- 著者
- Atsushi Mizuno Hidehiro Kaneko Yuta Suzuki Akira Okada Norifumi Takeda Hiroyuki Morita Katsuhito Fujiu Koichi Node Hideo Yasunaga Issei Komuro
- 出版者
- The Japanese Circulation Society
- 雑誌
- Circulation Journal (ISSN:13469843)
- 巻号頁・発行日
- pp.CJ-23-0292, (Released:2023-06-30)
- 参考文献数
- 13
- 被引用文献数
- 1
Background: The applicability of the Stages of Change model for cardiovascular disease-related behaviors, such as smoking, exercise, diet, and sleep quality, is unclear.Methods and Results: Using a large-scale epidemiological dataset, we found that baseline behavior change intention, as per the transtheoretical model, was associated with modifications of unhealthy lifestyles including cigarette smoking, physical inactivity, skipping breakfast, and poor sleep quality.Conclusions: Our results suggest that an individual’s motivation to change assessed by a general questionnaire may contribute to lifestyle modification and potentially prevent subsequent cardiovascular disease.
- 著者
- Atsushi Mizuno Chisa Matsumoto Takuya Kishi Mari Ishida Shoji Sanada Memori Fukuda Issei Komuro Kenichi Hirata Koichi Node
- 出版者
- The Japanese Circulation Society
- 雑誌
- Circulation Reports (ISSN:24340790)
- 巻号頁・発行日
- vol.3, no.2, pp.100-104, 2021-02-10 (Released:2021-02-10)
- 参考文献数
- 14
- 被引用文献数
- 5
Background:Cardiovascular department restriction policies on procedures resulting from the COVID-19 pandemic have not been fully evaluated.Methods and Results:We performed a retrospective analysis of a nationwide survey performed by the Japanese Circulation Society in August 2020. The total response rate was 48.9% (651/1,331). The rate of restriction of cardiovascular procedures peaked in April. Exacerbations of heart failure due to hospital restrictions were noted in 43.8% of departments.Conclusions:Many departments restricted their cardiological procedures, and this rate changed according to the pandemic situation. The exacerbation of cardiovascular disease resulting from pandemic restrictions should not be ignored.
- 著者
- Atsushi Mizuno Koichiro Niwa Kozo Matsuo Masaaki Kawada Aya Miyazaki Yoshiki Mori Norifumi Nakanishi Hideo Ohuchi Mamie Watanabe Atsushi Yao Kei Inai
- 出版者
- The Japanese Circulation Society
- 雑誌
- Circulation Journal (ISSN:13469843)
- 巻号頁・発行日
- vol.77, no.12, pp.2942-2947, 2013 (Released:2013-11-25)
- 参考文献数
- 33
- 被引用文献数
- 16 21
Background: Although the survival rate for repaired Tetralogy of Fallot (TOF) is dramatically improving, anatomical and functional residua and sequelae followed by arrhythmias and sudden death are still challenging issues to be resolved. Reoperation can reduce the incidence of arrhythmias and sudden death, but there is no consensus on the indications of reoperation for patients with TOF, especially in Japan. Methods and Results: A cross-sectional questionnaire survey of reoperation indications in patients with TOF was performed through a Japanese multicenter study. The questionnaire, which focused on the number of repaired TOF patients aged >15 years old, reoperation indications and management, was sent to the institutions belonging to Japanese Society for Adult Congenital Heart Disease. In total, 41.5% (78/188) of the institutions replied. The total number of repaired TOF patients was 4,010, and sudden cardiac death was observed in 45.236/4,010 (5.9%) experienced reoperation. Pulmonary stenosis (32%) and pulmonary regurgitation (29%) were the most common reasons for reoperation. There were only 2 implantable cardioverter defibrillator or resynchronization therapy defibrillator implantations. The physiological/anatomical indications of reoperation differed among the hospitals. Conclusions: Approximately 1.1% of patients suffered sudden death and 6% of repaired TOF patients had reoperation. The indications of reoperation, however, varied among the institutions. Therefore, detailed information for each case of sudden death or reoperation should be collected and analyzed in order to establish guidelines for reoperation. (Circ J 2013; 77: 2942–2947)
- 著者
- Jin Komuro Yuji Nagatomo Keitaro Mahara Mitsuaki Isobe Ayumi Goda Yasumori Sujino Atsushi Mizuno Yasuyuki Shiraishi Takashi Kohno Shun Kohsaka Tsutomu Yoshikawa West Tokyo Heart Failure (WET-HF) Registry Investigators
- 出版者
- The Japanese Circulation Society
- 雑誌
- Circulation Reports (ISSN:24340790)
- 巻号頁・発行日
- vol.1, no.4, pp.162-170, 2019-04-10 (Released:2019-04-10)
- 参考文献数
- 31
- 被引用文献数
- 8
Background: The concept of Clinical Scenario (CS) classification has been widely utilized to aid in choosing appropriate management strategies for acute decompensated heart failure (ADHF). Methods and Results: The West Tokyo-Heart Failure (WET-HF) Registry is a multicenter, prospective cohort registry enrolling consecutive hospitalized ADHF patients. Based on systolic blood pressure (SBP) at admission, 4,000 patients enrolled between 2006 and 2017 were classified into 3 groups: CS1, SBP ≥140 mmHg; CS2, 100≤SBP<140 mmHg; and CS3, SBP <100 mmHg. The CS1 group had a high rate of fluid retention such as leg edema, and the largest reduction in body weight at discharge. In-hospital diuretics use was the most frequent in CS1. Although the primary endpoint of long-term all-cause death and/or ADHF re-hospitalization was more common in more advanced CS, there was no significant difference between the 3 CS groups in patients with HF with preserved ejection fraction (HFpEF; P=0.10). Although more advanced CS was associated with larger left ventricular (LV) chamber size in HF with reduced EF (HFrEF), it was associated with smaller LV size in HFpEF. Conclusions: The long-term prognostic value of CS classification was limited in HFpEF. Whereas CS was closely associated with degree of LV remodeling in HFrEF, a smaller LV chamber might be associated with a lower cardiovascular functional reserve in HFpEF.
- 著者
- Keitaro Shinada Takashi Kohno Keiichi Fukuda Michiaki Higashitani Naoto Kawamatsu Takeshi Kitai Tatsuhiro Shibata Makoto Takei Kotaro Nochioka Gaku Nakazawa Hiroki Shiomi Mitsunori Miyashita Atsushi Mizuno
- 出版者
- The Japanese Circulation Society
- 雑誌
- Circulation Journal (ISSN:13469843)
- 巻号頁・発行日
- pp.CJ-23-0507, (Released:2023-11-22)
- 参考文献数
- 29
- 被引用文献数
- 1
Background: Enhanced discussions regarding end-of-life (EOL) are crucial to provide appropriate care for seriously ill patients. However, the current status of EOL discussions, especially their timing and influencing factors, among patients with cardiovascular diseases (CVD) remains unknown.Methods and Results: We conducted a cross-sectional questionnaire survey of bereaved family members of CVD patients who died at 10 tertiary care institutes in Japan. In all, 286 bereaved family members (38.2% male; median age 66.0 [interquartile range 58.0–73.0] years) of CVD patients were enrolled; of these, 200 (69.9%) reported that their families had had EOL discussions with physicians. The major topic discussed was resuscitation (79.0%), and 21.5% discussed the place of EOL care. Most discussions were held during hospitalization of the patient (88.2%). More than half (57.1%) the discussions were initiated less than 1 month before the patient died, and 22.6% of family members felt that this timing of EOL discussions was late. Bereaved family members’ perception of late EOL discussions was associated with the family members aggressive attitude towards life-prolonging treatment, less preparedness for bereavement, and less satisfaction with EOL care.Conclusions: Approximately 70% of bereaved family members of CVD patients had EOL discussions, which were often held shortly before the patient died. Further research is required to establish an ideal approach to EOL discussions at an appropriate time, which may improve the quality of EOL care.
- 著者
- Tadafumi Sugimoto Atsushi Mizuno Daisuke Yoneoka Shingo Matsumoto Chisa Matsumoto Yuya Matsue Mari Ishida Michikazu Nakai Yoshitaka Iwanaga Yoshihiro Miyamoto Koichi Node
- 出版者
- The Japanese Circulation Society
- 雑誌
- Circulation Reports (ISSN:24340790)
- 巻号頁・発行日
- vol.4, no.8, pp.353-362, 2022-08-10 (Released:2022-08-10)
- 参考文献数
- 15
- 被引用文献数
- 3
Background: Although reductions in hospitalizations for myocardial infarction and heart failure have been reported during the period of COVID-19 pandemic restrictions, it is unclear how the overall number of hospitalizations for cardiovascular disease (CVD) treatment changed in the early stages of the pandemic.Methods and Results: We analyzed the records of 574 certified hospitals affiliated with the Japanese Circulation Society and retrieved data from April 2015 to March 2020. Records were obtained from the nationwide Japanese Registry of All Cardiac and Vascular Diseases–Diagnosis Procedure Combination database. A quasi-Poisson regression model was used to estimate the number of hospitalizations for CVD treatment. Between January and March 2020, when the number of COVID-19 cases was relatively low in Japan, the actual/estimated number of hospitalizations for acute CVD was 18,233/21,634 (84.3%), whereas the actual/estimated number of scheduled hospitalizations was 16,921/19,066 (88.7%). The number of hospitalizations for acute heart failure and scheduled hospitalizations for valvular disease and aortic aneurysm were 81.1%, 84.6%, and 83.8% of the estimated values, respectively. A subanalysis that considered only facilities without hospitalization restrictions did not alter the results for these diseases.Conclusions: The spread of COVID-19 was associated with a decreased number of hospitalizations for CVD in Japan, even in the early stages of the pandemic.
- 著者
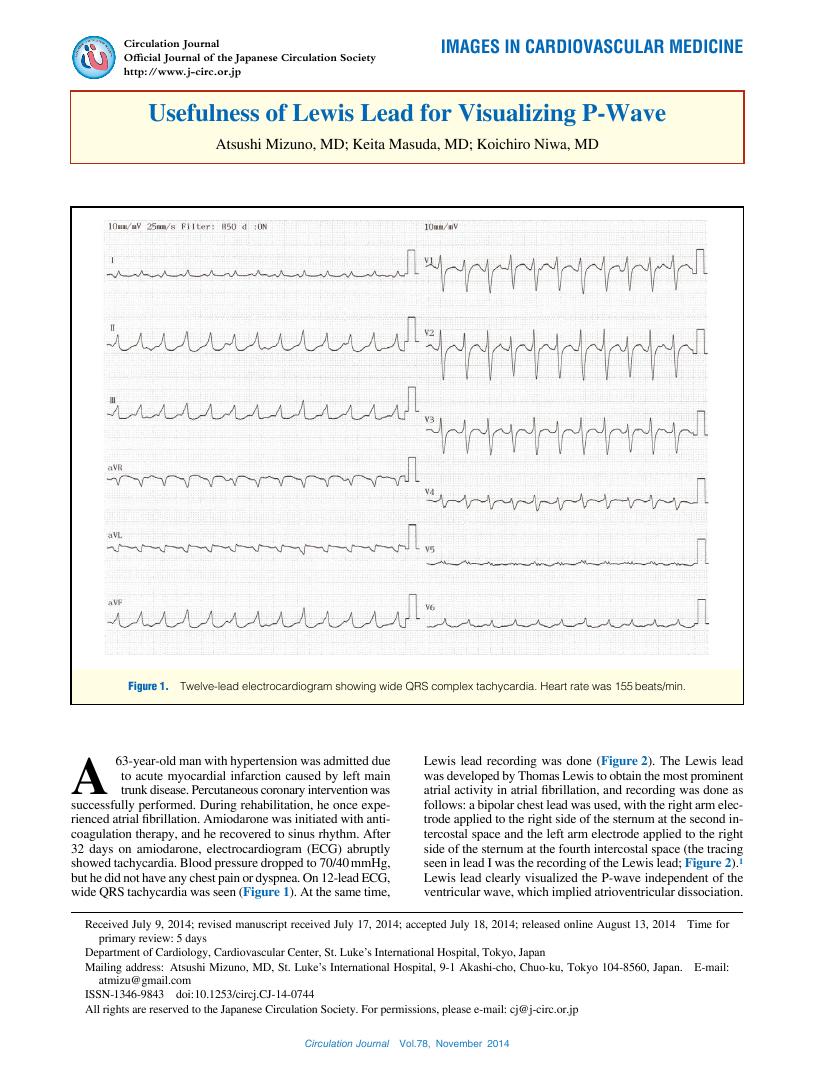
- Atsushi Mizuno Keita Masuda Koichiro Niwa
- 出版者
- The Japanese Circulation Society
- 雑誌
- Circulation Journal (ISSN:13469843)
- 巻号頁・発行日
- vol.78, no.11, pp.2774-2775, 2014-10-24 (Released:2014-10-24)
- 参考文献数
- 10
- 被引用文献数
- 4 5
- 著者
- Keiko Fukino Daisuke Ueshima Tetsuo Yamaguchi Atsushi Mizuno Kazuki Tobita Kenji Suzuki Naotaka Murata Kentaro Jujo Takahide Kodama Fumitaka Nakamura Michiaki Higashitani
- 出版者
- The Japanese Circulation Society
- 雑誌
- Circulation Journal (ISSN:13469843)
- 巻号頁・発行日
- pp.CJ-23-0215, (Released:2023-10-06)
- 参考文献数
- 48
Background: The mechanism underlying a poor prognosis in patients with lower-extremity artery disease (LEAD) with heart failure is unknown. We examined the prognostic impact of the left ventricular ejection fraction (LVEF) in patients with LEAD who underwent endovascular therapy (EVT).Methods and Results: From August 2014 to August 2016, 2,180 patients with LEAD (mean age, 73.2 years; male, 71.9%) underwent EVT and were stratified into low-LVEF (LVEF <40%; n=234, 10.7%) and not-low LVEF groups. In the low- vs. not-low LVEF groups, there was a higher prevalence of heart failure (i.e., history of heart failure hospitalization or New York Heart Association functional class III or IV symptoms) (44.0% vs. 8.3%, respectively), diabetes mellitus, chronic kidney disease, below-the-knee lesion, critical limb ischemia, and incidence of major cardiovascular and cerebrovascular events (MACCEs) and major adverse limb events (MALEs) (P<0.001, all). Low LVEF independently predicted MACCEs (hazard ratio: 2.23, 95% confidence interval: 1.63–3.03; P<0.001) and MALEs (hazard ratio: 1.85, 95% confidence interval: 1.15–2.96; P=0.011), regardless of heart failure (P value for interaction: MACCEs: 0.27; MALEs: 0.52).Conclusions: Low LVEF, but not symptomatic heart failure, increased the incidence of MACCEs and MALEs. Intensive cardiac dysfunction management may improve LEAD prognosis after EVT.
- 著者
- Atsushi Mizuno Chisa Matsumoto Daisuke Yoneoka Takuya Kishi Mari Ishida Shoji Sanada Memori Fukuda Yoshihiko Saito Keiko Yamauchi-Takihara Hiroyuki Tsutsui Keiichi Fukuda Issei Komuro Koichi Node
- 出版者
- The Japanese Circulation Society
- 雑誌
- Circulation Reports (ISSN:24340790)
- 巻号頁・発行日
- vol.3, no.3, pp.137-141, 2021-03-10 (Released:2021-03-10)
- 参考文献数
- 21
- 被引用文献数
- 6
Background:From the early phase of the Coronavirus disease-2019 (COVID-19) pandemic, cardiologists have paid attention not only to COVID-19-associated cardiovascular sequelae, but also to treatment strategies for rescheduling non-urgent procedures. The chief objective of this study was to explore confirmed COVID-19 cardiology case experiences and departmental policies, and their regional heterogeneity in Japan.Methods and Results:We performed a retrospective analysis of a nationwide survey performed by the Japanese Circulation Society on April 13, 2020. The questionnaire included cardiology department experience with confirmed COVID-19 cases and restriction policies, and was sent to 1,360 certified cardiology training hospitals. Descriptive analysis and spatial autocorrelation analysis of each response were performed to reveal the heterogeneity of departmental policies. The response rate was 56.8% (773 replies). Only 16% of all responding hospitals experienced a COVID-19 cardiology case. High-risk procedures were restricted in more than one-fifth of hospitals, including transesophageal echocardiography (34.9%) and scheduled catheterization (39.5%). The presence of a cardiologist in the COVID-19 team, the number of board-certified cardiologists, any medical resource shortage and a state of emergency were positively correlated with any type of restriction.Conclusions:We found both low clinical case experiences with COVID-19 and restrictions of cardiovascular procedures during the first COVID-19 wave in Japan. Restrictions arising as a result of COVID-19 were affected by hospital- and country-level variables, such as a state of emergency.
- 著者
- Tadafumi Sugimoto Atsushi Mizuno Takuya Kishi Naoya Ito Chisa Matsumoto Memori Fukuda Nobuyuki Kagiyama Tatsuhiro Shibata Takashi Ohmori Shogo Oishi Jun Fuse Keisuke Kida Fujimi Kawai Mari Ishida Shoji Sanada Issei Komuro Koichi Node
- 出版者
- The Japanese Circulation Society
- 雑誌
- Circulation Journal (ISSN:13469843)
- 巻号頁・発行日
- vol.84, no.6, pp.1039-1043, 2020-05-25 (Released:2020-05-25)
- 参考文献数
- 37
- 被引用文献数
- 20
Background:Despite the rapidly increasing attention being given to Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) infection, more commonly known as coronavirus disease 2019 (COVID-19), the relationship between cardiovascular disease and COVID-19 has not been fully described.Methods and Results:A systematic review was undertaken to summarize the important aspects of COVID-19 for cardiologists. Protection both for patients and healthcare providers, indication for treatments, collaboration with other departments and hospitals, and regular update of information are essentials to front COVID-19 patients.Conclusions:Because the chief manifestations of COVID-19 infection are respiratory and acute respiratory distress syndrome, cardiologists do not see infected patients directly. Cardiologists need to be better prepared regarding standard disinfection procedures, and be aware of the indications for extracorporeal membrane oxygenation and its use in the critical care setting.
- 著者
- Takuya Kishi Teruyuki Hirano Atsushi Mizuno Yoichiro Hashimoto Chisa Matsumoto Memori Fukuda Shoji Sanada Mari Ishida Koichi Node Susumu Miyamoto Issei Komuro on behalf of Directors of the Japan Stroke and Japanese Circulation Societies
- 出版者
- The Japanese Circulation Society
- 雑誌
- Circulation Reports (ISSN:24340790)
- 巻号頁・発行日
- vol.2, no.6, pp.343-344, 2020-06-10 (Released:2020-06-10)
- 被引用文献数
- 5
- 著者
- Keiko Yamasaki Hiroyuki Sawatari Nao Konagai Chizuko A. Kamiya Jun Yoshimatsu Jun Muneuchi Mamie Watanabe Terunobu Fukuda Atsushi Mizuno Ichiro Sakamoto Kenichiro Yamamura Tomoko Ohkusa Hiroyuki Tsutsui Koichiro Niwa Akiko Chishaki
- 出版者
- The Japanese Circulation Society
- 雑誌
- Circulation Journal (ISSN:13469843)
- 巻号頁・発行日
- vol.83, no.11, pp.2257-2264, 2019-10-25 (Released:2019-10-25)
- 参考文献数
- 38
- 被引用文献数
- 5
Background:The average maternal age at delivery, and thus the associated maternal risk are increasing including in women with congenital heart disease (CHD). A comprehensive management approach is therefore required for pregnant women with CHD. The present study aimed to investigate the factors determining peripartum safety in women with CHD.Methods and Results:We retrospectively collected multicenter data for 217 pregnant women with CHD (age at delivery: 31.4±5.6 years; NYHA classifications I and II: 88.9% and 7.4%, respectively). CHD severity was classified according to the American College of Cardiology/American Heart Association guidelines as simple (n=116), moderate complexity (n=69), or great complexity (n=32). Cardiovascular (CV) events (heart failure: n=24, arrhythmia: n=9) occurred in 30 women during the peripartum period. Moderate or great complexity CHD was associated with more CV events during gestation than simple CHD. CV events occurred earlier in women with moderate or great complexity compared with simple CHD. Number of deliveries (multiparity), NYHA functional class, and severity of CHD were predictors of CV events.Conclusions:This study identified not only the severity of CHD according to the ACC/AHA and NYHA classifications, but also the number of deliveries, as important predictive factors of CV events in women with CHD. This information should be made available to women with CHD and medical personnel to promote safe deliveries.
- 著者
- Masafumi Ono Atsushi Mizuno Nobuyuki Komiyama
- 出版者
- The Editorial Committee of Annals of Vascular Diseases
- 雑誌
- Annals of Vascular Diseases (ISSN:1881641X)
- 巻号頁・発行日
- vol.12, no.1, pp.99-102, 2019-03-25 (Released:2019-03-25)
- 参考文献数
- 10
- 被引用文献数
- 3
A 69-year-old male patient was admitted to our hospital due to sudden right leg pain and paralysis when walking, which was suspected to be acute limb ischemia. Computed tomography and aortography revealed isolated abdominal aortic dissection with bilateral common iliac artery (CIA) stenosis. Endovascular therapy was performed. A Palmaz XL stent (20×40 mm) was deployed on the aortic dissection with intravascular ultrasound assistance. Subsequently, CIA lesions disappeared. Stent deployment at the aortic dissection primary tear resulted in occlusion of the false lumen of the distal dissection of the bilateral CIAs. Postoperatively, his symptoms disappeared, with no recurrence during 14 months of follow-up.
- 著者
- Michiaki Higashitani Yukari Uemura Atsushi Mizuno Makoto Utsunomiya Tetsuo Yamaguchi Akihiro Matsui Shunsuke Ozaki Kazuki Tobita Atsushi Tosaka Akitsugu Oida Kenji Suzuki Takahide Kodama Kentaro Jujo Tatsuki Doijiri Yasuhiro Takahashi Shunsuke Matsuno Nobuhito Kaneko Akira Moriguchi Shohei Kishi Hitoshi Anzai on behalf of Toma-Code Registry Investigators
- 出版者
- The Japanese Circulation Society
- 雑誌
- Circulation Journal (ISSN:13469843)
- 巻号頁・発行日
- pp.CJ-18-0105, (Released:2018-05-11)
- 参考文献数
- 27
- 被引用文献数
- 21
Background:The present study was performed to clarify whether the preoperative clinical symptoms for endovascular therapy (EVT) can predict post-EVT death and cardiovascular prognosis in Japanese patients with peripheral artery disease (PAD), including acute disease.Methods and Results:The TOkyo taMA peripheral vascular intervention research COmraDE (Toma-Code) Registry is a Japanese prospective cohort of 2,321 consecutive patients with PAD treated with EVT, in 34 hospitals in the Kanto and Kōshin’etsu regions, from August 2014 to August 2016. In total, 2,173 symptomatic patients were followed up for a median of 10.4 months, including 1,370 with claudication, 719 with critical limb ischemia (CLI), and 84 with acute limb ischemia (ALI) for EVT. The all-cause death rates per 100 person-years for claudication, CLI and ALI were 3.5, 26.2, and 24.5, respectively. Similarly, major adverse cardiac and cerebrovascular events (MACCE) rates per 100 person-years for claudication, CLI, ALI, and others were 5.2, 31.2, and 29.7, respectively. After adjusting for the predictors of all-cause death and MACCE, namely, age, body mass index <18, diabetes mellitus, dialysis, cerebrovascular disease, and low left ventricular ejection fraction, it was determined that the preoperative indication for EVT was strongly associated with all-cause death and MACCE.Conclusions:The preoperative clinical symptoms for EVT can predict the prognosis in patients with PAD undergoing EVT.
- 著者
- Atsushi Mizuno Takeshi Yamamoto Yasuhiro Tanabe Toru Obayashi Morimasa Takayama Ken Nagao Tokyo CCU Network Scientific Committee
- 出版者
- 日本循環器学会
- 雑誌
- Circulation Journal (ISSN:13469843)
- 巻号頁・発行日
- vol.79, no.4, pp.889-891, 2015-03-25 (Released:2015-03-25)
- 参考文献数
- 11
- 被引用文献数
- 4 8
Background:The Pulmonary Embolism Severity Index (PESI) and simplified PESI (sPESI) have not been fully evaluated in Japan, so the present study aimed to evaluate these risk stratification models in the prediction of mortality of affected patients in Japan.Methods and Results:We retrospectively analysed 302 PE patients (63.9±17.2 years of age; 42.4% male) from January 2011 to December 2012 using data from the Tokyo CCU Network. The areas under the receiver-operating characteristic curves were 0.92 (95% confidence interval (CI): 0.88–0.97) for the PESI and 0.88 (95% CI: 0.77–0.98) for the sPESI.Conclusions:Both scores can be used to predict PE mortality in Japan. (Circ J 2015; 79: 889–891)