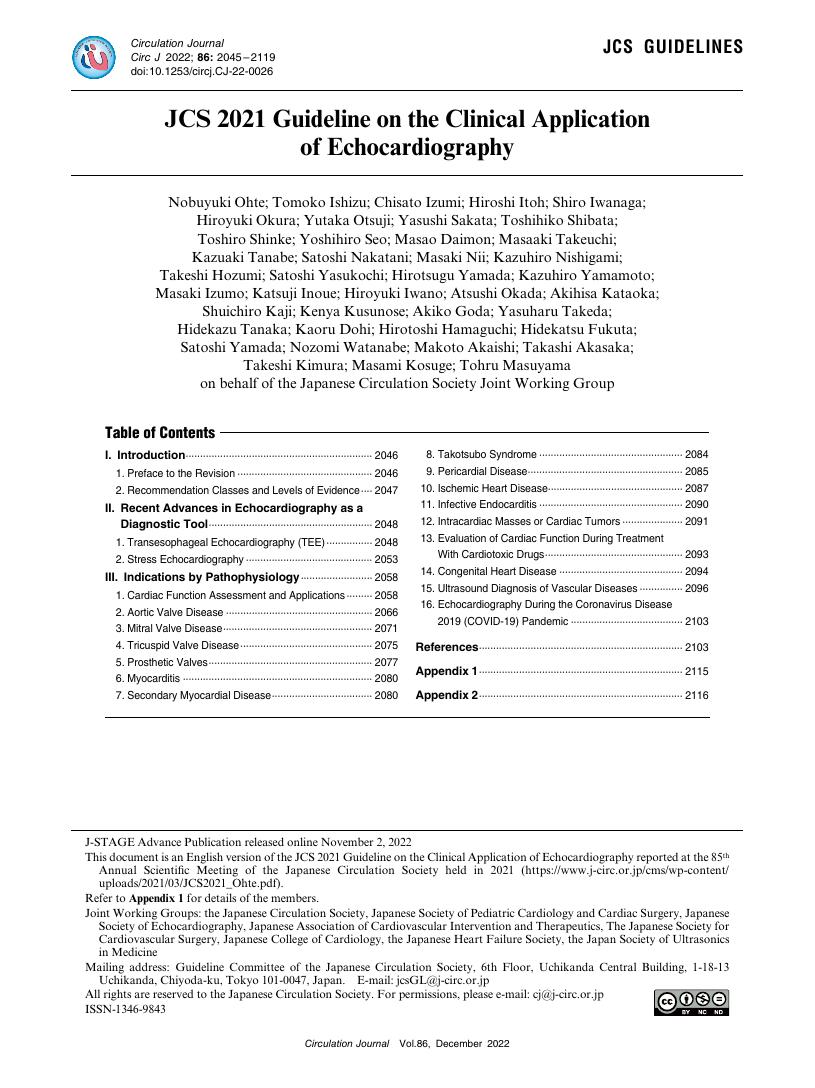
- Nobuyuki Ohte Tomoko Ishizu Chisato Izumi Hiroshi Itoh Shiro Iwanaga Hiroyuki Okura Yutaka Otsuji Yasushi Sakata Toshihiko Shibata Toshiro Shinke Yoshihiro Seo Masao Daimon Masaaki Takeuchi Kazuaki Tanabe Satoshi Nakatani Masaki Nii Kazuhiro Nishigami Takeshi Hozumi Satoshi Yasukochi Hirotsugu Yamada Kazuhiro Yamamoto Masaki Izumo Katsuji Inoue Hiroyuki Iwano Atsushi Okada Akihisa Kataoka Shuichiro Kaji Kenya Kusunose Akiko Goda Yasuharu Takeda Hidekazu Tanaka Kaoru Dohi Hirotoshi Hamaguchi Hidekatsu Fukuta Satoshi Yamada Nozomi Watanabe Makoto Akaishi Takashi Akasaka Takeshi Kimura Masami Kosuge Tohru Masuyama on behalf of the Japanese Circulation Society Joint Working Group
- 出版者
- The Japanese Circulation Society
- 雑誌
- Circulation Journal (ISSN:13469843)
- 巻号頁・発行日
- vol.86, no.12, pp.2045-2119, 2022-11-25 (Released:2022-11-25)
- 参考文献数
- 460
- 被引用文献数
- 16
- 著者
- Shingo Tsujinaga Hiroyuki Iwano Yasuyuki Chiba Suguru Ishizaka Miwa Sarashina Michito Murayama Masahiro Nakabachi Hisao Nishino Shinobu Yokoyama Kazunori Okada Sanae Kaga Toshihisa Anzai
- 出版者
- The Japanese Circulation Society
- 雑誌
- Circulation Reports (ISSN:24340790)
- 巻号頁・発行日
- vol.2, no.5, pp.271-279, 2020-05-08 (Released:2020-05-08)
- 参考文献数
- 27
- 被引用文献数
- 3
Background:Ventilatory inefficiency during exercise assessed using the lowest minute ventilation/carbon dioxide production (V̇E/V̇CO2) ratio was recently proven to be a strong prognostic marker of heart failure (HF) regardless of left ventricular ejection fraction (LVEF). Its physiological background, however, has not been elucidated.Methods and Results:Fifty-seven HF patients underwent cardiopulmonary exercise testing and exercise-stress echocardiography. The lowest V̇E/V̇CO2ratio was assessed on respiratory gas analysis. Echocardiography was obtained at rest and at peak exercise. LVEF was measured using the method of disks. Cardiac output (CO) and the ratio of transmitral early filling velocity (E) to early diastolic tissue velocity (e’) were calculated using the Doppler method. HF patients were divided into preserved EF (HFpEF) and reduced EF (HFrEF) using the LVEF cut-off 40% at rest. Twenty-four patients were classified as HFpEF and 33 as HFrEF. In HFpEF, age (r=0.58), CO (r=−0.44), e’ (r=−0.48) and E/e’ (r=0.45) during exercise correlated with the lowest V̇E/V̇CO2ratio (P<0.05 for all). In contrast, in HFrEF, age (r=0.47) and CO (r=−0.54) during exercise, but not e’ and E/e’, correlated with the lowest V̇E/V̇CO2ratio.Conclusions:Loss of CO augmentation was associated with ventilatory inefficiency in HF regardless of LVEF, although lung congestion determined ventilatory efficiency only in HFpEF.
- 著者
- Michito Murayama Hiroyuki Iwano Miwa Sarashina Toshihisa Anzai
- 出版者
- The Japanese Circulation Society
- 雑誌
- Circulation Journal (ISSN:13469843)
- 巻号頁・発行日
- pp.CJ-20-0678, (Released:2020-09-24)
- 被引用文献数
- 2
- 著者
- Kazuhiro Koyanagawa Yuta Kobayashi Tadao Aikawa Atsuhito Takeda Hideaki Shiraishi Satonori Tsuneta Noriko Oyama-Manabe Hiroyuki Iwano Toshiyuki Nagai Toshihisa Anzai
- 出版者
- Japanese Society for Magnetic Resonance in Medicine
- 雑誌
- Magnetic Resonance in Medical Sciences (ISSN:13473182)
- 巻号頁・発行日
- pp.bc.2020-0069, (Released:2020-09-07)
- 参考文献数
- 18
- 被引用文献数
- 1
To assess myocardial fibrosis associated with muscular dystrophy, T1-mapping and extracellular volume fraction (ECV) quantification was prospectively performed using cardiovascular MR (CMR) imaging in 6 male patients with muscular dystrophy and 5 female putative carriers of Duchenne or Becker muscular dystrophy. Five patients and all putative carriers had an elevated ECV (>29.5% for men and >35.2% for women), suggesting that ECV has a potential to detect diffuse fibrotic changes in patients and putative carriers of muscular dystrophy.
- 著者
- Taro Temma Toshiyuki Nagai Masaya Watanabe Rui Kamada Yumi Takahashi Hikaru Hagiwara Taro Koya Motoki Nakao Kazunori Omote Kiwamu Kamiya Hiroyuki Iwano Kazuhiro Yamamoto Tsutomu Yoshikawa Yoshihiko Saito Toshihisa Anzai
- 出版者
- The Japanese Circulation Society
- 雑誌
- Circulation Journal (ISSN:13469843)
- 巻号頁・発行日
- pp.CJ-19-0963, (Released:2020-02-01)
- 参考文献数
- 31
- 被引用文献数
- 9
Background:Atrial fibrillation (AF) is an important prognostic determinant in heart failure (HF) with preserved ejection fraction (HFpEF). However, it is unclear which HFpEF phenotypes are affected by AF in terms of long-term clinical outcomes because HFpEF is a heterogeneous syndrome with comorbidities such as coronary artery disease (CAD). In this study we determined the differential prognostic significance of AF in HFpEF patients according to CAD status.Methods and Results:Data for 408 hospitalized HFpEF patients enrolled in the Japanese Heart Failure Syndrome with Preserved Ejection Fraction Nationwide Multicenter Registry were analyzed. Patients were divided into 4 groups according to the presence of AF and CAD. The primary outcome was the composite of all-cause death and HF rehospitalization. The incidence of adverse events was higher in the AF–non-CAD than non-AF–non-CAD group (P=0.004). On multivariable Cox regression analysis with prespecified confounders, AF–non-CAD was significantly associated with an increased risk of adverse events than non-AF–non-CAD (adjusted HR, 1.91; 95% CI: 1.02–3.92) regardless of the type of AF. In contrast, risk was comparable between the AF–CAD and non-AF–CAD groups (adjusted HR, 1.24; 95% CI: 0.64–2.47).Conclusions:In HFpEF patients without CAD, AF was independently related to adverse events, indicating that intensive management of AF would have more beneficial effects particularly in HFpEF patients without CAD.
- 著者
- Michito Murayama Hiroyuki Iwano Miwa Sarashina Toshihisa Anzai
- 出版者
- The Japanese Circulation Society
- 雑誌
- Circulation Journal (ISSN:13469843)
- 巻号頁・発行日
- vol.84, no.11, pp.2036, 2020-10-23 (Released:2020-10-23)
- 被引用文献数
- 2
- 著者
- Hirokazu Komoriyama Kiwamu Kamiya Yuta Kobayashi Satonori Tsuneta Takao Konishi Takuma Sato Hiroyuki Iwano Toshiyuki Nagai Satoru Wakasa Kohsuke Kudo Toshihisa Anzai
- 出版者
- The Japanese Circulation Society
- 雑誌
- Circulation Journal (ISSN:13469843)
- 巻号頁・発行日
- pp.CJ-20-1248, (Released:2021-04-03)
- 著者
- Takashi Yoshitani Naoya Asakawa Mamoru Sakakibara Keiji Noguchi Yusuke Tokuda Kiwamu Kamiya Hiroyuki Iwano Satoshi Yamada Yusuke Kudou Mutsumi Nishida Chikara Shimizu Toraji Amano Hiroyuki Tsutsui
- 出版者
- The Japanese Circulation Society
- 雑誌
- Circulation Journal (ISSN:13469843)
- 巻号頁・発行日
- vol.80, no.5, pp.1187-1195, 2016-04-25 (Released:2016-04-25)
- 参考文献数
- 31
- 被引用文献数
- 13 25
Background:Heart failure (HF) causes organ congestion, which is thought to increase organ stiffness. The virtual touch quantification (VTQ) method can be used to assess liver stiffness in patients with chronic liver diseases. This study aimed to measure liver and kidney stiffness using VTQ and to determine its value for assessing organ congestion in patients with HF.Methods and Results:This study included 10 normal subjects and 38 HF patients (age 52.3±16.7 years, left ventricular ejection fraction 27.0±9.4%, plasma B-type natriuretic peptide [BNP] 1,297.3±1,155.1 pg/ml). We investigated the relationships between clinical characteristics and hemodynamics and liver and kidney stiffness, and assessed the effects of medical treatment on these measurements. Liver stiffness was significantly higher in HF patients (1.17±0.13 m/s vs. 2.03±0.91 m/s, P=0.004) compared with normal subjects, but kidney stiffness was similar in both groups. Central venous pressure (CVP) (P=0.021) and BNP (P=0.025) were independent predictive factors for increased liver stiffness in HF patients. Liver stiffness decreased significantly from 2.37±1.09 to 1.27±0.33 m/s (P<0.001) after treatment. Changes in liver stiffness in HF patients significantly correlated with changes in CVP (R=0.636, P=0.014) and cardiac index (R=−0.557, P=0.039) according to univariate analysis, and with changes in CVP in multivariate analysis.Conclusions:Liver stiffness measured by noninvasive VTQ methods can be used to assess liver congestion and therapeutic effects in patients with HF. (Circ J 2016; 80: 1187–1195)