- 著者
- Taishi Okuno Masaki Izumo Noriko Shiokawa Shingo Kuwata Yuki Ishibashi Yukio Sato Masashi Koga Kazuaki Okuyama Norio Suzuki Keisuke Kida Yasuhiro Tanabe Yoshihiro J. Akashi
- 出版者
- The Japanese Circulation Society
- 雑誌
- Circulation Journal (ISSN:13469843)
- 巻号頁・発行日
- pp.CJ-23-0503, (Released:2023-11-25)
- 参考文献数
- 14
Background: The MitraClip G4 system is a new iteration of the transcatheter edge-to-edge repair system. We assessed the impact of the G4 system on routine practice and outcomes in secondary mitral regurgitation (2°MR).Methods and Results: Consecutive patients with 2°MR treated with either the MitraClip G2 (n=89) or G4 (n=63) system between 2018 and 2021 were included. Baseline characteristics, procedures, and outcomes were compared. Inverse probability of treatment weighting and Cox regression were used to adjust for baseline differences. Baseline characteristics were similar, except for a lower surgical risk in the G4 group (Society of Thoracic Surgeons Predicted Risk of Mortality ≥8: 38.1% vs. 56.2%; P=0.03). In the G4 group, more patients had short (≤2 mm) coaptation length (83.7% vs. 54.0%; P<0.001) and fewer clips were used (17.5% vs. 36.0%; P=0.02). Acceptable MR reduction was observed in nearly all patients, with no difference between the G4 and G2 groups (100% vs. 97.8%, respectively; P=0.51). The G4 group had fewer patients with high transmitral gradients (>5mmHg; 3.3% vs. 13.6%; P=0.03). At 1 year, there was no significant difference between groups in the composite endpoint (death or heart failure rehospitalization) after baseline adjustment (10.5% vs. 20.2%; hazard ratio 0.39; 95% confidence interval 0.11–1.32; P=0.13).Conclusions: The G4 system achieved comparable device outcomes to the early-generation G2, despite treating more challenging 2°MR with fewer clips.
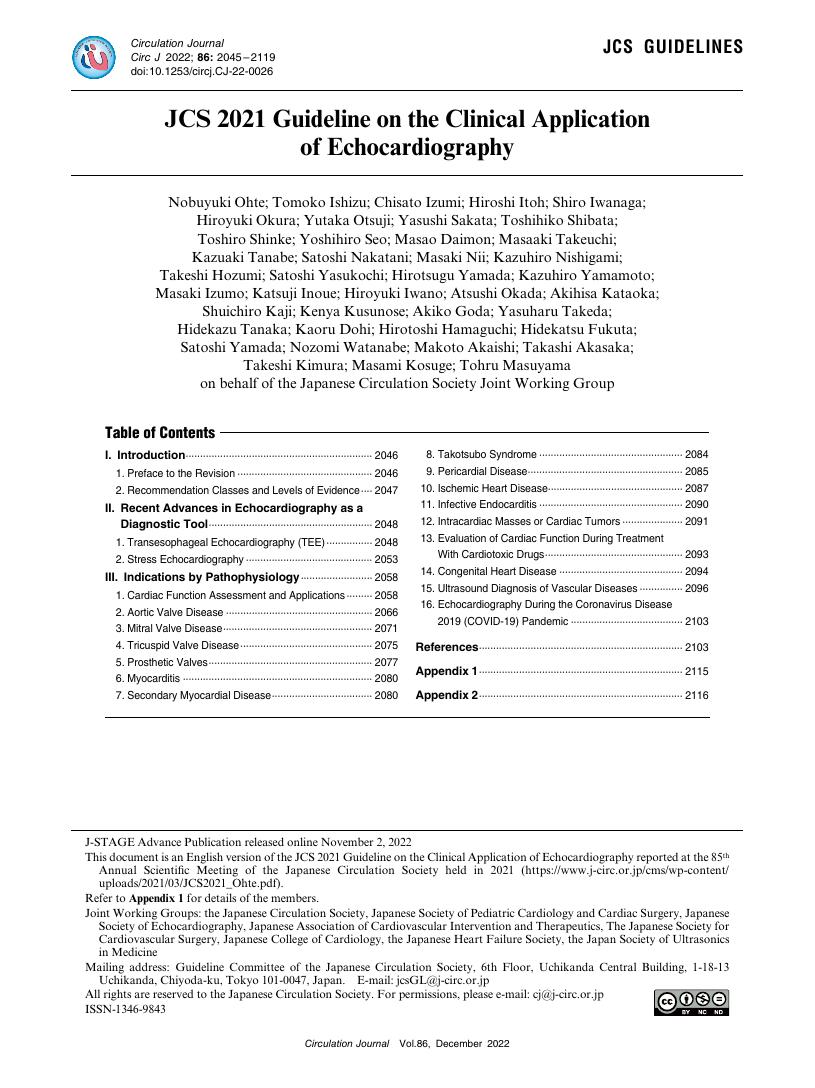
- 著者
- Nobuyuki Ohte Tomoko Ishizu Chisato Izumi Hiroshi Itoh Shiro Iwanaga Hiroyuki Okura Yutaka Otsuji Yasushi Sakata Toshihiko Shibata Toshiro Shinke Yoshihiro Seo Masao Daimon Masaaki Takeuchi Kazuaki Tanabe Satoshi Nakatani Masaki Nii Kazuhiro Nishigami Takeshi Hozumi Satoshi Yasukochi Hirotsugu Yamada Kazuhiro Yamamoto Masaki Izumo Katsuji Inoue Hiroyuki Iwano Atsushi Okada Akihisa Kataoka Shuichiro Kaji Kenya Kusunose Akiko Goda Yasuharu Takeda Hidekazu Tanaka Kaoru Dohi Hirotoshi Hamaguchi Hidekatsu Fukuta Satoshi Yamada Nozomi Watanabe Makoto Akaishi Takashi Akasaka Takeshi Kimura Masami Kosuge Tohru Masuyama on behalf of the Japanese Circulation Society Joint Working Group
- 出版者
- The Japanese Circulation Society
- 雑誌
- Circulation Journal (ISSN:13469843)
- 巻号頁・発行日
- vol.86, no.12, pp.2045-2119, 2022-11-25 (Released:2022-11-25)
- 参考文献数
- 460
- 被引用文献数
- 16
- 著者
- Takashi Matsumoto Shunsuke Kubo Masaki Izumo Shingo Mizuno Shinichi Shirai on behalf of the MitraClip Japan PMS Investigators
- 出版者
- The Japanese Circulation Society
- 雑誌
- Circulation Journal (ISSN:13469843)
- 巻号頁・発行日
- pp.CJ-21-0309, (Released:2021-10-29)
- 参考文献数
- 16
- 被引用文献数
- 10
Background:The MitraClip NT System was approved for marketing in Japan on October 31, 2017, and a prospective, multi-center, single-arm Post-Marketing use Surveillance (PMS) study was launched in 2018. This is the first report of the Japan PMS study with 1-year subject outcomes.Methods and Results:A total of 500 patients were registered between April 2018 and January 2019. Patients with symptomatic chronic moderate-to-severe (3+) or severe mitral regurgitation (MR; 4+), MR with a Society of Thoracic Surgery (STS) replacement score of ≥8%, or presence of 1 pre-defined risk factor were enrolled. Primary outcome measures included acute procedural success (APS), and rate of Single Leaflet Device Attachment (SLDA) at 30 days. The overall cohort was elderly (77.9±9.48 years) with functional MR etiology in 71.6% of the subjects. The majority of subjects were New York Heart Association (NYHA) class III/IV (68.9%), with mean STS replacement score of 11.95±9.66%. The APS rate was 91.13% and the 30-day SLDA rate was 1.21%. Durable MR reduction was achieved with 88.1% of subjects at MR ≤2+ at 1 year. Significant improvement in the functional capacity was observed, with 93% of subjects at NYHA class I/II at 1 year.Conclusions:In the Japan PMS experience, the MitraClip procedure resulted in improvements in MR severity, with significantly improved functional outcomes. These results demonstrate safety and efficacy of MitraClip therapy in the eligible Japanese population.
- 著者
- Shingo Kuwata Masaki Izumo Taishi Okuno Noriko Shiokawa Yukio Sato Masashi Koga Kazuaki Okuyama Yasuhiro Tanabe Tomoo Harada Yuki Ishibashi Yoshihiro J Akashi
- 出版者
- The Japanese Circulation Society
- 雑誌
- Circulation Journal (ISSN:13469843)
- 巻号頁・発行日
- pp.CJ-23-0240, (Released:2023-07-13)
- 参考文献数
- 22
- 被引用文献数
- 2
Background: Renal congestion is a potential prognostic factor in patients with heart failure and recently, assessment has become possible with intrarenal Doppler ultrasonography (IRD). The association between renal congestion assessed by IRD and outcomes after mitral transcatheter edge-to-edge repair (TEER) is unknown, so we aimed to clarify renal congestion and its prognostic implications in patients with mitral regurgitation (MR) who underwent TEER using MitraClip system.Methods and Results: Patients with secondary MR who underwent TEER and were assessed for intrarenal venous flow (IRVF) by IRD were classified according to their IRVF pattern as continuous or discontinuous. Of the 105 patients included, 78 patients (74%) formed the continuous group and 27 (26%) were the discontinuous group. Kaplan-Meier analysis revealed significant prognostic power of the IRVF pattern for predicting the composite outcome of all-cause death and heart failure rehospitalization (log-rank P=0.0257). On multivariate Cox regression analysis, the composite endpoint was independently associated with the discontinuous IRVF pattern (hazard ratio, 3.240; 95% confidence interval, 1.300–8.076; P=0.012) adjusted using inverse probability of treatment weighting.Conclusions: IRVF patterns strongly correlated with clinical outcomes without changes in renal function. Thus, they may be useful for risk stratification after mitral TEER for patients with secondary MR.
- 著者
- Makoto Miyake Misa Takegami Yuki Obayashi Masashi Amano Takeshi Kitai Tomoyuki Fujita Tadaaki Koyama Hidekazu Tanaka Kenji Ando Tatsuhiko Komiya Masaki Izumo Hiroya Kawai Kiyoyuki Eishi Kiyoshi Yoshida Takeshi Kimura Ryuzo Nawada Tomohiro Sakamoto Yoshisato Shibata Toshihiro Fukui Kenji Minatoya Kenichi Tsujita Yasushi Sakata Tetsuya Kimura Kumiko Sugio Atsushi Takita Atsushi Iwakura Toshihiro Tamura Kunihiro Nishimura Yutaka Furukawa Chisato Izumi for the BPV-AF Registry Group
- 出版者
- The Japanese Circulation Society
- 雑誌
- Circulation Journal (ISSN:13469843)
- 巻号頁・発行日
- pp.CJ-22-0226, (Released:2022-07-08)
- 参考文献数
- 28
- 被引用文献数
- 2
Background: Current guidelines equally recommend direct oral anticoagulants (DOACs) and warfarin for atrial fibrillation (AF) patients with a bioprosthetic valve (BPV); however, there are limited data comparing DOACs and warfarin in AF patients with an aortic BPV.Methods and Results: This post-hoc subgroup analysis of a multicenter, prospective, observational registry (BPV-AF Registry) aimed to compare DOACs and warfarin in AF patients with an aortic BPV. The primary outcome was a composite of stroke, systemic embolism, major bleeding, heart failure requiring hospitalization, all-cause death, or BPV reoperation. The analysis included 479 patients (warfarin group, n=258; DOAC group, n=221). Surgical aortic valve replacement was performed in 74.4% and 36.7% of patients in the warfarin and DOAC groups, respectively. During a mean follow up of 15.5 months, the primary outcome occurred in 45 (17.4%) and 32 (14.5%) patients in the warfarin and DOAC groups, respectively. No significant difference was found in the primary outcome between the 2 groups (adjusted hazard ratio: 0.88, 95% confidence interval: 0.51–1.50). No significant multiplicative interaction was observed between the anticoagulant effects and type of aortic valve procedure (P=0.577).Conclusions: Among AF patients with an aortic BPV, no significant difference was observed in the composite outcome of adverse clinical events between patients treated with warfarin and those treated with DOACs, suggesting that DOACs can be used as alternatives to warfarin in these patients.