- 著者
- Hiroyuki Tsutsui Mitsuaki Isobe Hiroshi Ito Hiroshi Ito Ken Okumura Minoru Ono Masafumi Kitakaze Koichiro Kinugawa Yasuki Kihara Yoichi Goto Issei Komuro Yoshikatsu Saiki Yoshihiko Saito Yasushi Sakata Naoki Sato Yoshiki Sawa Akira Shiose Wataru Shimizu Hiroaki Shimokawa Yoshihiko Seino Koichi Node Taiki Higo Atsushi Hirayama Miyuki Makaya Tohru Masuyama Toyoaki Murohara Shin-ichi Momomura Masafumi Yano Kenji Yamazaki Kazuhiro Yamamoto Tsutomu Yoshikawa Michihiro Yoshimura Masatoshi Akiyama Toshihisa Anzai Shiro Ishihara Takayuki Inomata Teruhiko Imamura Yu-ki Iwasaki Tomohito Ohtani Katsuya Onishi Takatoshi Kasai Mahoto Kato Makoto Kawai Yoshiharu Kinugasa Shintaro Kinugawa Toru Kuratani Shigeki Kobayashi Yasuhiko Sakata Atsushi Tanaka Koichi Toda Takashi Noda Kotaro Nochioka Masaru Hatano Takayuki Hidaka Takeo Fujino Shigeru Makita Osamu Yamaguchi Uichi Ikeda Takeshi Kimura Shun Kohsaka Masami Kosuge Masakazu Yamagishi Akira Yamashina on behalf of the Japanese Circulation Society and the Japanese Heart Failure Society Joint Working Group
- 出版者
- The Japanese Circulation Society
- 雑誌
- Circulation Journal (ISSN:13469843)
- 巻号頁・発行日
- vol.83, no.10, pp.2084-2184, 2019-09-25 (Released:2019-09-25)
- 参考文献数
- 608
- 被引用文献数
- 435
25 0 0 0 OA Superiority of Long-Acting to Short-Acting Loop Diuretics in the Treatment of Congestive Heart Failure
- 著者
- Tohru Masuyama Takeshi Tsujino Hideki Origasa Kazuhiro Yamamoto Takashi Akasaka Yutaka Hirano Nobuyuki Ohte Takashi Daimon Satoshi Nakatani Hiroshi Ito
- 出版者
- The Japanese Circulation Society
- 雑誌
- Circulation Journal (ISSN:13469843)
- 巻号頁・発行日
- vol.76, no.4, pp.833-842, 2012 (Released:2012-03-23)
- 参考文献数
- 30
- 被引用文献数
- 46 49
Background: Diuretics are the most prescribed drug in heart failure (HF) patients. However, clinical evidence about their long-term effects is lacking. The purpose of this study was to compare the therapeutic effects of furosemide and azosemide, a short- and long-acting loop diuretic, respectively, in patients with chronic heart failure (CHF). Methods and Results: In this multicenter, prospective, randomized, open, blinded endpoint trial, we compared the effects of azosemide and furosemide in patients with CHF and New York Heart Association class II or III symptoms. 320 patients (160 patients in each group, mean age 71 years) were followed up for a minimum of 2 years. The primary endpoint was a composite of cardiovascular death or unplanned admission to hospital for congestive HF. During a median follow-up of 35.2 months, the primary endpoint occurred in 23 patients in the azosemide group and in 34 patients in the furosemide group (hazard ratio [HR], 0.55, 95% confidence interval [CI] 0.32-0.95: P=0.03). Among the secondary endpoints, unplanned admission to hospital for congestive HF or a need for modification of the treatment for HF were also reduced in the azosemide group compared with the furosemide group (HR, 0.60, 95%CI 0.36-0.99: P=0.048). Conclusions: Azosemide, compared with furosemide, reduced the risk of cardiovascular death or unplanned admission to hospital for congestive HF. (Circ J 2012; 76: 833-842)
22 0 0 0 OA JCS/JHFS 2021 Guideline Focused Update on Diagnosis and Treatment of Acute and Chronic Heart Failure
- 著者
- Hiroyuki Tsutsui Tomomi Ide Hiroshi Ito Yasuki Kihara Koichiro Kinugawa Shintaro Kinugawa Miyuki Makaya Toyoaki Murohara Koichi Node Yoshihiko Saito Yasushi Sakata Wataru Shimizu Kazuhiro Yamamoto Yasuko Bando Yu-ki Iwasaki Yoshiharu Kinugasa Isamu Mizote Hitoshi Nakagawa Shogo Oishi Akiko Okada Atsushi Tanaka Takashi Akasaka Minoru Ono Takeshi Kimura Shun Kosaka Masami Kosuge Shin-ichi Momomura on behalf of the Japanese Circulation Society and the Japanese Heart Failure Society Joint Working Group
- 出版者
- The Japanese Circulation Society
- 雑誌
- Circulation Journal (ISSN:13469843)
- 巻号頁・発行日
- pp.CJ-21-0431, (Released:2021-09-29)
- 参考文献数
- 252
- 被引用文献数
- 84
- 著者
- Minoru Ono Osamu Yamaguchi Tomohito Ohtani Koichiro Kinugawa Yoshikatsu Saiki Yoshiki Sawa Akira Shiose Hiroyuki Tsutsui Norihide Fukushima Goro Matsumiya Masanobu Yanase Kenji Yamazaki Kazuhiro Yamamoto Masatoshi Akiyama Teruhiko Imamura Kiyotaka Iwasaki Miyoko Endo Yoshihiko Ohnishi Takahiro Okumura Koichi Kashiwa Osamu Kinoshita Kaori Kubota Osamu Seguchi Koichi Toda Hiroshi Nishioka Tomohiro Nishinaka Takashi Nishimura Toru Hashimoto Masaru Hatano Haruhiko Higashi Taiki Higo Takeo Fujino Yumiko Hori Toru Miyoshi Motoharu Yamanaka Takayuki Ohno Takeshi Kimura Shunei Kyo Yasushi Sakata Takeshi Nakatani on behalf of the JCS/JSCVS/JATS/JSVS Joint Working Group
- 出版者
- The Japanese Circulation Society
- 雑誌
- Circulation Journal (ISSN:13469843)
- 巻号頁・発行日
- pp.CJ-21-0880, (Released:2022-04-05)
- 参考文献数
- 288
- 被引用文献数
- 10
- 著者
- Toshihisa Anzai Takuma Sato Yoshihiro Fukumoto Chisato Izumi Yoshiyuki Kizawa Masatoshi Koga Katsuji Nishimura Mitsuru Ohishi Akihiro Sakashita Yasushi Sakata Tsuyoshi Shiga Yasuchika Takeishi Satoshi Yasuda Kazuhiro Yamamoto Takahiro Abe Rie Akaho Yasuhiro Hamatani Hayato Hosoda Naoki Ishimori Mika Kato Yoshiharu Kinugasa Takuro Kubozono Toshiyuki Nagai Shogo Oishi Katsuki Okada Tatsuhiro Shibata Atsushi Suzuki Tsuyoshi Suzuki Masahito Takagi Yasuko Takada Kenkichi Tsuruga Akiomi Yoshihisa Dai Yumino Keiichi Fukuda Yasuki Kihara Yoshihiko Saito Yoshiki Sawa Hiroyuki Tsutsui Takeshi Kimura on behalf of the Japanese Circulation Society Joint Working Group
- 出版者
- The Japanese Circulation Society
- 雑誌
- Circulation Journal (ISSN:13469843)
- 巻号頁・発行日
- pp.CJ-20-1127, (Released:2021-03-26)
- 参考文献数
- 316
- 被引用文献数
- 19
- 著者
- Hiroyuki Tsutsui Hiroshi Ito Masafumi Kitakaze Issei Komuro Toyoaki Murohara Tohru Izumi Kenji Sunagawa Yoshio Yasumura Masafumi Yano Kazuhiro Yamamoto Tsutomu Yoshikawa Takayoshi Tsutamoto Junwei Zhang Akifumi Okayama Yoshihiko Ichikawa Kazuhiro Kanmuri Masunori Matsuzaki for the J-EMPHASIS-HF Study Group
- 出版者
- 日本循環器学会
- 雑誌
- Circulation Journal (ISSN:13469843)
- 巻号頁・発行日
- pp.CJ-17-0323, (Released:2017-08-19)
- 参考文献数
- 19
- 被引用文献数
- 23
Background:The mineralocorticoid receptor antagonist eplerenone improved clinical outcomes among patients with heart failure with reduced ejection faction (HFrEF) in the EMPHASIS-HF (Eplerenone in Mild Patients Hospitalization And SurvIval Study in Heart Failure) study. However, similar efficacy and safety have not been established in Japanese patients. We evaluated the efficacy and safety of eplerenone in patients with HFrEF in a multicenter, randomized, double-blind placebo-controlled outcome study (ClinicalTrials.gov Identifier: NCT01115855). The aim of the study was to evaluate efficacy predefined as consistency of the primary endpoint with that of EMPHASIS-HF at a point estimate of <1 for the hazard ratio.Methods and Results:HFrEF patients with NYHA functional class II–IV and an EF ≤35% received eplerenone (n=111) or placebo (n=110) on top of standard therapy for at least 12 months. The primary endpoint was a composite of death from cardiovascular causes or hospitalization for HF. The primary endpoint occurred in 29.7% of patients in the eplerenone group vs. 32.7% in the placebo group [hazard ratio=0.85 (95% CI: 0.53–1.36)]. Hospitalization for any cause and changes in plasma BNP and LVEF were favorable with eplerenone. A total of 17 patients (15.3%) in the eplerenone group and 10 patients (9.1%) in the placebo group died. Adverse events, including hyperkalemia, were similar between the groups.Conclusions:Eplerenone was well-tolerated in Japanese patients with HFrEF and showed results consistent with those reported in the EMPHASIS-HF study.
- 著者
- Hiroyuki Tsutsui Shin-ichi Momomura Yoshihiko Saito Hiroshi Ito Kazuhiro Yamamoto Yasushi Sakata Tomomi Ohishi Pankaj Kumar Toshihito Kitamura
- 出版者
- The Japanese Circulation Society
- 雑誌
- Circulation Journal (ISSN:13469843)
- 巻号頁・発行日
- pp.CJ-23-0174, (Released:2023-08-26)
- 参考文献数
- 38
Background: The PARALLEL-HF study assessed the efficacy and safety of sacubitril/valsartan vs. enalapril in Japanese patients with chronic heart failure with reduced ejection fraction (HFrEF). This open-label extension (OLE) assessed long-term safety with sacubitril/valsartan.Methods and Results: This study enrolled 150 patients who received sacubitril/valsartan 50 or 100 mg, b.i.d., in addition to optimal background heart failure (HF) therapy. A dose level of sacubitril/valsartan 200 mg, b.i.d., was targeted by Week 8. At OLE baseline, higher concentrations of B-type natriuretic peptide (BNP) and urine cGMP, and lower concentrations of N-terminal pro B-type natriuretic peptide (NT-proBNP), were observed in the sacubitril/valsartan core group (patients who received sacubitril/valsartan in both the core and extension study) than in the enalapril core group (patients who received enalapril in the core study and were then transitioned to sacubitril/valsartan). The mean exposure to study drug was 98.9%. There was no trend of worsening of HF at Month 12. No obvious changes in cardiac biomarkers were observed, whereas BNP and urine cGMP increased and NT-proBNP decreased in the enalapril core group, which was evident at Weeks 2–4 and sustained to Month 12.Conclusions: Long-term sacubitril/valsartan at doses up to 200 mg, b.i.d., has a positive risk-benefit profile; it was safe and well tolerated in Japanese patients with chronic HFrEF.
- 著者
- Hiroyuki Tsutsui Shin-ichi Momomura Yoshihiko Saito Hiroshi Ito Kazuhiro Yamamoto Yasushi Sakata Akshay Suvas Desai Tomomi Ohishi Takayuki Iimori Toshihito Kitamura Weinong Guo on behalf of the PARALLEL-HF Investigators
- 出版者
- The Japanese Circulation Society
- 雑誌
- Circulation Journal (ISSN:13469843)
- 巻号頁・発行日
- pp.CJ-20-0854, (Released:2021-03-16)
- 参考文献数
- 21
- 被引用文献数
- 37
Background:In the Prospective Comparison of angiotensin receptor neprilysin inhibitor (ARNI) With ACEi to Determine Impact on Global Mortality and Morbidity in Heart Failure (PARADIGM-HF) study, treatment with sacubitril/valsartan reduced the primary outcome of cardiovascular (CV) death and heart failure (HF) hospitalization compared with enalapril in patients with chronic HF and reduced ejection fraction (HFrEF). A prospective randomized trial was conducted to assess the efficacy and safety of sacubitril/valsartan in Japanese HFrEF patients.Methods and Results:In the Prospective comparison of ARNI with ACEi to determine the noveL beneficiaL trEatment vaLue in Japanese Heart Failure patients (PARALLEL-HF) study, 225 Japanese HFrEF patients (New York Heart Association [NYHA] class II–IV, left ventricular ejection fraction [LVEF] ≤35%) were randomized (1 : 1) to receive sacubitril/valsartan 200 mg bid or enalapril 10 mg bid. Over a median follow up of 33.9 months, no significant between-group difference was observed for the primary composite outcome of CV death and HF hospitalization (HR 1.09; 95% CI 0.65–1.82; P=0.6260). Early and sustained reductions in N-terminal pro-brain natriuretic peptide (NT-proBNP) from baseline were observed with sacubitril/valsartan compared with enalapril (between-group difference: Week 2: 25.7%, P<0.01; Month 6: 18.9%, P=0.01, favoring sacubitril/valsartan). There was no significant difference in the changes in NYHA class and Kansas City Cardiomyopathy Questionnaire (KCCQ) clinical summary score at Week 8 and Month 6. Sacubitril/valsartan was well tolerated with fewer study drug discontinuations due to adverse events, although the sacubitril/valsartan group had a higher proportion of patients with hypotension.Conclusions:In Japanese patients with HFrEF, there was no difference in reduction in the risk of CV death or HF hospitalization between sacubitril/valsartan and enalapril, and sacubitril/valsartan was safe and well tolerated.
- 著者
- Hiroyuki Tsutsui Shin-ichi Momomura Yoshihiko Saito Hiroshi Ito Kazuhiro Yamamoto Yasushi Sakata Tomomi Ohishi Takayuki Iimori Toshihito Kitamura on behalf of the PARALLEL-HF Investigators
- 出版者
- The Japanese Circulation Society
- 雑誌
- Circulation Journal (ISSN:13469843)
- 巻号頁・発行日
- pp.CJ-23-0349, (Released:2023-11-21)
- 参考文献数
- 18
Background: Lower systolic blood pressure (SBP) is known to be associated with poor prognosis in heart failure (HF). We evaluated the efficacy and safety of sacubitril/valsartan according to baseline SBP tertiles in Japanese patients from the PARALLEL-HF study.Methods and Results: In all, 223 patients were stratified into tertiles according to baseline SBP (≤114 mmHg: n=75; >114 and ≤130 mmHg: n=76; and >130 mmHg: n=72). Patients with lower SBP (≤114 mmHg) had the highest median N-terminal pro B-type natriuretic peptide (NT-proBNP) concentrations at baseline (P=0.0184). No significant difference was observed between sacubitril/valsartan and enalapril for the composite outcome of cardiovascular death and HF hospitalization across SBP tertiles (P-interaction=0.2682). Although the P-interaction value was not significant (0.2106), a greater reduction in NT-proBNP with sacubitril/valsartan compared with enalapril was observed in patients with SBP >130 mmHg (P=0.0076). The incidence of hypotension-related events and reduction or discontinuation of treatment due to hypotension-related events was higher in the lower SBP subgroup, and these events were more frequent in the sacubitril/valsartan than enalapril group.Conclusions: The efficacy of sacubitril/valsartan compared with enalapril was consistent across baseline SBP tertiles in Japanese patients from the PARALLEL-HF study. Hypotension-related events were more common in patients treated with sacubitril/valsartan with lower SBP.
- 著者
- Kazuhiro Yamamoto Miyuki Tsuchihashi-Makaya Yoshiharu Kinugasa Yuki Iida Kentaro Kamiya Yasuki Kihara Yuji Kono Yukihito Sato Norio Suzuki Harumi Takeuchi Taiki Higo Yasushi Miyazawa Isao Miyajima Akira Yamashina Katsushi Yoshita Koichi Washida Masafumi Kuzuya Tetsuya Takahashi Yutaka Nakaya Naoyuki Hasebe Hiroyuki Tsutsui on behalf of The Japanese Heart Failure Society Expert Consensus Writing Committee
- 出版者
- The Japanese Circulation Society
- 雑誌
- Circulation Journal (ISSN:13469843)
- 巻号頁・発行日
- pp.CJ-20-0322, (Released:2020-07-10)
- 参考文献数
- 206
- 被引用文献数
- 21
- 著者
- Hideo Izawa Toshiko Yoshida Toshimi Ikegame Kazuhiro P. Izawa Yoshihiro Ito Hideo Okamura Naohiko Osada Shintaro Kinugawa Takuro Kubozono Yuji Kono Kiyonori Kobayashi Kazuhiko Nishigaki Taiki Higo Akihiro Hirashiki Yasushi Miyazawa Yuji Morio Masanobu Yanase Sumio Yamada Hisao Ikeda Shin-ichi Momomura Yasuki Kihara Kazuhiro Yamamoto Yoichi Goto Shigeru Makita the Japanese Association of Cardiac Rehabilitation Standard Cardiac Rehabilitation Program Planning Committee
- 出版者
- The Japanese Circulation Society
- 雑誌
- Circulation Journal (ISSN:13469843)
- 巻号頁・発行日
- pp.CJ-19-0670, (Released:2019-11-09)
- 参考文献数
- 21
- 被引用文献数
- 52
- 著者
- Akihiro Okamura Masaru Kato Takuya Tomomori Aiko Takami Shunsuke Kawatani Kazuhiro Yamamoto
- 出版者
- The Japanese Circulation Society
- 雑誌
- Circulation Journal (ISSN:13469843)
- 巻号頁・発行日
- pp.CJ-23-0069, (Released:2023-04-11)
- 参考文献数
- 2
- 著者
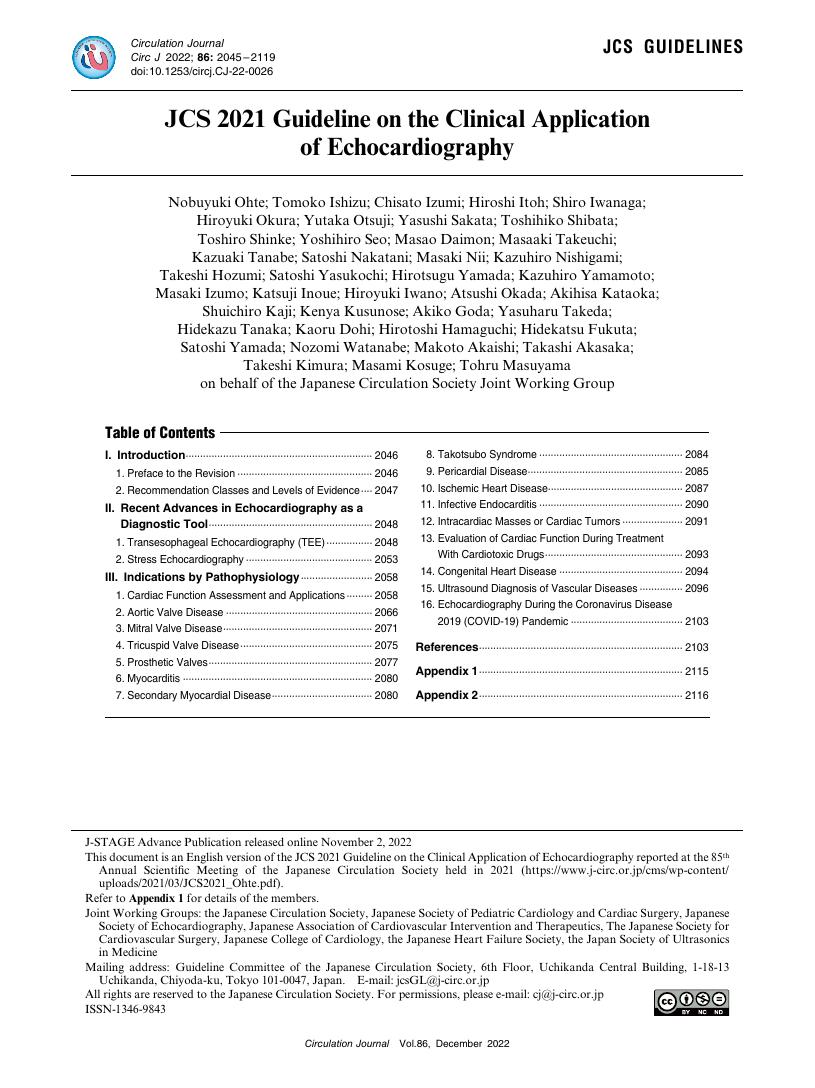
- Nobuyuki Ohte Tomoko Ishizu Chisato Izumi Hiroshi Itoh Shiro Iwanaga Hiroyuki Okura Yutaka Otsuji Yasushi Sakata Toshihiko Shibata Toshiro Shinke Yoshihiro Seo Masao Daimon Masaaki Takeuchi Kazuaki Tanabe Satoshi Nakatani Masaki Nii Kazuhiro Nishigami Takeshi Hozumi Satoshi Yasukochi Hirotsugu Yamada Kazuhiro Yamamoto Masaki Izumo Katsuji Inoue Hiroyuki Iwano Atsushi Okada Akihisa Kataoka Shuichiro Kaji Kenya Kusunose Akiko Goda Yasuharu Takeda Hidekazu Tanaka Kaoru Dohi Hirotoshi Hamaguchi Hidekatsu Fukuta Satoshi Yamada Nozomi Watanabe Makoto Akaishi Takashi Akasaka Takeshi Kimura Masami Kosuge Tohru Masuyama on behalf of the Japanese Circulation Society Joint Working Group
- 出版者
- The Japanese Circulation Society
- 雑誌
- Circulation Journal (ISSN:13469843)
- 巻号頁・発行日
- vol.86, no.12, pp.2045-2119, 2022-11-25 (Released:2022-11-25)
- 参考文献数
- 460
- 被引用文献数
- 16
5 0 0 0 OA Efficacy and Safety of Ivabradine in Japanese Patients With Chronic Heart Failure ― J-SHIFT Study ―
- 著者
- Hiroyuki Tsutsui Shin-ichi Momomura Akira Yamashina Hiroaki Shimokawa Yasuki Kihara Yoshihiko Saito Nobuhisa Hagiwara Hiroshi Ito Masafumi Yano Kazuhiro Yamamoto Junya Ako Takayuki Inomata Yasushi Sakata Takashi Tanaka Yasushi Kawasaki on behalf of the J-SHIFT Study Investigators
- 出版者
- The Japanese Circulation Society
- 雑誌
- Circulation Journal (ISSN:13469843)
- 巻号頁・発行日
- pp.CJ-19-0227, (Released:2019-08-08)
- 参考文献数
- 18
- 被引用文献数
- 24 49
Background:Increased heart rate (HR) is an independent risk factor for cardiovascular outcomes in chronic heart failure (HF). Ivabradine, anIfinhibitor, improved outcomes in patients with HF and reduced ejection fraction (HFrEF) in the SHIFT study. We evaluated its efficacy and safety in Japanese HFrEF patients in a randomized, double-blind, placebo-controlled phase III study: the J-SHIFT study. The main objective was to confirm a hazard ratio of <1 in the primary composite endpoint of cardiovascular death or hospital admission for worsening HF.Methods and Results:Patients with NYHA functional class II–IV, left ventricular EF ≤35%, and resting HR ≥75 beats/min in sinus rhythm under optimal medical therapy received ivabradine (n=127) or placebo (n=127). Mean reduction in resting HR was significantly greater in the ivabradine group (15.2 vs. 6.1 beats/min, P<0.0001). However, symptomatic bradycardia did not occur. A total of 26 (20.5%) patients in the ivabradine group and 37 (29.1%) patients in the placebo group had the primary endpoint event (hazard ratio 0.67, 95% CI 0.40–1.11, P=0.1179) during median follow-up of 589 days. Mild phosphenes were reported in 8 (6.3%) patients in the ivabradine group and 4 (3.1%) patients in the placebo group (P=0.3760).Conclusions:The J-SHIFT study supported the efficacy and safety of ivabradine for Japanese HFrEF patients, in accord with the SHIFT study.
- 著者
- Yoshiharu Kinugasa Masahiko Kato Shinobu Sugihara Masayuki Hirai Kensaku Yamada Kiyotaka Yanagihara Kazuhiro Yamamoto
- 出版者
- The Japanese Circulation Society
- 雑誌
- Circulation Journal (ISSN:13469843)
- 巻号頁・発行日
- vol.77, no.3, pp.705-711, 2013 (Released:2013-02-25)
- 参考文献数
- 32
- 被引用文献数
- 92 208 15
Background: The clinical significance of nutritional risk assessment in patients with heart failure with preserved ejection fraction (HFpEF) remains undefined. Geriatric nutritional risk index (GNRI) is a simple nutritional assessment tool for elderly subjects. Its predictive value was evaluated in patients with HFpEF, a common HF phenotype in the elderly population. Methods and Results: The present study enrolled 152 consecutive patients (mean age, 77±11 years; male, 53.9%) who were hospitalized with HFpEF at the authors’ institution. GNRI on admission was calculated as follows: 14.89×serum albumin (g/dl)+41.7×body mass index/22. Characteristics and mortality (median follow-up of 2.1 years) were compared between 2 groups: low GNRI (<92) with moderate or severe nutritional risk; and high GNRI (≥92) with no or low nutritional risk. Patients in the low-GNRI group were more often female, and had lower serum hemoglobin and sodium, but higher serum blood urea nitrogen (BUN), C-reactive protein, and B-type natriuretic peptide (BNP) compared to those in the high-GNRI group (P<0.05, respectively). Physical activity at discharge measured by Barthel index was significantly lower in the low-GNRI group than the high-GNRI group (P<0.05). On Cox hazard analysis, lower GNRI predicted increased mortality independent of age, gender, prior HF hospitalization, and higher BUN and BNP (P<0.01). Conclusions: GNRI may be useful for predicting functional dependency and mortality in patients with HFpEF. (Circ J 2013; 77: 705–711)
- 著者
- Hiroyuki Tsutsui Hiroshi Ito Masafumi Kitakaze Issei Komuro Toyoaki Murohara Tohru Izumi Kenji Sunagawa Yoshio Yasumura Masafumi Yano Kazuhiro Yamamoto Tsutomu Yoshikawa Takayoshi Tsutamoto Junwei Zhang Akifumi Okayama Yoshihiko Ichikawa Kazuhiro Kanmuri Masunori Matsuzaki for the J-EMPHASIS-HF Study Group
- 出版者
- The Japanese Circulation Society
- 雑誌
- Circulation Journal (ISSN:13469843)
- 巻号頁・発行日
- vol.82, no.1, pp.148-158, 2017-12-25 (Released:2017-12-25)
- 参考文献数
- 19
- 被引用文献数
- 23
Background:The mineralocorticoid receptor antagonist eplerenone improved clinical outcomes among patients with heart failure with reduced ejection faction (HFrEF) in the EMPHASIS-HF (Eplerenone in Mild Patients Hospitalization And SurvIval Study in Heart Failure) study. However, similar efficacy and safety have not been established in Japanese patients. We evaluated the efficacy and safety of eplerenone in patients with HFrEF in a multicenter, randomized, double-blind placebo-controlled outcome study (ClinicalTrials.gov Identifier: NCT01115855). The aim of the study was to evaluate efficacy predefined as consistency of the primary endpoint with that of EMPHASIS-HF at a point estimate of <1 for the hazard ratio.Methods and Results:HFrEF patients with NYHA functional class II–IV and an EF ≤35% received eplerenone (n=111) or placebo (n=110) on top of standard therapy for at least 12 months. The primary endpoint was a composite of death from cardiovascular causes or hospitalization for HF. The primary endpoint occurred in 29.7% of patients in the eplerenone group vs. 32.7% in the placebo group [hazard ratio=0.85 (95% CI: 0.53–1.36)]. Hospitalization for any cause and changes in plasma BNP and LVEF were favorable with eplerenone. A total of 17 patients (15.3%) in the eplerenone group and 10 patients (9.1%) in the placebo group died. Adverse events, including hyperkalemia, were similar between the groups.Conclusions:Eplerenone was well-tolerated in Japanese patients with HFrEF and showed results consistent with those reported in the EMPHASIS-HF study.
- 著者
- Miyako Yoshida Honami Kojima Atsushi Uda Tamami Haraguchi Minoru Ozeki Ikuo Kawasaki Kazuhiro Yamamoto Ikuko Yano Midori Hirai Takahiro Uchida
- 出版者
- The Pharmaceutical Society of Japan
- 雑誌
- Chemical and Pharmaceutical Bulletin (ISSN:00092363)
- 巻号頁・発行日
- vol.67, no.5, pp.404-409, 2019-05-01 (Released:2019-05-01)
- 参考文献数
- 30
- 被引用文献数
- 9 9
The purpose of the study was to evaluate the ability of different beverages to mask the bitterness of zopiclone and eszopiclone in tablet formulations using the artificial taste sensor and human gustatory sensation testing. The beverages tested for bitterness-masking effects were: Mugicha, Sports beverage, Lactic acid drink, Orange juice and a diluted simple syrup (an 8.5% sucrose solution). The bitterness intensities estimated by the taste sensor of zopiclone or eszopiclone one-tablet solutions mixed with the various beverages, corresponded well with the observed bitterness intensities measured by gustatory sensation testing. The Sports beverage, Lactic acid drink and Orange juice significantly suppressed the bitterness intensity of both zopiclone and eszopiclone 1-tablet solutions compared with water when tested in the artificial taste sensor. Sports beverage, Lactic acid drink and Orange juice all contain citric acid as acidifier, so it was postulated that citric acid was involved in the mechanism of bitterness intensity suppression of zopiclone and eszopiclone 1-tablet solutions by these three beverages. It was then shown that citric acid suppressed the bitterness intensity of a zopiclone one-tablet sample solution in a dose-dependent manner. 1H-NMR spectroscopic analysis of mixtures of citric acid with zopiclone suggested that the carboxyl groups of citric acid interact with the amine group on zopiclone. This study therefore showed that the bitterness intensities of zopiclone and eszopiclone can be suppressed by citric-acid-contained beverages and suggests that this bitterness suppression is due to a direct electrostatic interaction between citric acid and the two drugs.
- 著者
- Yuya Matsue Yoshiharu Kinugasa Takeshi Kitai Shogo Ohishi Kazuhiro Yamamoto Hiroyuki Tsutsui
- 出版者
- The Japanese Circulation Society
- 雑誌
- Circulation Reports (ISSN:24340790)
- 巻号頁・発行日
- pp.CR-20-0081, (Released:2020-08-13)
- 参考文献数
- 18
- 被引用文献数
- 3
Background:The effect of the COVID-19 pandemic on the respiratory management strategy with regard to the use of non-invasive positive pressure ventilation (NPPV) and high-flow nasal cannula (HFNC) in patients with acute heart failure (AHF) in Japan is unclear.Methods and Results:This cross-sectional study used a self-reported online questionnaire, with responses from 174 institutions across Japan. More than 60% of institutions responded that the treatment of AHF patients requiring respiratory management became fairly or very difficult during the COVID-19 pandemic than earlier, with institutions in alert areas considering such treatment significantly more difficult than those in non-alert areas (P=0.004). Overall, 61.7% and 58.8% of institutions changed their indications for NPPV and HFNC, respectively. Significantly more institutions in the alert area changed their practices for the use of NPPV and HFNC during the COVID-19 pandemic (P=0.004 and P=0.002, respectively). When there was insufficient time or information to determine whether AHF patients may have concomitant COVID-19, institutions in alert areas were significantly more likely to refrain from using NPPV and HFNC than institutions in non-alert areas.Conclusions:The COVID-19 pandemic has compelled healthcare providers to change the respiratory management of AHF, especially in alert areas.
- 著者
- Taro Temma Toshiyuki Nagai Masaya Watanabe Rui Kamada Yumi Takahashi Hikaru Hagiwara Taro Koya Motoki Nakao Kazunori Omote Kiwamu Kamiya Hiroyuki Iwano Kazuhiro Yamamoto Tsutomu Yoshikawa Yoshihiko Saito Toshihisa Anzai
- 出版者
- The Japanese Circulation Society
- 雑誌
- Circulation Journal (ISSN:13469843)
- 巻号頁・発行日
- pp.CJ-19-0963, (Released:2020-02-01)
- 参考文献数
- 31
- 被引用文献数
- 9
Background:Atrial fibrillation (AF) is an important prognostic determinant in heart failure (HF) with preserved ejection fraction (HFpEF). However, it is unclear which HFpEF phenotypes are affected by AF in terms of long-term clinical outcomes because HFpEF is a heterogeneous syndrome with comorbidities such as coronary artery disease (CAD). In this study we determined the differential prognostic significance of AF in HFpEF patients according to CAD status.Methods and Results:Data for 408 hospitalized HFpEF patients enrolled in the Japanese Heart Failure Syndrome with Preserved Ejection Fraction Nationwide Multicenter Registry were analyzed. Patients were divided into 4 groups according to the presence of AF and CAD. The primary outcome was the composite of all-cause death and HF rehospitalization. The incidence of adverse events was higher in the AF–non-CAD than non-AF–non-CAD group (P=0.004). On multivariable Cox regression analysis with prespecified confounders, AF–non-CAD was significantly associated with an increased risk of adverse events than non-AF–non-CAD (adjusted HR, 1.91; 95% CI: 1.02–3.92) regardless of the type of AF. In contrast, risk was comparable between the AF–CAD and non-AF–CAD groups (adjusted HR, 1.24; 95% CI: 0.64–2.47).Conclusions:In HFpEF patients without CAD, AF was independently related to adverse events, indicating that intensive management of AF would have more beneficial effects particularly in HFpEF patients without CAD.
- 著者
- Maya Adachi Mai Watanabe Yasutaka Kurata Yumiko Inoue Tomomi Notsu Kenshiro Yamamoto Hiromu Horie Shogo Tanno Maki Morita Junichiro Miake Toshihiro Hamada Masanari Kuwabara Naoe Nakasone Haruaki Ninomiya Motokazu Tsuneto Yasuaki Shirayoshi Akio Yoshida Motonobu Nishimura Kazuhiro Yamamoto Ichiro Hisatome
- 出版者
- The Japanese Circulation Society
- 雑誌
- Circulation Journal (ISSN:13469843)
- 巻号頁・発行日
- pp.CJ-19-0261, (Released:2019-09-13)
- 参考文献数
- 39
- 被引用文献数
- 5
Background:Treatment of myocardial infarction (MI) includes inhibition of the sympathetic nervous system (SNS). Cell-based therapy using adipose-derived stem cells (ASCs) has emerged as a novel therapeutic approach to treat heart failure in MI. The purpose of this study was to determine whether a combination of ASC transplantation and SNS inhibition synergistically improves cardiac functions after MI.Methods and Results:ASCs were isolated from fat tissues of Lewis rats. In in vitro studies using cultured ASC cells, mRNA levels of angiogenic factors under normoxia or hypoxia, and the effects of norepinephrine and a β-blocker, carvedilol, on the mRNA levels were determined. Hypoxia increased vascular endothelial growth factor (VEGF) mRNA in ASCs. Norepinephrine further increased VEGF mRNA; this effect was unaffected by carvedilol. VEGF promoted VEGF receptor phosphorylation and tube formation of human umbilical vein endothelial cells, which were inhibited by carvedilol. In in vivo studies using a rat MI model, transplanted ASC sheets improved contractile functions of MI hearts; they also facilitated neovascularization and suppressed fibrosis after MI. These beneficial effects of ASC sheets were abolished by carvedilol. The effects of ASC sheets and carvedilol on MI heart functions were confirmed by Langendorff perfusion experiments using isolated hearts.Conclusions:ASC sheets prevented cardiac dysfunctions and remodeling after MI in a rat model via VEGF secretion. Inhibition of VEGF effects by carvedilol abolished their beneficial effects.