21 0 0 0 OA 腎機能低下患者における薬物暴露量変化と腎排泄寄与率の関係の網羅的解析
- 著者
- 山田 麻衣子 大野 能之 樋坂 章博 山口 諒 鈴木 洋史
- 出版者
- 一般社団法人日本医療薬学会
- 雑誌
- 医療薬学 (ISSN:1346342X)
- 巻号頁・発行日
- vol.39, no.11, pp.660-667, 2013-11-10 (Released:2014-11-10)
- 参考文献数
- 22
- 被引用文献数
- 1 1
We investigated the relationships between the renal excretion ratio (RR) and changes in drug exposure in patients with renal dysfunction (RD), to examine the usefulness of RR in determining the optimal dosage for patients with renal dysfunction.The area under the plasma concentration time curve ratios (AUC ratios: AUCRs = AUCRD/AUCNormal) of 52 out of 70 drugs was observed within 67-150% of the theoretical values calculated by the Giusti-Hayton method using the RR value. It was confirmed that the RR is useful for determining the optimal dosage of extensively renally excreted drugs for patients with RD. However, it should be noted that the AUCRs were more than 150 % of the theoretical value for some orally administrated drugs that are excreted renally but less extensively. Especially, for substrates of OATP1B1 or OATP1B3, the AUCRs of four out of five drugs were more than 150%. Substrates of metabolizing enzymes and other transporters showed less relevance in this regard.
12 0 0 0 OA 医療用医薬品(内用薬剤)の添付文書における腎機能低下患者への投与に関連する記載内容の調査研究
- 著者
- 竹内 裕紀 大野 能之 和泉 智 鎌田 直博 田中 章郎 長谷川 功 三宅 健文 奥田 真弘
- 出版者
- 一般社団法人日本医療薬学会
- 雑誌
- 医療薬学 (ISSN:1346342X)
- 巻号頁・発行日
- vol.42, no.3, pp.160-167, 2016-03-10 (Released:2017-03-16)
- 参考文献数
- 14
- 被引用文献数
- 1 1
The dosage and administration of renally excreted drugs to patients with decreased renal function need to be optimized in accordance with their renal function. However, drug package inserts do not necessarily have sufficient information. Therefore, we identified and classified the issues regarding this lack of information and investigated the percentage of affected package inserts.We investigated 341 oral drugs in the Clinical Practice Guidebook of Chronic Kidney Disease 2012.1. The shortcomings in the description of urinary excretion parameters, which is needed for dose adjustment in accordance with renal function, are classified as follows: (1) unchanged drugs and metabolites are not indicated (28%, 95/341), (2) bioavailability for oral dosage is not taken into account (84%, 286/341), and (3) sufficient recovery time for urinary excretion is not acknowledged (3.5%, 12/341).2. With respect to the dosage regimen of renally excreted drugs, the following information was absent: (1) dosage and dosing interval in accordance with renal function are not described (63%, 70/111) and (2) considerations for dose reduction are not provided (32%, 36/111).3. A major shortcoming in the description of drug administration for anuric dialysis patient is that nephrotoxic drugs, such as, nonsteroidal anti-inflammatory drugs, are described as being contraindicated (100%, 11/11).We found that the current information in package inserts of several drugs is insufficient to understand the required dose adjustment or the correct method of administration to patients with decreased renal function. We aim to improve the information in drug package inserts to allow for effective and safe pharmacotherapy.
- 著者
- 大野 能之
- 出版者
- 公益社団法人 日本薬学会
- 雑誌
- YAKUGAKU ZASSHI (ISSN:00316903)
- 巻号頁・発行日
- vol.138, no.3, pp.337-345, 2018-03-01 (Released:2018-03-01)
- 参考文献数
- 38
- 被引用文献数
- 1 2
Drug-drug interactions (DDIs) can affect the clearance of various drugs from the body; however, these effects are difficult to sufficiently evaluate in clinical studies. This article outlines our approach to improving methods for evaluating and providing drug information relative to the effects of DDIs. In a previous study, total exposure changes to many substrate drugs of CYP caused by the co-administration of inhibitor or inducer drugs were successfully predicted using in vivo data. There are two parameters for the prediction: the contribution ratio of the enzyme to oral clearance for substrates (CR), and either the inhibition ratio for inhibitors (IR) or the increase in clearance of substrates produced by induction (IC). To apply these predictions in daily pharmacotherapy, the clinical significance of any pharmacokinetic changes must be carefully evaluated. We constructed a pharmacokinetic interaction significance classification system (PISCS) in which the clinical significance of DDIs was considered in a systematic manner, according to pharmacokinetic changes. The PISCS suggests that many current ‘alert’ classifications are potentially inappropriate, especially for drug combinations in which pharmacokinetics have not yet been evaluated. It is expected that PISCS would contribute to constructing a reliable system to alert pharmacists, physicians and consumers of a broad range of pharmacokinetic DDIs in order to more safely manage daily clinical practices.
6 0 0 0 医療現場における薬物相互作用へのかかわり方(1)
- 著者
- 大野 能之 樋坂 章博 岩本 卓也 木村 丈司 百 賢二 米澤 淳 伊藤 清美
- 出版者
- 一般社団法人日本医療薬学会
- 雑誌
- 医療薬学 (ISSN:1346342X)
- 巻号頁・発行日
- vol.44, no.11, pp.537-545, 2018-11-10 (Released:2019-11-10)
- 参考文献数
- 11
The first academic subcommittee of the Japanese Society of Pharmaceutical Health Care and Sciences has a plan to create a guide on how to manage drug interactions in clinical settings. This review describes the information that forms the basis of the guide. This article, part (1), reports the results of a questionnaire on the content of the guide and also describes how to evaluate and manage drug interactions in clinical settings. The contents of the ʻDrug Interaction Guideline for Drug Development and Labeling Recommendationsʼ, the new Japanese guideline, are also described. It is important also in clinical practice to appropriately evaluate and manage drug interactions based on a sufficient understanding of the new guideline and related information.
4 0 0 0 OA クリアランス理論に基づいた医薬品情報の評価と提供に関する研究
- 著者
- 大野 能之
- 出版者
- 一般社団法人日本医療薬学会
- 雑誌
- 医療薬学 (ISSN:1346342X)
- 巻号頁・発行日
- vol.39, no.5, pp.257-270, 2013-05-10 (Released:2014-05-10)
- 参考文献数
- 33
- 被引用文献数
- 1
Renal dysfunction and drug-drug interactions (DDIs) can affect the clearance of various drugs from the body; however, these effects are difficult to sufficiently evaluate in clinical studies. This article outlines our recent approaches to improve the method of evaluating and providing the drug information on the effects of renal dysfunction and DDIs. These approaches aim to optimize the drug regimens of patients with renal dysfunction and to improve the management of DDIs. The renal excretion ratio (RR) is required to predict alterations in drug clearance in patients with renal dysfunction. However, the estimation of RR requires pharmacokinetic information that is not always provided in the Japanese drug package inserts or interview forms.A systematic approach to predict changes in drug clearance due to DDIs of the cytochrome p450 (CYP) is described. Uniquely, this method uses a small number of parameters, which are only obtained by in vivo DDI studies, i.e., the contribution ratio of CYPs to oral clearance of substrates (CR), the inhibition ratio of inhibitors (IR) or the increase in clearance by induction (IC). Changes in oral clearance for any combination of drugs can be predicted once these parameters have been calculated for each drug. These predictions were used to construct a pharmacokinetic interaction significance classification system (PISCS) to evaluate the clinical risk of DDIs in daily therapy.
4 0 0 0 OA 医療現場における薬物相互作用へのかかわり方(2)
- 著者
- 木村 丈司 岩本 卓也 大野 能之 樋坂 章博 百 賢二 米澤 淳 伊藤 清美
- 出版者
- 一般社団法人日本医療薬学会
- 雑誌
- 医療薬学 (ISSN:1346342X)
- 巻号頁・発行日
- vol.44, no.11, pp.546-558, 2018-11-10 (Released:2019-11-10)
- 参考文献数
- 44
The first academic subcommittee of the Japanese Society of Pharmaceutical Health Care and Sciences has a plan to create a guide on how to manage drug interactions in clinical settings. This review describes the information that forms the basis of the guide. This article, part (2), summarizes the practice reports on managing drug interactions in clinical settings, their problems, and the proper concepts of drug interactions in patients with special background. Each pharmacist is expected to enhance the literacy of drug interactions and manage them adequately, which will lead to the improvement of clinical outcomes.
3 0 0 0 OA 腎臓病患者への薬物投与設計の理論と実際
- 著者
- 大野 能之 樋坂 章博 山田 麻衣子 山本 武人 鈴木 洋史
- 出版者
- 一般社団法人 日本腎臓病薬物療法学会
- 雑誌
- 日本腎臓病薬物療法学会誌 (ISSN:21870411)
- 巻号頁・発行日
- vol.1, no.3, pp.119-130, 2012 (Released:2018-04-02)
- 参考文献数
- 29
腎機能障害時には、各薬剤の腎排泄寄与率を正しく把握しておく必要がある。腎排泄寄与率とは、全身クリアランスに対する腎のクリアランスの割合を指す。この時重要なのが、基本的には未変化体の尿中排泄率である。不活性の代謝物を含めた腎排泄率が高くても、活性本体の未変化体の排泄が少なければ、腎機能の低下は薬効にさほど影響しない。ただし、内服薬の場合は、投与された薬剤が全身循環する割合、すなわちバイオアベイラビリティを考慮し、補正しなければならない。その他、腎から排泄される代謝物に薬効や毒性がある場合は、腎機能に応じて投与量を調整する必要がある。また、特に血中濃度半減期が極端に長い薬剤の場合は、体内から排泄が終了するまで、十分時間をとって観察されたデータを用いるべきである。 腎機能障害がある場合に、そうでない場合と同程度の血中濃度を維持する方法としては、一回あたりの投与量の減量と、一回あたりの投与量の減量はせず投与間隔を延長をする方法の2つが考えられる。投与量の調整は比較的簡便である一方、薬剤によっては血中濃度が定常状態に達するまでに時間を要することが懸念される。このような場合、速やかな効果発現を求めるのであれば、治療初期は通常用量で使用し、血中濃度が治療濃度域に達した後に減量するなどの対応が必要になる。 投与間隔を調整する場合には、1 回の用量は変わらないため、血中濃度のピーク値は通常使用時と同程度まで上がり、投与間隔をあける分、トラフ値も同程度となる。しかし、高濃度または低濃度の時間が継続するため、効果や副作用の面から望ましくない場合もある。こうした長所、短所を理解したうえで、個々の薬剤及び患者ごとに適切な投与設計を行うことが重要である。
3 0 0 0 OA 医療現場における薬物相互作用へのかかわり方(3)
- 著者
- 百 賢二 米澤 淳 岩本 卓也 大野 能之 木村 丈司 樋坂 章博 伊藤 清美
- 出版者
- 一般社団法人日本医療薬学会
- 雑誌
- 医療薬学 (ISSN:1346342X)
- 巻号頁・発行日
- vol.44, no.11, pp.559-567, 2018-11-10 (Released:2019-11-10)
- 参考文献数
- 31
The first academic subcommittee of the Japanese Society of Pharmaceutical Health Care and Sciences has a plan to create a guide on how to manage drug interactions in clinical settings. This review describes the information that forms the basis of the guide. As evidence for drug interactions with various mechanisms has not been clarified for all combinations, each case needs to be managed based on knowledge of clinical pharmacology regarding drug interactions. This article, part (3), shows the examples of both experimental and surveillance studies on drug interactions and also summarizes the points that require consideration when conducting surveillance studies.The focus on drug interactions based on polypharmacy is increasing given that the number of elderly people continues to increase in Japan. Pharmacists are expected to contribute to the proper use of drugs through the assessment and performance of wet and dry studies.
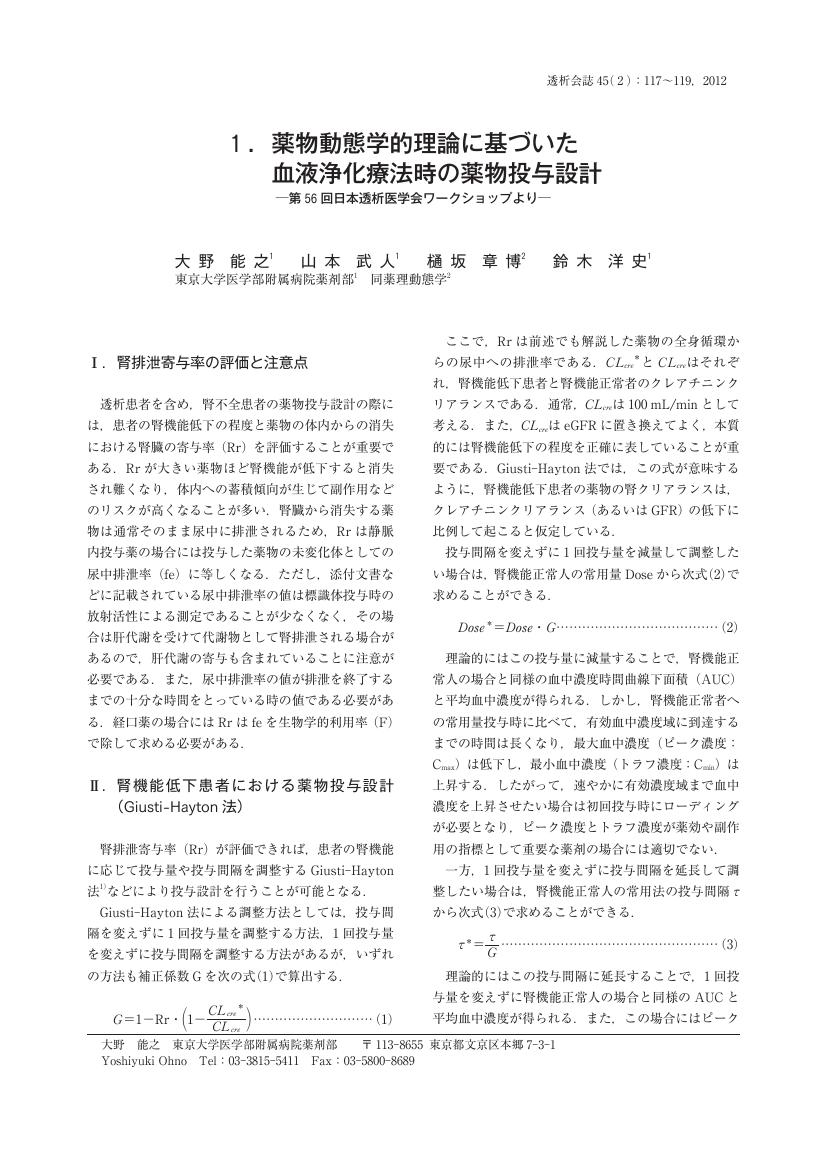
1 0 0 0 OA 1. 薬物動態学的理論に基づいた血液浄化療法時の薬物投与設計
- 著者
- 大野 能之 山本 武人 樋坂 章博 鈴木 洋史
- 出版者
- 一般社団法人 日本透析医学会
- 雑誌
- 日本透析医学会雑誌 (ISSN:13403451)
- 巻号頁・発行日
- vol.45, no.2, pp.117-119, 2012-02-28 (Released:2012-02-29)
- 参考文献数
- 4
1 0 0 0 OA 病棟薬剤師の配置展開が処方提案および相談応需に与える効果
- 著者
- 小久江 伸介 大野 能之 折山 豊仁 山口 諒 徳田 篤志 長瀬 幸恵 鈴木 洋史
- 出版者
- 一般社団法人日本医療薬学会
- 雑誌
- 医療薬学 (ISSN:1346342X)
- 巻号頁・発行日
- vol.42, no.10, pp.694-700, 2016-10-10 (Released:2017-10-10)
- 参考文献数
- 7
- 被引用文献数
- 1 4
At the University of Tokyo hospital, we began allocation of ward pharmacists to some wards in August 2012 and to all wards in August 2014. In this study, we qualitatively and quantitatively reviewed cases reported by ward pharmacists to evaluate the effects of this allocation on intervention and consultation that required positive participation.We retrospectively reviewed the pharmaceutical interventions' record from April 2012 through March 2015. We also analyzed cases for three months after the allocation of pharmacists to every ward. We found a highly positive correlation (R2 = 0.928, P < 0.0001) between the number of wards and pharmaceutical interventions. Intervention cases per month increased by 21.5 after allocating a pharmacist to a ward. There were a total of 2,438 intervention cases over three months. Active and passive approaches were employed in 1,833 cases and 605 cases, respectively. High-risk medicines were associated with 39.3% of cases. The prescription change rate was 86.2% for active interventions and 50.9% for passive interventions.Results showed that the allocation of a ward pharmacist could assist pharmaceutical approaches through the evaluation of patient complaints and clinical conditions, participation in the treatment plan, and consultation from medical staff. There were also reports that an active approach led to critical adverse event avoidance and pharmacotherapy effect improvement. These findings suggest that the allocation of ward pharmacists results in the promotion of healthcare services and medical safety.