- 著者
- Mariko Harada-Shiba Takao Ohta Akira Ohtake Masatsune Ogura Kazushige Dobashi Atsushi Nohara Shizuya Yamashita Koutaro Yokote Joint Working Group by Japan Pediatric Society and Japan Atherosclerosis Society for Making Guidance of Pediatric Familial Hypercholesterolemia
- 出版者
- Japan Atherosclerosis Society
- 雑誌
- Journal of Atherosclerosis and Thrombosis (ISSN:13403478)
- 巻号頁・発行日
- pp.CR002, (Released:2018-02-06)
- 参考文献数
- 49
- 被引用文献数
- 63
This paper describes consensus statement by Joint Working Group by Japan Pediatric Society and Japan Atherosclerosis Society for Making Guidance of Pediatric Familial Hypercholesterolemia (FH) in order to improve prognosis of FH.FH is a common genetic disease caused by mutations in genes related to low density lipoprotein (LDL) receptor pathway. Because patients with FH have high LDL cholesterol (LDL-C) levels from the birth, atherosclerosis begins and develops during childhood which determines the prognosis. Therefore, in order to reduce their lifetime risk for cardiovascular disease, patients with FH need to be diagnosed as early as possible and appropriate treatment should be started.Diagnosis of pediatric heterozygous FH patients is made by LDL-C ≥140 mg/dL, and family history of FH or premature CAD. When the diagnosis is made, they need to improve their lifestyle including diet and exercise which sometimes are not enough to reduce LDL-C levels. For pediatric FH aged ≥10 years, pharmacotherapy needs to be considered if the LDL-C level is persistently above 180 mg/dL. Statins are the first line drugs starting from the lowest dose and are increased if necessary. The target LDL-C level should ideally be <140 mg/dL. Assessment of atherosclerosis is mainly performed by noninvasive methods such as ultrasound.For homozygous FH patients, the diagnosis is made by existence of skin xanthomas or tendon xanthomas from infancy, and untreated LDL-C levels are approximately twice those of heterozygous FH parents. The responsiveness to pharmacotherapy should be ascertained promptly and if the effect of treatment is not enough, LDL apheresis needs to be immediately initiated.
- 著者
- Daisaku Masuda Shizuya Yamashita
- 出版者
- Japan Atherosclerosis Society
- 雑誌
- Journal of Atherosclerosis and Thrombosis (ISSN:13403478)
- 巻号頁・発行日
- vol.24, no.2, pp.95-109, 2017-02-01 (Released:2017-02-01)
- 参考文献数
- 133
- 被引用文献数
- 32 108
Fasting hypertriglyceridemia is positively associated with the morbidity of coronary heart disease (CHD), and postprandial (non-fasting) hypertriglyceridemia is also correlated with the risk status for CHD, which is related to the increase in chylomicron (CM) remnant lipoproteins produced from the intestine. CM remnant particles, as well as oxidized low density lipoprotein (LDL) or very low density lipoprotein (VLDL) remnants, are highly atherogenic and act by enhancing systemic inflammation, platelet activation, coagulation, thrombus formation, and macrophage foam cell formation. The cholesterol levels of remnant lipoproteins significantly correlate with small, dense LDL; impaired glucose tolerance (IGT) and CHD prevalence. We have developed an assay of apolipoprotein (apo)B-48 levels to evaluate the accumulation of CM remnants. Fasting apoB-48 levels correlate with the morbidity of postprandial hypertriglyceridemia, obesity, type III hyperlipoproteinemia, the metabolic syndrome, hypothyroidism, chronic kidney disease, and IGT. Fasting apoB-48 levels also correlate with carotid intima-media thickening and CHD prevalence, and a high apoB-48 level is a significant predictor of CHD risk, independent of the fasting TG level. Diet interventions, such as dietary fibers, polyphenols, medium-chain fatty acids, diacylglycerol, and long-chain n-3 polyunsaturated fatty acids (PUFA), ameliorate postprandial hypertriglyceridemia, moreover, drugs for dyslipidemia (n-3 PUFA, statins, fibrates or ezetimibe) and diabetes concerning incretins (dipeptidyl-peptidase IV inhibitor or glucagon like peptide-1 analogue) may improve postprandial hypertriglyceridemia. Since the accumulation of CM remnants correlates to impaired lipid and glucose metabolism and atherosclerotic cardiovascular events, further studies are required to investigate the characteristics, physiological activities, and functions of CM remnants for the development of new interventions to reduce atherogenicity.
- 著者
- Mariko Harada-Shiba Hidenori Arai Yasushi Ishigaki Shun Ishibashi Tomonori Okamura Masatsune Ogura Kazushige Dobashi Atsushi Nohara Hideaki Bujo Katsumi Miyauchi Shizuya Yamashita Koutaro Yokote Working Group by Japan Atherosclerosis Society for Making Guidance of Familial Hypercholesterolemia
- 出版者
- Japan Atherosclerosis Society
- 雑誌
- Journal of Atherosclerosis and Thrombosis (ISSN:13403478)
- 巻号頁・発行日
- pp.CR003, (Released:2018-06-07)
- 参考文献数
- 74
- 被引用文献数
- 167
Statement1. Familial hypercholesterolemia (FH) is an autosomal hereditary disease with the 3 major clinical features of hyper-LDL-cholesterolemia, premature coronary artery disease and tendon and skin xanthomas. As there is a considerably high risk of coronary artery disease, in addition to early diagnosis and intensive treatment, family screening (cascade screening) is required (Recommendation level A)2.For a diagnosis of FH, at least 2 of the following criteria should be satisfied:① LDL-C ≥180 mg/dL, ② Tendon/skin xanthomas, ③ History of FH or premature coronary artery disease (CAD) within 2nd degree blood relatives (Recommendation level A)3. Intensive lipid-lowering therapy is necessary for the treatment of FH. First-line drug should be statin. (Recommendation level A, evidence level 3)4.Screening for coronary artery disease as well as asymptomatic atherosclerosis should be conducted periodically in FH patients. (Recommendation level A)5. For homozygous FH, consider LDL apheresis and treatment with PCSK9 inhibitors or MTP inhibitors. (Recommendation level A)6.For severe forms of heterozygous FH who have resistant to drug therapy, consider PCSK9 inhibitors and LDL apheresis. (Recommendation level A)7.Refer FH homozygotes as well as heterozygotes who are resistant to drug therapy, who are children or are pregnant or have the desire to bear children to a specialist. (Recommendation level A)
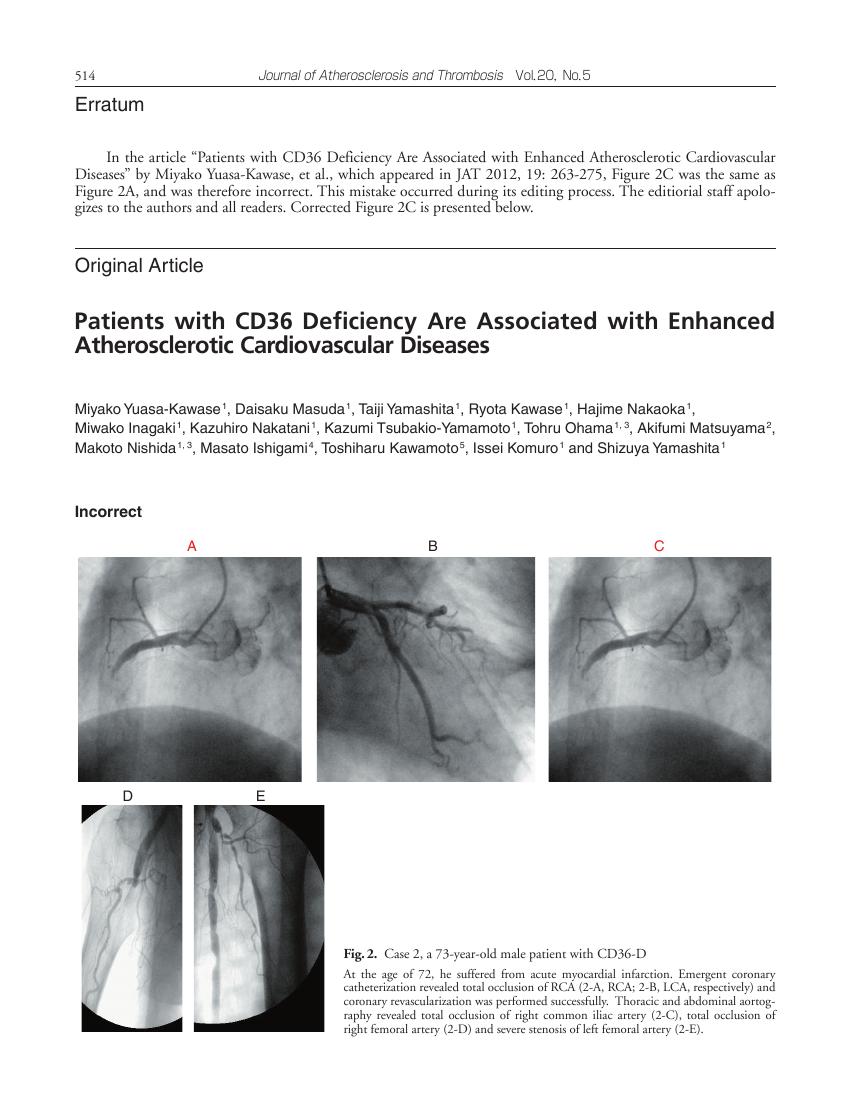
4 0 0 0 OA Patients with CD36 Deficiency Are Associated with Enhanced Atherosclerotic Cardiovascular Diseases
- 著者
- Miyako Yuasa-Kawase Daisaku Masuda Taiji Yamashita Ryota Kawase Hajime Nakaoka Miwako Inagaki Kazuhiro Nakatani Kazumi Tsubakio-Yamamoto Tohru Ohama Akifumi Matsuyama Makoto Nishida Masato Ishigami Toshiharu Kawamoto Issei Komuro Shizuya Yamashita
- 出版者
- 一般社団法人 日本動脈硬化学会
- 雑誌
- Journal of Atherosclerosis and Thrombosis (ISSN:13403478)
- 巻号頁・発行日
- vol.19, no.3, pp.263-275, 2012 (Released:2012-03-26)
- 参考文献数
- 48
- 被引用文献数
- 9 32
Aim: The clustering of dyslipidemia, impaired glucose tolerance and hypertension increases the morbidity and mortality from cardiovascular events. A class B scavenger receptor, CD36, is a receptor for oxidized LDL and a transporter of long-chain fatty acids. Because of the impaired uptake of oxidized LDL in CD36-deficient macrophages and from the results of CD36 knockout mice, CD36 deficiency (CD36-D) was supposed to be associated with reduced risks for coronary artery disease (CAD); however, CD36-D patients are often accompanied by a clustering of coronary risk factors. The current study aimed to investigate the morbidity and severity of cardiovascular diseases in CD36-D patients.Methods: By screening for CD36 antigen on platelets and monocytes using FACS or the absent myocardial accumulation of 123I-BMIPP by scintigraphy, 40 patients with type I CD36-D were collected, the morbidity of CAD and their features of atherosclerotic cardiovascular diseases were observed. Screening for CD36-D in both CAD patients (n =319) and healthy subjects (n =1,239) were underwent.Results: The morbidity of CAD was significantly higher in CD36-D patients than in the general population; 50% of patients (20 out of 40) had CAD identified by BMIPP scintigraphy and 37.5% (3 out of 8) by FACS screening, respectively. Three representative CD36-D cases demonstrated severe CAD and atherosclerosis. The frequency of CD36-D was three times higher in CAD patients than in healthy subjects (0.9% vs 0.3%, p <0.0001).Conclusion: The morbidity of CAD is significantly higher in CD36-D patients suffering from severe atherosclerosis, implying that the status of CD36-D might be atherogenic.
- 著者
- Makoto Kinoshita Koutaro Yokote Hidenori Arai Mami Iida Yasushi Ishigaki Shun Ishibashi Seiji Umemoto Genshi Egusa Hirotoshi Ohmura Tomonori Okamura Shinji Kihara Shinji Koba Isao Saito Tetsuo Shoji Hiroyuki Daida Kazuhisa Tsukamoto Juno Deguchi Seitaro Dohi Kazushige Dobashi Hirotoshi Hamaguchi Masumi Hara Takafumi Hiro Sadatoshi Biro Yoshio Fujioka Chizuko Maruyama Yoshihiro Miyamoto Yoshitaka Murakami Masayuki Yokode Hiroshi Yoshida Hiromi Rakugi Akihiko Wakatsuki Shizuya Yamashita Committee for Epidemiology and Clinical Management of Atherosclerosis
- 出版者
- Japan Atherosclerosis Society
- 雑誌
- Journal of Atherosclerosis and Thrombosis (ISSN:13403478)
- 巻号頁・発行日
- vol.25, no.9, pp.846-984, 2018-09-01 (Released:2018-09-01)
- 参考文献数
- 999
- 被引用文献数
- 347 534
- 著者
- Hayato Tada Akihiro Nomura Masatsune Ogura Katsunori Ikewaki Yasushi Ishigaki Kyoko Inagaki Kazuhisa Tsukamoto Kazushige Dobashi Kimitoshi Nakamura Mika Hori Kota Matsuki Shizuya Yamashita Shinji Yokoyama Masa-aki Kawashiri Mariko Harada-Shiba on behalf of the Committee on Primary Dyslipidemia under the Research Program on Rare and Intractable Desease of the Ministry of Health Labour and Welfare of Japan
- 出版者
- Japan Atherosclerosis Society
- 雑誌
- Journal of Atherosclerosis and Thrombosis (ISSN:13403478)
- 巻号頁・発行日
- pp.RV17052, (Released:2021-04-28)
- 参考文献数
- 56
- 被引用文献数
- 36
Sitosterolemia is an inherited metabolic disorder characterized by increased levels of plant sterols, such as sitosterol. This disease is caused by loss-of-function genetic mutations in ATP-binding cassette (ABC) subfamily G member 5 or member 8 (ABCG5 or ABCG8, respectively), both of which play important roles in selective excretion of plant sterols from the liver and intestine, leading to failure to prevent absorption of food plant sterols. This disorder has been considered to be extremely rare. However, accumulated clinical data as well as genetics suggest the possibility of a much higher prevalence. Its clinical manifestations resemble those observed in patients with familial hypercholesterolemia (FH), including tendon xanthomas, hyper LDL-cholesterolemia, and premature coronary atherosclerosis. We provide an overview of this recessive genetic disease, diagnostic as well as therapeutic tips, and the latest diagnostic criteria in Japan.
- 著者
- Atsushi Hirayama Shizuya Yamashita Andrea Ruzza Hyoe Inomata Marcoli Cyrille Chen Lu Andrew W. Hamer Masayuki Yoshida Arihiro Kiyosue Tamio Teramoto
- 出版者
- The Japanese Circulation Society
- 雑誌
- Circulation Journal (ISSN:13469843)
- 巻号頁・発行日
- vol.83, no.5, pp.971-977, 2019-04-25 (Released:2019-04-25)
- 参考文献数
- 11
- 被引用文献数
- 1
Background: Treatment with evolocumab reduces mean low-density lipoprotein cholesterol (LDL-C) up to 75% and cardiovascular events by 16% in the first year and 25% thereafter. Methods and Results: Japanese patients with hypercholesterolemia enrolled in the parent YUKAWA-1-2 studies could enroll, once eligible, in the OSLER studies (n=556). OSLER re-randomized patients 2:1 to evolocumab plus standard of care (SOC; evolocumab+SOC) or SOC alone for 1 year; after year 1, patients could enter the all-evolocumab+SOC open-label extension of OSLER. Patients received evolocumab+SOC from the 2nd year through up to 5 years. Long-term efficacy and safety, including antidrug antibodies, were evaluated. Of 556 patients, 532 continued to the all-evolocumab+SOC extension: mean (standard deviation [SD]) age 61 (10) years, 39% female. A total of 91% of 532 patients completed the studies. Mean (SD) LDL-C change from parent-study baseline with evolocumab from a mean (SD) baseline of 142.3 (21.3) and 105.0 (31.1) mg/dL in OSLER-1 and OSLER-2, respectively, was maintained through the end of the study: −58.0% (19.1%) at year 5 in OSLER-1, −62.7% (25.6%) at year 3 in OSLER-2. The overall safety profile of the evolocumab+SOC periods was similar to that of the year-1 controlled period. Antidrug antibodies were detected transiently in 3 patients. No neutralizing antibodies were detected. Conclusions: Japanese patients who continued evolocumab+SOC for up to 5 years experienced sustained high LDL-C level reduction. Long-term evolocumab+SOC exposure showed no new safety signals.
2 0 0 0 OA Patients with CD36 Deficiency Are Associated with Enhanced Atherosclerotic Cardiovascular Diseases
- 著者
- Miyako Yuasa-Kawase Daisaku Masuda Taiji Yamashita Ryota Kawase Hajime Nakaoka Miwako Inagaki Kazuhiro Nakatani Kazumi Tsubakio-Yamamoto Tohru Ohama Akifumi Matsuyama Makoto Nishida Masato Ishigami Toshiharu Kawamoto Issei Komuro Shizuya Yamashita
- 出版者
- 一般社団法人 日本動脈硬化学会
- 雑誌
- Journal of Atherosclerosis and Thrombosis (ISSN:13403478)
- 巻号頁・発行日
- vol.20, no.5, pp.514-515, 2013 (Released:2013-05-29)
- 参考文献数
- 48
- 著者
- Hironobu Mitani Kota Suzuki Junya Ako Kazuma Iekushi Renata Majewska Salsabil Touzeni Shizuya Yamashita
- 出版者
- Japan Atherosclerosis Society
- 雑誌
- Journal of Atherosclerosis and Thrombosis (ISSN:13403478)
- 巻号頁・発行日
- vol.30, no.11, pp.1622-1634, 2023-11-01 (Released:2023-11-01)
- 参考文献数
- 32
- 被引用文献数
- 6
Aims: The study aimed to investigate low-density lipoprotein cholesterol (LDL-C) goal achievement rates in patients receiving LDL-C-lowering therapy using recent real-world data, following the 2017 revision of the Japan Atherosclerosis Society Guidelines for Prevention of Atherosclerotic Cardiovascular Diseases (JAS GL2017). Methods: Patients with documented LDL-C test results were extracted from the Medical Data Vision claims database between July 2018 and June 2021 and divided into three groups according to JAS GL2017: primary prevention high risk (Group I, LDL-C goal <120 mg/dL), secondary prevention (Group II, LDL-C goal <100 mg/dL), and secondary prevention high risk (Group III, LDL-C goal <70 mg/dL). Results: The mean LDL-C value was 108.7 mg/dL (n=125,235), 94.4 mg/dL (n=57,910), and 90.6 mg/dL (n=33,850) in Groups I, II, and III, respectively. Intensive statin monotherapy (pitavastatin, rosuvastatin, or atorvastatin) was the most frequently prescribed lipid-lowering treatment (21.6%, 30.8%, and 42.7% in Groups I, II, and III, respectively), followed by ezetimibe (2.5%, 7.1%, and 8.5% in Groups I, II, and III, respectively). LDL-C goals were achieved by 65.5%, 60.6%, and 25.4% of patients overall in Groups I, II, and III, respectively. Achievement rates were 83.9%, 75.3%, and 29.5% in patients prescribed intensive statin monotherapy and 82.3%, 86.4%, and 46.4% in those prescribed statin and ezetimibe combinations in Groups I, II, and III, respectively. In Group III, the proportion of patients with familial hypercholesterolemia prescribed statin and ezetimibe combinations achieving LDL-C goals was low (32.5%). Conclusions: The proportion of patients achieving LDL-C goals for secondary prevention in the high-risk group remains low even with statin and ezetimibe combination therapy.
- 著者
- Mariko Harada-Shiba Hidenori Arai Shinichi Oikawa Takao Ohta Tomoo Okada Tomonori Okamura Atsushi Nohara Hideaki Bujo Koutaro Yokote Akihiko Wakatsuki Shun Ishibashi Shizuya Yamashita
- 出版者
- Japan Atherosclerosis Society
- 雑誌
- Journal of Atherosclerosis and Thrombosis (ISSN:13403478)
- 巻号頁・発行日
- vol.19, no.12, pp.1043-1060, 2012 (Released:2012-12-20)
- 参考文献数
- 85
- 被引用文献数
- 144 146
Familial hypercholesterolemia (FH) is a highly prevalent autosomal dominant hereditary disease, generally characterized by three major signs, hyper-low-density-lipoprotein (LDL) cholesterolemia, tendon/skin xanthomas and premature coronary artery disease (CAD). Because the risk of CAD is very high in these patients, they should be identified at an early stage of their lives and started on intensive treatment to control LDL-cholesterol. We here introduce a new guideline for the management of FH patients in Japan intending to achieve better control to prevent CAD. Diagnostic criteria for heterozygous FH are 2 or more of 1) LDL-cholesterol ≥180 mg/dL, 2) tendon/skin xanthoma(s), and 3) family history of FH or premature CAD within second degree relatives, for adults; and to have both 1) LDL-cholesterol ≥140 mg/dL and 2) family history of FH or premature CAD within second degree relatives, for children. For the treatment of adult heterozygous FH, intensive lipid control with statins and other drugs is necessary. Other risks of CAD, such as smoking, diabetes mellitus, hypertension etc., should also be controlled strictly. Atherosclerosis in coronary, carotid, or peripheral arteries, the aorta and aortic valve should be screened periodically. FH in children, pregnant women, and women who wish to bear a child should be referred to specialists. For homozygotes and severe heterozygotes resistant to drug therapies, LDL apheresis should be performed. The treatment cost of homozygous FH is authorized to be covered under the program of Research on Measures against Intractable Diseases by the Japanese Ministry of Health, Labour, and Welfare.
- 著者
- Hidenori Arai Hideaki Bujo Daisaku Masuda Toshiyuki Ishibashi Satoshi Nakagawa Kenichiro Tanabe Tatsuo Kagimura Hyun-Jae Kang Moo Hyun Kim Jidong Sung Sang-Hyun Kim Cheol-Ho Kim Jeong Euy Park Junbo Ge Byung-Hee Oh Toru Kita Yasushi Saito Masanori Fukushima Yuji Matsuzawa Shizuya Yamashita
- 出版者
- Japan Atherosclerosis Society
- 雑誌
- Journal of Atherosclerosis and Thrombosis (ISSN:13403478)
- 巻号頁・発行日
- pp.62821, (Released:2021-04-18)
- 参考文献数
- 45
- 被引用文献数
- 6
Aims: In this study, we integrated two randomized control trials, PROSPECTIVE and IMPACT, to address the effect of probucol on cerebrocardiovascular events and carotid intima-media thickness (IMT) in Japanese, Korean, and Chinese patients with coronary artery disease (CAD). Methods: A total of 1,025 patients from the PROSPECTIVE and IMPACT studies were enrolled. The time to the first major adverse cerebrocardiovascular event, in addition to carotid IMT and lipid levels, was compared between the control and probucol groups. Results: In the integrated analysis, the adjusted hazard ratio (HR) and 95% confidence interval (CI) were 0.67 and 0.44–1.03, respectively, indicating a tendency to show the effect of probucol on cerebrocardiovascular events in secondary prevention. We also found no significant differences between the control and probucol groups in the mean IMT of the carotid arteries and its changes. However, we found a significant decrease in cerebrocardiovascular events in patients with reduced levels of HDL cholesterol (HDL-C) (≥ 6.25 mg/dL) compared with those with levels <6.25 mg/dL (p=0.024), without any increase in adverse events such as severe ventricular arrhythmias. Conclusion: We demonstrated a marginal effect of probucol on cerebrocardiovascular events in Asian patients with CAD, with reasonable safety profiles. A larger study may be needed to support the effect of probucol for cardiovascular prevention.
- 著者
- Shizuya Yamashita Hidenori Arai Hideaki Bujo Daisaku Masuda Tohru Ohama Toshiyuki Ishibashi Koji Yanagi Yasuji Doi Satoshi Nakagawa Koichi Yamashiro Kenichiro Tanabe Toru Kita Masunori Matsuzaki Yasushi Saito Masanori Fukushima Yuji Matsuzawa on Behalf of the PROSPECTIVE Study Group
- 出版者
- Japan Atherosclerosis Society
- 雑誌
- Journal of Atherosclerosis and Thrombosis (ISSN:13403478)
- 巻号頁・発行日
- pp.55327, (Released:2020-04-24)
- 参考文献数
- 50
- 被引用文献数
- 26
Aims: Although intensive statin therapy reduced cardiovascular risks, cardiovascular events have not been completely prevented. Probucol is a potent antioxidant and reduces tendon xanthomas in familial hypercholesterolemia patients despite reduction of high-density lipoprotein (HDL)-cholesterol (HDL-C). We investigated whether probucol can reduce cardiovascular events on top of conventional lipid-lowering therapy in patients with coronary heart disease (CHD). Methods: PROSPECTIVE is a multicenter, randomized, prospective study that recruited 876 Japanese patients with CHD and dyslipidemia with an low-density lipoprotein (LDL)-cholesterol (HDL-C) level of ≥ 140 mg/dL without medication or those treated with lipid-lowering drugs. Lipid-lowering agents were administered during the study period in the control group (n=438), and probucol 500 mg/day was added to lipid-lowering therapy in the probucol group (n=438). Patients were randomly assigned to two treatment groups by adjusting the LDL-C level and presence of diabetes and hypertension and followed up for more than 3 years. The primary end point was a composite of cerebrovascular and cardiovascular events (cardiovascular disease death including sudden death, nonfatal myocardial infarction, nonfatal stroke, hospitalization for unstable angina, hospitalization for heart failure, or coronary revascularization). The secondary end point was carotid intima–media thickness in a subset of patients. Results: The incidence of the primary end point showed a trend to be lower in the probucol group compared with that in the control group despite reduced HDL-C without serious adverse events. Anti-atherogenic effects of probucol may be attributed to its potent antioxidative function and enhancement of reverse cholesterol transport. Conclusion: Since there was no statistical significance between the probucol and control groups despite a marked reduction of HDL-C, further studies on the clinical outcomes of probucol on top of conventional therapy may be necessary in the future (UMIN000003307).
1 0 0 0 OA Reference Intervals of Serum Non-Cholesterol Sterols by Gender in Healthy Japanese Individuals
- 著者
- Hiroshi Yoshida Hayato Tada Kumie Ito Yoshimi Kishimoto Hidekatsu Yanai Tomonori Okamura Katsunori Ikewaki Kyoko Inagaki Tetsuo Shoji Hideaki Bujo Takashi Miida Masayuki Yoshida Masafumi Kuzuya Shizuya Yamashita
- 出版者
- Japan Atherosclerosis Society
- 雑誌
- Journal of Atherosclerosis and Thrombosis (ISSN:13403478)
- 巻号頁・発行日
- pp.50187, (Released:2019-09-05)
- 参考文献数
- 26
- 被引用文献数
- 28
Aims: The present study was conducted to establish a practical method for measuring non-cholesterol sterols and reference intervals of serum levels.Methods: Healthy subjects (109 men and 151 women), four patients with sitosterolemia, and 10 heterozygous mutation carriers of ABCG5/ABCG8 genes were investigated. Then, three non-cholesterol sterols (sitosterol, campesterol, and lathosterol) of fasting serum samples were measured via a practical and highly sensitive gas chromatography (GC) method with 0.2 µg/mL as the lower limit of quantification. The coefficient of variation (CV) values for within-run reproducibility were 3.06%, 1.89%, and 1.77% for lathosterol, campesterol, and sitosterol, respectively. The CV values for between-run reproducibility were 2.81%, 2.06%, and 2.10% for lathosterol, campesterol, and sitosterol, respectively.Results: The serum levels of sitosterol and campesterol were significantly higher in women than in men, whereas the serum levels of lathosterol were significantly higher in men than in women. Because of these gender difference, the determination of reference intervals of the three sterol values was performed by considering gender. The reference intervals of sitosterol, campesterol, and lathosterol were 0.99–3.88, 2.14–7.43, and 0.77–3.60 µg/mL in men and 1.03–4.45, 2.19–8.34, and 0.64–2.78 µg/mL in women, respectively. The serum levels of sitosterol and campesterol were higher in patients with sitosterolemia (94.3±47.3 and 66.3±36.6 µg/mL, respectively) than in healthy subjects.Conclusion: These results demonstrate a practical and highly sensitive GC method to measure non-cholesterol sterol levels and gender-segregated reference intervals of sitosterol, campesterol, and lathosterol in Japanese healthy subjects.
- 著者
- Atsushi Hirayama Narimon Honarpour Masayuki Yoshida Shizuya Yamashita Fannie Huang Scott M. Wasserman Tamio Teramoto
- 出版者
- 日本循環器学会
- 雑誌
- Circulation Journal (ISSN:13469843)
- 巻号頁・発行日
- pp.CJ-14-0130, (Released:2014-03-21)
- 参考文献数
- 38
- 被引用文献数
- 30 83 26
Background: YUKAWA is a 12-week, randomized, double-blind, placebocontrolled, phase 2 study evaluating the efficacy and safety of evolocumab (AMG 145) in statin-treated Japanese patients at high cardiovascular risk. Methods and Results: 310 eligible patients receiving stable statin (±ezetimibe) therapy were randomized to 1 of 6 treatments: placebo every 2 weeks (Q2W) or monthly (QM), evolocumab 70mg or 140mg Q2W, or evolocumab 280mg or 420mg QM. The primary endpoint was the percentage change from baseline in low-density lipoprotein cholesterol (LDL-C) measured by preparative ultracentrifugation (UC). Secondary endpoints included percentage changes in other lipid parameters and the proportion of patients with LDL-C <1.8mmol/L. Mean (SD) age was 62 (10) years; 37% were female; and the mean (SD) baseline LDL-C was 3.7 (0.5) mmol/L (by UC). Mean (SE) changes vs. placebo in LDL-C were greatest in the high-dose groups: −68.6 (3.0) % and −63.9 (3.2) % with 140mg Q2W and 420mg QM dosing, respectively. Up to 96% of evolocumab-treated patients achieved LDL-C <1.8mmol/L. Adverse events (AEs) were more frequent in evolocumab (51%) vs. placebo (38%) patients; 4 patients taking evolocumab discontinued treatment because of an AE. There were no significant differences in AE rates based on dose or dose frequency. Conclusions: In Japanese patients at high cardiovascular risk with hypercholesterolemia on stable statin therapy, evolocumab significantly reduced LDL-C and was well tolerated during this 12-week study.