- 著者
- Shi-Lin Tang Zhen-Wang Zhao Shang-Ming Liu Gang Wang Xiao-Hua Yu Jin Zou Si-Qi Wang Xiao-Yan Dai Min-Gui Fu Xi-Long Zheng Da-Wei Zhang Hui Fu Chao-Ke Tang
- 出版者
- The Japanese Circulation Society
- 雑誌
- Circulation Journal (ISSN:13469843)
- 巻号頁・発行日
- pp.CJ-18-0700, (Released:2019-01-18)
- 参考文献数
- 41
- 被引用文献数
- 25
Background: Recent studies have suggested that pregnancy-associated plasma protein-A (PAPP-A) is involved in the pathogenesis of atherosclerosis. This study aim is to investigate the role and mechanisms of PAPP-A in reverse cholesterol transport (RCT) and inflammation during the development of atherosclerosis. Methods and Results: PAPP-A was silenced in apolipoprotein E (apoE−/−) mice with administration of PAPP-A shRNA. Oil Red O staining of the whole aorta root revealed that PAPP-A knockdown reduced lipid accumulation in aortas. Oil Red O, hematoxylin and eosin (HE) and Masson staining of aortic sinus further showed that PAPP-A knockdown alleviated the formation of atherosclerotic lesions. It was found that PAPP-A knockdown reduced the insulin-like growth factor 1 (IGF-1) levels and repressed the PI3K/Akt pathway in both aorta and peritoneal macrophages. The expression levels of LXRα, ABCA1, ABCG1, and SR-B1 were increased in the aorta and peritoneal macrophages from apoE−/−mice administered with PAPP-A shRNA. Furthermore, PAPP-A knockdown promoted RCT from macrophages to plasma, the liver, and feces in apoE−/−mice. In addition, PAPP-A knockdown elevated the expression and secretion of monocyte chemoattractant protein-1 (MCP-1), interleukin-6 (IL-6), tumor necrosis factor-α, and interleukin-1β through the nuclear factor kappa-B (NF-κB) pathway. Conclusions: The present study results suggest that PAPP-A promotes the development of atherosclerosis in apoE−/−mice through reducing RCT capacity and activating an inflammatory response.
1 0 0 0 OA Impending Epidemic
- 著者
- Yuji Okura Mahmoud M. Ramadan Yukiko Ohno Wataru Mitsuma Komei Tanaka Masahiro Ito Keisuke Suzuki Naohito Tanabe Makoto Kodama Yoshifusa Aizawa
- 出版者
- The Japanese Circulation Society
- 雑誌
- Circulation Journal (ISSN:13469843)
- 巻号頁・発行日
- vol.72, no.3, pp.489-491, 2008 (Released:2008-02-25)
- 参考文献数
- 9
- 被引用文献数
- 61 290
Background The future burden of heart failure in Japan was projected to 2055 in order to prospectively estimate of the number of these patients. Methods and Results The statistics are based on prevalence data of left ventricular dysfunction (LVD) in Sado City using the Sado Heart Failure Study (2003) and population estimates from the Japanese National Institute of Population and Social Security Research Report (2006). The number of Japanese outpatients with LVD was 979,000 in 2005, and is predicted to increase gradually as the population ages, reaching 1.3 million by 2030. Conclusion LVD is expected to precipitate a future epidemic of heart failure in Japan. (Circ J 2008; 72: 489 - 491)
- 著者
- Masaomi Gohbara Kunihiro Nishimura Michikazu Nakai Yoko Sumita Tsutomu Endo Yasushi Matsuzawa Masaaki Konishi Masami Kosuge Toshiaki Ebina Kouichi Tamura Kazuo Kimura
- 出版者
- The Japanese Circulation Society
- 雑誌
- Circulation Reports (ISSN:24340790)
- 巻号頁・発行日
- vol.1, no.1, pp.20-28, 2019-01-10 (Released:2019-01-10)
- 参考文献数
- 30
- 被引用文献数
- 7
Background: The aim of this study was to clarify the clinical impact of activities of daily living (ADL) using the Japanese Registry of All Cardiac and Vascular Diseases-Diagnosis Procedure Combination (JROAD-DPC) database. Methods and Results: From April 2012 to March 2014, the JROAD-DPC database included 206,643 patients with acute coronary syndrome (ACS; n=49,784), heart failure (HF; n=136,878), or aortic aneurysm/dissection (Aorta; n=19,981). We divided them into 3 categories with regard to age (low, 20–59 years; middle, 60–79 years; high, ≥80 years) and admission ADL (low, Barthel index [BI] 0–70; middle, BI 75–95; high, BI 100). ACS, HF, and Aorta patients with low ADL had higher in-hospital mortality rates (18.3%, 16.7%, and 33.4%) than those with middle or high ADL (P<0.001, χ2 test). On multivariable analysis, BI on admission was associated with in-hospital mortality of ACS (OR, 0.986 per 1 BI; P<0.001), HF (OR, 0.986 per 1 BI; P<0.001), and Aorta (OR, 0.986 per 1 BI; P<0.001), adjusted for gender, age, body mass index, hypertension, diabetes mellitus, dyslipidemia, and the Charlson comorbidity index. Moreover, patients with low age and low ADL had a higher in-hospital mortality rate than those with high age and high ADL in regard to HF (8.6% vs. 6.0%). Conclusions: According to JROAD-DPC data, assessment of admission ADL is important in patients with cardiovascular disease.
- 著者
- Takashi Oki Hirokazu Miyoshi Yoshifumi Oishi Arata Iuchi Kenya Kusunose Hirotsugu Yamada Allan L. Klein
- 出版者
- The Japanese Circulation Society
- 雑誌
- Circulation Reports (ISSN:24340790)
- 巻号頁・発行日
- vol.1, no.1, pp.8-16, 2019-01-10 (Released:2019-01-10)
- 参考文献数
- 67
- 被引用文献数
- 4
At present, heart failure with preserved ejection fraction (HFpEF) is a commonly accepted condition in HF patients. In contrast to HF with reduced EF (HFrEF), HFpEF is strongly associated with aging, and vascular, metabolic, neurohormonal, and systemic inflammatory comorbidities. Two major hypotheses explain the pathophysiology of HFpEF (stages C,D in the American College of Cardiology Foundation/American Heart Association HF staging system): (1) impaired active relaxation and increased passive stiffness of the left ventricular (LV) myocardium during diastole (left atrial [LA]-LV coupling); and (2) LV and arterial stiffening during systole (LV-arterial coupling). Cardiac structural and functional abnormalities can be evaluated using non-invasive measures, such as 2-D, flow velocity Doppler, and tissue Doppler echocardiography, to estimate LV filling pressure and afterload mismatch. The clinical application of 2-D speckle-tracking echocardiography (2D-STE) is feasible for earlier diagnosis of functional abnormalities of the LA, LV, and elastic arteries in asymptomatic patients with cardiovascular risk factors (stages A,B). The goal of this review is to highlight the role of 2D-STE to detect impairment of LA-LV-arterial coupling beyond diastolic function earlier, because it may provide important information on the pathophysiology and prevention of HFpEF.
- 著者
- Shingo Minatoguchi Takahiro Ando Toshiki Tanaka Yoshihisa Yamada Hiromitsu Kanamori Masanori Kawasaki Kazuhiko Nishigaki Shinya Minatoguchi
- 出版者
- The Japanese Circulation Society
- 雑誌
- Circulation Reports (ISSN:24340790)
- 巻号頁・発行日
- vol.1, no.1, pp.17-19, 2019-01-10 (Released:2019-01-10)
- 参考文献数
- 9
- 被引用文献数
- 3
Background: It is still unclear whether dynamic exercise increases the number of Muse cells, pluripotent stem cells, in the peripheral blood. Methods and Results: The number of Muse cells, SSEA3+ and CD105+ double-positive cells, in the peripheral blood was measured using FACS before and after 40 min of cardiac rehabilitation with dynamic exercise in 6 patients with heart disease. The number of Muse cells significantly increased after cardiac rehabilitation in all patients. Muse cell mobilization may be related to the beneficial clinical outcome of cardiac rehabilitation. Conclusions: Cardiac rehabilitation increases the number of Muse cells in the peripheral blood.
- 著者
- Hiroshi Matsuo Kaoru Dohi Hirofumi Machida Hideyuki Takeuchi Toshikazu Aoki Hiroyuki Nishimura Masashi Yasutomi Michiharu Senga Takehiko Ichikawa Kentaro Kakuta Yasuhide Mizutani Akiko Tanoue Naoki Isaka Kazuki Oosugi Sukenari Koyabu Masato Sakurai Yoshihisa Fukui Hitoshi Kakimoto Tadafumi Sugimoto Takahiro Ohnishi Tomohiro Murata Eiji Ishikawa Ryuji Okamoto Tomomi Yamada Toru Ogura Yuki Nishimura Takashi Tanigawa Shinsuke Nomura Masakatsu Nishikawa Masaaki Ito
- 出版者
- The Japanese Circulation Society
- 雑誌
- Circulation Journal (ISSN:13469843)
- 巻号頁・発行日
- vol.82, no.2, pp.586-595, 2018-01-25 (Released:2018-01-25)
- 参考文献数
- 37
- 被引用文献数
- 29
Background:The aim of this study was to assess the echocardiographic characteristics of chronic hemodialysis (HD) patients with end-stage renal disease (ESRD) in a multicenter prospective cohort study.Methods and Results:Three hundred and fifteen patients with ESRD (67.9±10.6 years, 47.6% male) on chronic HD for ≥1 year were examined on transthoracic echocardiography, including Doppler-derived aortic valve area (AVA) measurement. Only 11.5% and 3.4% of all patients had normal left ventricular (LV) geometry and normal LV filling pattern, respectively. The majority of patients had aortic and mitral valvular calcification, and approximately 50% of all 315 patients had aortic valve narrowing with AVA <2.0 cm2. Patients were divided into 3 groups according to AVA index tertile: group 1, highest tertile; group 2, middle tertile; and group 3, lowest tertile. Group 3 was older, had a greater cardiothoracic ratio on chest X-ray, higher plasma brain natriuretic peptide and total LV afterload, and lower stroke volume index than the other 2 groups. Age and intact parathyroid hormone (PTH) level were independently associated with low AVA index.Conclusions:Patients with ESRD on chronic HD have a high prevalence of cardiac structural and functional abnormalities including calcified aortic sclerosis. High age and PTH were associated with aortic valve narrowing in these patients.
- 著者
- Tadafumi Sugimoto Kaoru Dohi Katsuya Onishi Tomomi Yamada Masahide Horiguchi Takeshi Takamura Akihiro Kawamura Tetsuya Seko Mashio Nakamura Atsunobu Kasai Masaaki Ito
- 出版者
- The Japanese Circulation Society
- 雑誌
- Circulation Journal (ISSN:13469843)
- 巻号頁・発行日
- vol.78, no.11, pp.2704-2710, 2014-10-24 (Released:2014-10-24)
- 参考文献数
- 42
- 被引用文献数
- 3 6
Background:Secondary hyperparathyroidism develops as a compensatory response to chronic heart failure (HF) and renal failure. The role of parathyroid hormone (PTH) level in acute decompensated HF remains unclear. The aim of this study was therefore to investigate the relationships among mortality, renal function, and serum PTH level in acute decompensated HF patients.Methods and Results:A total of 266 consecutive patients admitted for acute decompensated HF without acute coronary syndrome (78±12 years; 48% male) were enrolled. Demographic, clinical, and laboratory characteristics were obtained on admission.During 1-year follow-up, 65 patients (24%) died. Serum PTH level on admission was within the normal range (10–65 pg/ml) in 108 patients (41%), of whom 39 (15%) had low-normal PTH (10–40 pg/ml). On Kaplan-Meier analysis all-cause mortality was significantly higher in patients with low-normal PTH than in those with high-normal (40–65 pg/ml) or high (>65 pg/ml) PTH (log-rank test). On univariate and multivariate Cox regression analysis, low-normal PTH was significantly associated with increased all-cause mortality (unadjusted HR, 2.88; 95% CI: 1.69–4.91; P<0.001; adjusted HR, 3.84; 95% CI: 1.54–9.57; P=0.004).Conclusions:In patients with acute decompensated HF resulting in hospitalization, low-normal PTH on admission is associated with increased all-cause mortality, regardless of renal function. (Circ J 2014; 78: 2704–2710)
- 著者
- Kohei Takata Satoshi Imaizumi Emi Kawachi Yasunori Suematsu Tomohiko Shimizu Satomi Abe Yoshino Matsuo Hitomi Tsukahara Keita Noda Eiji Yahiro Bo Zhang Yoshinari Uehara Shin-ichiro Miura Keijiro Saku
- 出版者
- The Japanese Circulation Society
- 雑誌
- Circulation Journal (ISSN:13469843)
- 巻号頁・発行日
- vol.78, no.12, pp.2955-2962, 2014-11-25 (Released:2014-11-25)
- 参考文献数
- 47
- 被引用文献数
- 23 48
Background:Smoking cessation reduces the risk of cardiovascular disease (CVD) and improves clinical outcomes in public health. We studied the effect of smoking cessation on high-density lipoprotein (HDL) functionality.Methods and Results:We randomly treated 32 smokers with varenicline or a transdermal nicotine patch as part of a 12-week smoking cessation program (The VN-SEESAW Study). The plasma lipid profiles, plasma and HDL malondialdehyde (MDA) levels, HDL subfractions as analyzed by capillary isotachophoresis, cholesterol efflux capacity, and antiinflammatory activity of HDL were measured before and after the anti-smoking intervention. After smoking cessation, HDL-C, apoA-I levels and HDL subfractions were not significantly different from the respective baseline values. However, cholesterol efflux capacity and the HDL inflammatory index (HII) were significantly improved after smoking cessation. The changes in both parameters (%∆ cholesterol efflux capacity and ∆HII) were also significantly improved in the successful smoking cessation group compared with the unsuccessful group. The changes in cholesterol efflux capacity and HII also correlated with those in end-expiratory CO concentration and MDA in HDL, respectively.Conclusions:Our findings indicate that smoking cessation leads to improved HDL functionality, increased cholesterol efflux capacity and decreased HII, without changing HDL-C or apoA-I levels or HDL subfractions. This may be one of the mechanisms by which smoking cessation improves the risk of CVD. (Circ J 2014; 78: 2955–2962)
- 著者
- Tomohiro Hayashi Tomoya Yamashita Hikaru Watanabe Kenjiro Kami Naofumi Yoshida Tokiko Tabata Takuo Emoto Naoto Sasaki Taiji Mizoguchi Yasuhiro Irino Ryuji Toh Masakazu Shinohara Yuko Okada Wataru Ogawa Takuji Yamada Ken-ichi Hirata
- 出版者
- The Japanese Circulation Society
- 雑誌
- Circulation Journal (ISSN:13469843)
- 巻号頁・発行日
- vol.83, no.1, pp.182-192, 2018-12-25 (Released:2018-12-25)
- 参考文献数
- 44
- 被引用文献数
- 79
Background: Gut microbiome composition or circulating microbiome-related metabolites in patients with heart failure (HF) have not been investigated at different time points (i.e., in the decompensated (Decomp) and compensated (Comp) phases). Methods and Results: We prospectively enrolled 22 patients admitted for HF and 11 age-, sex-, and comorbidity-matched hospitalized control subjects without a history of HF. Gut flora and plasma microbiome-related metabolites were evaluated by amplicon sequencing of the bacterial 16S ribosomal RNA gene and capillary electrophoresis time-of-flight mass spectrometry, respectively. HF patients were evaluated in both the Decomp and Comp phases during hospitalization. The phylum Actinobacteria was enriched in HF patients compared with control subjects. At the genus level, Bifiodobacterium was abundant while Megamonas was depleted in HF patients. Meanwhile, plasma concentration of trimethylamine N-oxide (TMAO), a gut microbiome-derived metabolite, was increased in HF patients (Decomp HF vs. control, P=0.003; Comp HF vs. control, P=0.004). A correlation analysis revealed positive correlations between the abundance of the genus Escherichia/Shigella and levels of TMAO and indoxyl sulfate (IS, a microbe-dependent uremic toxin) in Comp HF (TMAO: r=0.62, P=0.002; IS: r=0.63, P=0.002). Escherichia/Shigella was more abundant in Decomp than in Comp HF (P=0.030). Conclusions: Our results suggest that gut microbiome composition and microbiome-related metabolites are altered in HF patients.
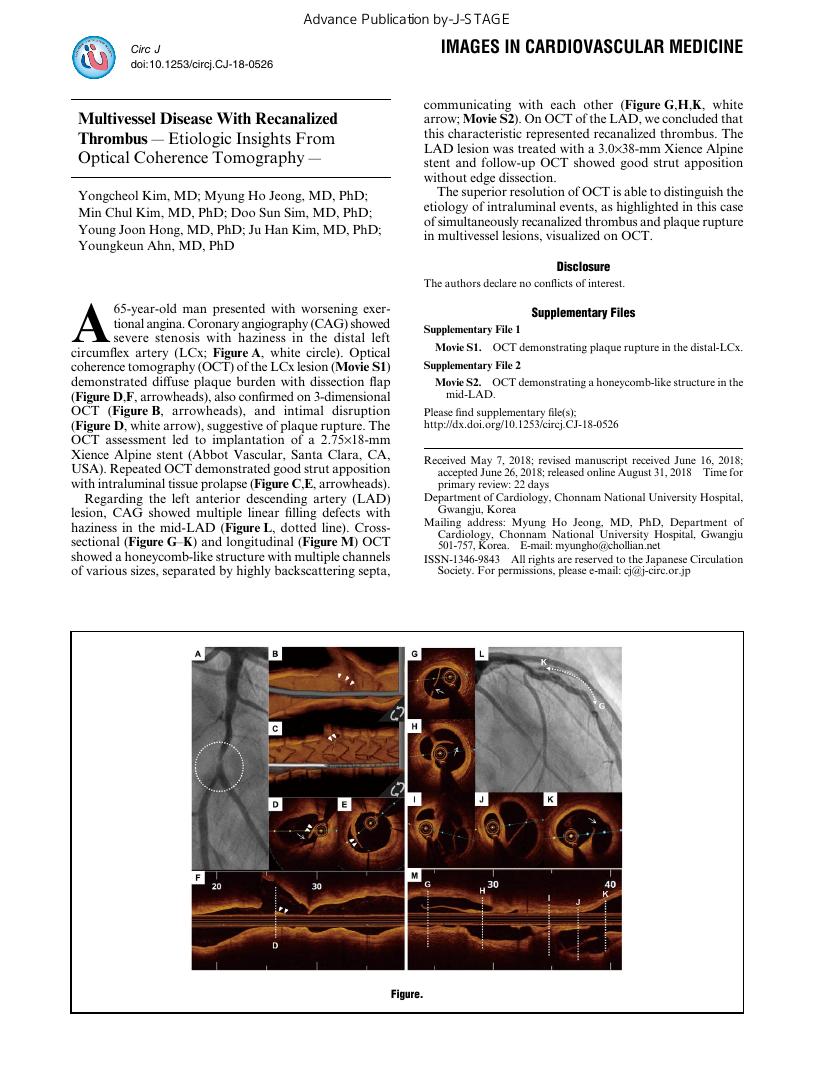
- 著者
- Yongcheol Kim Myung Ho Jeong Min Chul Kim Doo Sun Sim Young Joon Hong Ju Han Kim Youngkeun Ahn
- 出版者
- The Japanese Circulation Society
- 雑誌
- Circulation Journal (ISSN:13469843)
- 巻号頁・発行日
- pp.CJ-18-0526, (Released:2018-08-31)
- 著者
- Raisuke Iijima Rintaro Nakajima Kaoru Sugi Masato Nakamura
- 出版者
- The Japanese Circulation Society
- 雑誌
- Circulation Journal (ISSN:13469843)
- 巻号頁・発行日
- vol.71, no.7, pp.1079-1085, 2007 (Released:2007-06-25)
- 参考文献数
- 34
- 被引用文献数
- 7 7
Background Recent studies have shown that a global flow abnormality affects the entire coronary tree in patients with acute coronary syndrome (ACS), and that it is associated with adverse outcomes. Postprandial hyperglycemia is also thought to promote coronary endothelial dysfunction, as well as the release of inflammatory and vasoconstrictive factors. This study used the corrected Thrombolysis In Myocardial Infarction frame count (CTFC) to investigate whether optimal control of postprandial hyperglycemia improves pan-coronary flow. Methods and Results Eighty ACS patients with postprandial hyperglycemia who had successful coronary intervention and who had undergone a 75-g oral glucose tolerance test (OGTT) were included. A second OGTT and angiogram were performed 8 months after procedures. The patients were divided according to postprandial glycemia after the second 75-g OGTT; optimal postprandial hyperglycemia was defined as a 2-h blood glucose concentration <7.8 mmol/L. Changes in the CTFC of culprit/non-culprit arteries, glucose response, and other clinical variables were compared. Forty patients improved to an optimal control at 8 months. In the culprit artery, the 8-month angiogram revealed a significantly improved CTFC among those with optimal control compared with the initial angiogram (30±9 vs 24±12, p<0.05). In contrast, the CTFC was not evidently improved among patients with suboptimal control. The CTFC at 8 months had thus obviously improved more in patients with optimal, than with suboptimal control (24±12 vs 30±11, p<0.05). Conclusion Optimal control of postprandial hyperglycemia improves epicardial blood flow in both arteries and this beneficial effect might be from improved coronary endothelial function. (Circ J 2007; 71: 1079 - 1085)
- 著者
- Tetsuya Tatsumi Eishi Ashihara Toshihide Yasui Shinsaku Matsunaga Atsumichi Kido Yuji Sasada Satoshi Nishikawa Mitsuyoshi Hadase Masahiro Koide Reo Nakamura Hidekazu Irie Kazuki Ito Akihiro Matsui Hiroyuki Matsui Maki Katamura Shigehiro Kusuoka Satoaki Matoba Satoshi Okayama Manabu Horii Shiro Uemura Chihiro Shimazaki Hajime Tsuji Yoshihiko Saito Hiroaki Matsubara
- 出版者
- The Japanese Circulation Society
- 雑誌
- Circulation Journal (ISSN:13469843)
- 巻号頁・発行日
- vol.71, no.8, pp.1199-1207, 2007 (Released:2007-07-25)
- 参考文献数
- 40
- 被引用文献数
- 59 73
Background Transplantation of non-expanded peripheral blood mononuclear cells (PBMNCs) enhances neovessel formation in ischemic myocardium and limbs by releasing angiogenic factors. This study was designed to examine whether intracoronary transplantation of PBMNCs improves cardiac function after acute myocardial infarction (AMI). Methods and Results After successful percutaneous coronary intervention (PCI) for a ST-elevation AMI with occlusion of proximal left anterior descending coronary artery within 24 h, patients were assigned to either a control group or the PBMNC group that received intracoronary infusion of PBMNCs within 5 days after PCI. PBMNCs were obtained from patients by COBE spectra-apheresis and concentrated to 10 ml, 3.3 ml of which was infused via over-the-wire catheter. The primary endpoint was the global left ventricular ejection fraction (LVEF) change from baseline to 6 months' follow-up. The data showed that the absolute increase in LVEF was 7.4% in the control group and 13.4% (p=0.037 vs control) in the PBMNC group. Cell therapy resulted in a greater tendency of ΔRegional ejection fraction (EF) or significant improvement in the wall motion score index and Tc-99m-tetrofosmin perfusion defect score associated with the infarct area, compared with controls. Moreover, intracoronary administration of PBMNCs did not exacerbate either left ventricular (LV) end-diastolic and end-systolic volume expansion or high-risk arrhythmia, without any adverse clinical events. Conclusion Intracoronary infusion of non-expanded PBMNCs promotes improvement of LV systolic function. This less invasive and more feasible approach to collecting endothelial progenitor cells may provide a novel therapeutic option for improving cardiac function after AMI. (Circ J 2007; 71: 1199 - 1207)
- 著者
- Pawel Szulc Ez Zoubir Amri Annie Varennes Patricia Panaia-Ferrari Eric Fontas Joëlle Goudable Roland Chapurlat Véronique Breuil
- 出版者
- The Japanese Circulation Society
- 雑誌
- Circulation Journal (ISSN:13469843)
- 巻号頁・発行日
- vol.82, no.12, pp.2954-2961, 2018-11-24 (Released:2018-11-24)
- 参考文献数
- 42
- 被引用文献数
- 7
Background: Severe abdominal aortic calcification (AAC) points to high cardiovascular risk and leptin stimulates arterial calcification; however, clinical data on their association are scarce. We studied the link between serum leptin and AAC severity and progression, and the effect of smoking and lipid levels, on this association in men. Methods and Results: At baseline, 548 community-dwelling men aged 50–85 years underwent blood collection and lateral lumbar spine radiography. In 448 men, X-ray was repeated after 3 and 7.5 years. AAC was assessed using Kauppila’s semiquantitative score. In multivariable models, high leptin was associated with higher odds of severe AAC (odds ratio [OR]=1.71 per SD, 95% confidence interval [CI]: 1.22–2.40). The odds of severe AAC were the highest in men who had elevated leptin levels and either were ever-smokers (OR=9.22, 95% CI: 3.43–24.78) or had hypertriglyceridemia (vs. men without these characteristics). Higher leptin was associated with greater AAC progression (OR=1.34 per SD, 95% CI: 1.04–1.74). The risk of AAC progression was the highest in men who had elevated leptin levels and either were current smokers or had high low-density lipoprotein-cholesterol levels (OR=5.91, 95% CI: 2.46–14.16 vs. men without these characteristics). These links remained significant after adjustment for baseline AAC and in subgroups defined according to smoking and low-density lipoprotein-cholesterol levels. Conclusions: In older men, high leptin levels are associated with greater severity and rapid progression of AAC independent of smoking, low-density lipoprotein-cholesterol or triglycerides.
- 著者
- Yasutsugu Shiono Takashi Akasaka
- 出版者
- The Japanese Circulation Society
- 雑誌
- Circulation Journal (ISSN:13469843)
- 巻号頁・発行日
- pp.CJ-18-1056, (Released:2018-12-06)
- 参考文献数
- 13
- 著者
- Shinichi Nunoda
- 出版者
- The Japanese Circulation Society
- 雑誌
- Circulation Journal (ISSN:13469843)
- 巻号頁・発行日
- vol.82, no.12, pp.2943-2945, 2018-11-24 (Released:2018-11-24)
- 参考文献数
- 14
- 被引用文献数
- 2
1 0 0 0 OA Dementia and Cardiovascular Surgery
- 著者
- Akira Sezai
- 出版者
- The Japanese Circulation Society
- 雑誌
- Circulation Journal (ISSN:13469843)
- 巻号頁・発行日
- vol.82, no.12, pp.2939-2940, 2018-11-24 (Released:2018-11-24)
- 参考文献数
- 8
- 著者
- Mitsuyuki Nakayama Yasuhiro Asari
- 出版者
- The Japanese Circulation Society
- 雑誌
- Circulation Journal (ISSN:13469843)
- 巻号頁・発行日
- vol.72, no.8, pp.1385-1387, 2008 (Released:2008-07-25)
- 参考文献数
- 13
- 被引用文献数
- 4 5
Patients demonstrating critical limb ischemia with a long-distance occlusion of the major arteries are sometimes poor candidates for bypass surgery, because tandem occlusion complicates distal anastomoses and poor run-off causes early occlusion of bypass grafts. In order to resolve these problems, angiogenesis therapy was attempted by subcutaneous injection of granulocyte colony-stimulating factor either before or after peripheral bypass surgery in 2 cases. (Circ J 2008; 72: 1385 - 1387)
- 著者
- Toshinao Takahashi Toshio Nagai Masato Kanda Mei-Lan Liu Naomichi Kondo Atsuhiko T Naito Takehiko Ogura Haruaki Nakaya Jong-Kook Lee Issei Komuro Yoshio Kobayashi
- 出版者
- The Japanese Circulation Society
- 雑誌
- Circulation Journal (ISSN:13469843)
- 巻号頁・発行日
- vol.79, no.12, pp.2703-2712, 2015-11-25 (Released:2015-11-25)
- 参考文献数
- 42
- 被引用文献数
- 7 17
Background:Adipose tissue is one of the sources of mesenchymal stem cells, which have the potential to differentiate into various types of cells, including myocytes. Whether brown adipose tissue (BAT)-derived cells might differentiate into the cardiac pacemaking-conducting cells, and have the potential to regenerate the cardiac conduction system (CCS), is investigated in this study.Methods and Results:BAT was isolated from the interscapular area of mice and enzymatically digested before culture. Round or fusiform cells showed spontaneous beating at 4–7 days after culturing of BAT-derived cells. Reverse transcriptase-polymerase chain reaction analysis and immunocytochemical analysis revealed that BAT-derived cells expressed several cardiomyocytes, the CCS and pacemaker (PM) cell marker genes and proteins. Patch-clamp techniques revealed that spontaneous electrical activity and the shape of the action potential showed properties of cardiac PM cells. Next, a complete atrioventricular (AV) block was created in mice and green fluorescent protein-positive (GFP (+)) BAT-derived cells were injected intramyocardially around the AV node. At 1 week after transplantation, 50% of BAT-derived cells injected mice showed a sinus rhythm or a 2:1 AV block. Immunohistochemical analysis revealed that injected GFP (+) cells were engrafted and some GFP (+) cells co-expressed several cardiac PM cell marker proteins.Conclusions:BAT-derived cells differentiate into the CCS and PM-like cells in vitro and in vivo, and may become a useful cell source for arrhythmia therapy. (Circ J 2015; 79: 2703–2712)
- 著者
- Kyohei Marume Seiji Takashio Toshiyuki Nagai Kenichi Tsujita Yoshihiko Saito Tsutomu Yoshikawa Toshihisa Anzai
- 出版者
- The Japanese Circulation Society
- 雑誌
- Circulation Journal (ISSN:13469843)
- 巻号頁・発行日
- pp.CJ-18-0639, (Released:2018-11-09)
- 参考文献数
- 50
- 被引用文献数
- 24
Background:Statins might be associated with improved survival in patients with heart failure with preserved ejection fraction (HFpEF). The effect of statins in HFpEF without coronary artery disease (CAD), however, remains unclear.Methods and Results:From the JASPER registry, a multicenter, observational, prospective cohort with Japanese patients aged ≥20 years requiring hospitalization with acute HF and LVEF ≥50%, 414 patients without CAD were selected for outcome analysis. Based on prescription of statins at admission, we divided patients into the statin group (n=81) or no statin group (n=333). We followed them for 25 months. The association between statin use and primary (all-cause mortality) and secondary (non-cardiac death, cardiac death, or rehospitalization for HF) endpoints was assessed in the entire cohort and in a propensity score-matched cohort. In the propensity score-matched cohort, 3-year mortality was lower in the statin group (HR, 0.21; 95% CI: 0.06–0.72; P=0.014). The statin group had a significantly lower incidence of non-cardiac death (P=0.028) and rehospitalization for HF (P<0.001), but not cardiac death (P=0.593). The beneficial effect of statins on mortality did not have any significant interaction with cholesterol level or HF severity.Conclusions:Statin use has a beneficial effect on mortality in HFpEF without CAD. The present findings should be tested in an adequately powered randomized clinical trial.
- 著者
- Toshiyuki Niki Tetsuzo Wakatsuki Koji Yamaguchi Yoshio Taketani Hiroyasu Oeduka Kenya Kusunose Takayuki Ise Takashi Iwase Hirotsugu Yamada Takeshi Soeki Masataka Sata
- 出版者
- The Japanese Circulation Society
- 雑誌
- Circulation Journal (ISSN:13469843)
- 巻号頁・発行日
- vol.80, no.2, pp.450-460, 2016-01-25 (Released:2016-01-25)
- 参考文献数
- 53
- 被引用文献数
- 22 67
Background:The effects of eicosapentaenoic acid (EPA) on coronary artery disease have been previously reported; however, those of the addition of EPA to strong statins on coronary plaque components and local inflammatory cytokines are not known.Methods and Results:A total of 95 patients who had been treated with strong statin for at least 6 months were randomized into 2 groups: an EPA group (additional treatment with EPA at 1,800 mg/day, n=48) or a control group (no additional treatment, n=47), for 6 months. The tissue characteristics of target coronary plaque in each patient were analyzed using IB-IVUS before and after treatment. We also measured plasma levels of inflammatory cytokines sampled in the coronary sinus (CS) and peripheral vein.A significant reduction in lipid volume (18.5±1.3 to 15.0±1.5 mm3, P=0.007) and a significant increase in fibrous volume (22.9±0.8 to 25.6±1.1 mm3, P=0.01) were observed in IB-IVUS image analyses in the EPA group, but no significant changes in the plaque components in the control group. CS levels of pentraxin 3 and monocyte chemoattractant protein-1 were lower after than before treatment with EPA (3.3±2.1 to 2.6±1.2 ng/ml, 120.4±26.2 to 110.2±26.8 pg/ml, P=0.015 and P=0.008, respectively); however, there were no significant changes in those inflammatory cytokines between pre- and post-treatment in the control group.Conclusions:The addition of EPA was associated with reduced lipid volume in coronary plaques and decreased inflammatory cytokines. (Circ J 2016; 80: 450–460)