- 著者
- Madoka Sano Kitae Kim Yutaka Furukawa
- 出版者
- The Japanese Society of Internal Medicine
- 雑誌
- Internal Medicine (ISSN:09182918)
- 巻号頁・発行日
- pp.8826-21, (Released:2021-12-28)
- 参考文献数
- 3
- 著者
- Shigeru Makita Takanori Yasu Yoshihiro J Akashi Hitoshi Adachi Hideo Izawa Shunichi Ishihara Yoshitaka Iso Hideo Ohuchi Kazuto Omiya Yusuke Ohya Koichi Okita Yutaka Kimura Akira Koike Masahiro Kohzuki Shinji Koba Masataka Sata Kazunori Shimada Tomoki Shimokawa Hirokazu Shiraishi Naokata Sumitomo Tetsuya Takahashi Tomoyuki Takura Hiroyuki Tsutsui Masatoshi Nagayama Emiko Hasegawa Yoshihiro Fukumoto Yutaka Furukawa Shin-ichiro Miura Satoshi Yasuda Sumio Yamada Yuichiro Yamada Dai Yumino Toshiko Yoshida Takuji Adachi Toshimi Ikegame Kazuhiro P Izawa Takeshi Ishida Neiko Ozasa Naohiko Osada Hiroaki Obata Naoya Kakutani Yusuke Kasahara Masaaki Kato Kentaro Kamiya Shintaro Kinugawa Yuji Kono Yasuyuki Kobayashi Teruyuki Koyama Kazuhiro Sase Shinji Sato Tatsuhiro Shibata Norio Suzuki Daisuke Tamaki Minako Yamaoka-Tojo Michio Nakanishi Eisaku Nakane Mari Nishizaki Taiki Higo Kanta Fujimi Tasuku Honda Yasuharu Matsumoto Noriko Matsumoto Ikuko Miyawaki Makoto Murata Shusuke Yagi Masanobu Yanase Midori Yamada Miho Yokoyama Noboru Watanabe Haruki Ito Takeshi Kimura Syunei Kyo Yoichi Goto Ryuji Nohara Ken-Ichi Hirata on behalf of the Japanese Circulation Society/the Japanese Association of Cardiac Rehabilitation Joint Working Group
- 出版者
- The Japanese Circulation Society
- 雑誌
- Circulation Journal (ISSN:13469843)
- 巻号頁・発行日
- pp.CJ-22-0234, (Released:2022-12-09)
- 参考文献数
- 559
- 被引用文献数
- 67
- 著者
- Miho Nishitani-Yokoyama Hiroyuki Daida Kazunori Shimada Akiko Ushijima Keisuke Kida Yuji Kono Yasuhiko Sakata Masatoshi Nagayama Yutaka Furukawa Nagaharu Fukuma Keijiro Saku Shin-ichiro Miura Yusuke Ohya Youichi Goto Shigeru Makita for the Japanese Association of Cardiac Rehabilitation (JACR) Registration Committee
- 出版者
- The Japanese Circulation Society
- 雑誌
- Circulation Reports (ISSN:24340790)
- 巻号頁・発行日
- pp.CR-20-0087, (Released:2020-11-27)
- 参考文献数
- 25
- 被引用文献数
- 2
Background:Cardiac rehabilitation (CR) is categorized as a Class I recommendation in guidelines for the management of patients with acute coronary syndrome (ACS); however, nationwide studies on CR in patients with ACS remain limited in Japan.Methods and Results:The Japanese Association of Cardiac Rehabilitation (JACR) Registry is a nationwide, real-world database for patients participating in CR. From the JACR Registry database, we analyzed 924 patients participating in Phase II CR in 7 hospitals between September 2014 and December 2016. The mean age of patients was 65.9±12.0 years, and 80% were male. The prevalence of ST-elevation myocardial infarction (STEMI), non-STEMI (NSTEMI), and unstable angina pectoris (UAP) was 58%, 9%, and 33%, respectively. The prevalence of hypertension, diabetes, dyslipidemia, current smoking, and a family history was 55%, 27%, 67%, 21%, and 10%, respectively. Among the entire CR cohort at baseline, 96%, 78%, and 92% were treated with aspirin, β-blockers, and statins, respectively. After CR, the values of body mass index, the lipid profile, and exercise capacity significantly improved in the STEMI, NSTEMI and UAP groups.Conclusions:In the JACR Registry, a high rate of guideline-recommended medications at baseline and improvements in both coronary risk factors and exercise capacity after CR were observed in patients with ACS.
- 著者
- Tomotsugu Seki Makoto Murata Kensuke Takabayashi Takashi Yanagisawa Masayuki Ogihara Ritsuko Kurimoto Keisuke Kida Koichi Tamita Xiaoyang Song Neiko Ozasa Ryoji Taniguchi Miho Nishitani-Yokoyama Shinji Koba Ryosuke Murai Yutaka Furukawa Maki Hamasaki Hirokazu Kondo Hironori Hayashi Asako Ootakara-Katsume Kento Tateishi Satoaki Matoba Hitoshi Adachi Hirokazu Shiraishi for the START Investigators
- 出版者
- The Japanese Circulation Society
- 雑誌
- Circulation Reports (ISSN:24340790)
- 巻号頁・発行日
- vol.5, no.3, pp.90-94, 2023-03-10 (Released:2023-03-10)
- 参考文献数
- 18
Background: Clinical practice guidelines strongly recommend optimal medical therapy (OMT), including lifestyle modification, pharmacotherapy, and exercise-based cardiac rehabilitation (CR), in patients with stable ischemic heart disease (SIHD). However, the efficacy and safety of CR in patients with SIHD without revascularization remain unclear.Methods and Results: The Prospective Registry of STable Angina RehabiliTation (Pre-START) study is a multicenter, prospective, single-arm, open-label pilot study to evaluate the efficacy and safety of CR on health-related quality of life (HRQL), exercise capacity, and clinical outcomes in Japanese patients with SIHD without revascularization. In this study, all patients will undergo guideline-based OMT and are encouraged to have 36 outpatient CR sessions within 5 months after enrollment. The primary endpoint is the change in the Seattle Angina Questionnaire-7 summary score between baseline and the 6-month visit; an improvement of ≥5 points will be defined as a clinically important change. Secondary endpoints include changes in other HRQL scores and exercise capacity between baseline and the 6-month visit, as well as clinical outcomes between enrollment and the 6-month visit.Conclusions: The Pre-START study will provide valuable evidence to elucidate the efficacy and safety of CR in patients with SIHD and indispensable information for a subsequent randomized controlled trial. The study was registered with the University Hospital Medical Information Network (UMIN) Clinical Trials Registry (ID: UMIN000045415) on April 1, 2022.
- 著者
- Miho Nishitani-Yokoyama Hiroyuki Daida Kazunori Shimada Akiko Ushijima Keisuke Kida Yuji Kono Yasuhiko Sakata Masatoshi Nagayama Yutaka Furukawa Nagaharu Fukuma Keijiro Saku Shin-ichiro Miura Yusuke Ohya Youichi Goto Shigeru Makita for the Japanese Association of Cardiac Rehabilitation (JACR) Registration Committee
- 出版者
- The Japanese Circulation Society
- 雑誌
- Circulation Reports (ISSN:24340790)
- 巻号頁・発行日
- vol.2, no.12, pp.715-721, 2020-12-10 (Released:2020-12-10)
- 参考文献数
- 25
- 被引用文献数
- 2
Background:Cardiac rehabilitation (CR) is categorized as a Class I recommendation in guidelines for the management of patients with acute coronary syndrome (ACS); however, nationwide studies on CR in patients with ACS remain limited in Japan.Methods and Results:The Japanese Association of Cardiac Rehabilitation (JACR) Registry is a nationwide, real-world database for patients participating in CR. From the JACR Registry database, we analyzed 924 patients participating in Phase II CR in 7 hospitals between September 2014 and December 2016. The mean age of patients was 65.9±12.0 years, and 80% were male. The prevalence of ST-elevation myocardial infarction (STEMI), non-STEMI (NSTEMI), and unstable angina pectoris (UAP) was 58%, 9%, and 33%, respectively. The prevalence of hypertension, diabetes, dyslipidemia, current smoking, and a family history was 55%, 27%, 67%, 21%, and 10%, respectively. Among the entire CR cohort at baseline, 96%, 78%, and 92% were treated with aspirin, β-blockers, and statins, respectively. After CR, the values of body mass index, the lipid profile, and exercise capacity significantly improved in the STEMI, NSTEMI and UAP groups.Conclusions:In the JACR Registry, a high rate of guideline-recommended medications at baseline and improvements in both coronary risk factors and exercise capacity after CR were observed in patients with ACS.
- 著者
- Yasuaki Takeji Hiroki Shiomi Takeshi Morimoto Yutaka Furukawa Natsuhiko Ehara Yoshihisa Nakagawa Takao Kato Junichi Tazaki Eri Toda Kato Hidenori Yaku Yusuke Yoshikawa Tomohisa Tada Michiya Hanyu Kazushige Kadota Tatsuhiko Komiya Kenji Ando Takeshi Kimura CREDO-Kyoto PCI/CABG Registry Cohort Investigators
- 出版者
- The Japanese Circulation Society
- 雑誌
- Circulation Journal (ISSN:13469843)
- 巻号頁・発行日
- pp.CJ-19-0980, (Released:2020-01-29)
- 参考文献数
- 31
- 被引用文献数
- 7
Background:The effect of diabetes mellitus (DM) status on the long-term risk for heart failure (HF) in patients undergoing coronary revascularization has not been adequately evaluated.Methods and Results:In this study, 15,231 patients who underwent coronary revascularization in the CREDO-Kyoto Registry Cohort-2 were divided into 2 groups according to DM status (DM group: n=5,999; Non-DM group: n=9,232). The DM group was further divided into 2 groups according to insulin treatment (insulin-treated DM [ITDM]: n=1,353; non-insulin-treated DM [NITDM]: n=4,646). The primary outcome measure was HF hospitalization. The cumulative 5-year incidence of HF hospitalization was significantly higher in the DM than non-DM group (11.0% vs. 6.6%, respectively; log-rank P<0.0001), and in the ITDM than NITDM group (14.6% vs. 10.0%, respectively; log-rank P<0.0001). After adjusting for confounders, the increased risk of HF hospitalization with DM relative to non-DM remained significant (hazard ratio [HR] 1.47, 95% confidence interval [CI] 1.30–1.67, P<0.0001), whereas the risk associated with ITDM relative to NITDM was not significant (HR 1.17, 95% CI 0.96–1.43, P=0.12).Conclusions:The adjusted long-term risk for HF hospitalization after coronary revascularization was significantly higher in DM than non-DM patients, regardless of revascularization strategy, but did not differ between ITDM and NITDM patients.
- 著者
- Hisashi Kai Takeshi Kimura Kenji Fukuda Yoshihiro Fukumoto Tatsuyuki Kakuma Yutaka Furukawa on behalf of CREDO-Kyoto Investigators
- 出版者
- 日本循環器学会
- 雑誌
- Circulation Journal (ISSN:13469843)
- 巻号頁・発行日
- pp.CJ-15-1151, (Released:2016-04-06)
- 参考文献数
- 21
- 被引用文献数
- 9
Background:We investigated the effects of age and low diastolic blood pressure (DBP) on cardiovascular death in patients with coronary artery disease (CAD) after coronary revascularization.Methods and Results:Stable, chronic CAD patients after coronary revascularization in the CREDO-Kyoto registry cohort-1 were allocated to the Young (≤64 years, n=2,619), Young-Old (65–74 years, n=2,932), and Old-Old (≥75 years, n=1,629) groups. Kaplan-Meier analysis showed that the crude cumulative incidence of cardiovascular death was higher in Young-Old patients with DBP <70 mmHg (P<0.001) and in Old-Old patients with DBP <60 mmHg (P=0.017), but not <70 mmHg (P=0.629), compared with each counterpart. Low DBP did not increase cardiovascular death in young patients. After adjustments with independent predictors, DBP <60 mmHg did not increase the cardiovascular death in the Old-Old group (HR=1.579 [95% CI, 0.944–2.642], P=0.082) and DBP <70 mmHg remained a predictor in the Young-Old group (HR=1.665 [1.094–2.532], P=0.017). On multivariate stepwise Cox proportional hazard regression analysis, independent predictors for cardiovascular death in low DBP patients were creatinine clearance (CCr; inversely), prior cerebrovascular disease, and aortic disease in the Young-Old group and CCr (inversely) and malignancy in the Old-Old group.Conclusions:DBP <60 mmHg was not an independent factor for predicting cardiovascular death in Old-Old revascularized CAD patients, whereas DBP <70 mmHg remained a predictor in the Young-Old.
- 著者
- Tomohiko Taniguchi Yuhei Hasegawa Kitae Kim Natsuhiko Ehara Yutaka Furukawa
- 出版者
- The Japanese Circulation Society
- 雑誌
- Circulation Journal (ISSN:13469843)
- 巻号頁・発行日
- pp.CJ-23-0205, (Released:2023-05-24)
- 著者
- Atsushi Kobori Yasuhiro Sasaki Misun Pak Masahiro Ishikura Ryosuke Murai Taiji Okada Toshiaki Toyota Tomohiko Taniguchi Kitae Kim Natsuhiko Ehara Makoto Kinoshita Yasuki Kihara Yutaka Furukawa
- 出版者
- The Japanese Circulation Society
- 雑誌
- Circulation Journal (ISSN:13469843)
- 巻号頁・発行日
- vol.86, no.2, pp.290-298, 2022-01-25 (Released:2022-01-25)
- 参考文献数
- 27
- 被引用文献数
- 4
Background:Outcomes of cryoballoon ablation for persistent atrial fibrillation (AF) are unclear, especially in Japanese patients, so the effectiveness and safety of cryoballoon ablation in clinical practice were retrospectively compared with those of contact force-sensing radiofrequency (CFRF) ablation including the high-power protocol.Methods and Results:Consecutive patients with persistent AF were reviewed, and 253 and 265 patients who underwent cryoballoon and CFRF ablation, respectively, were enrolled. The primary endpoint was atrial arrhythmia recurrence. The secondary endpoints were periprocedural complications and repeat ablation. The rate of additional left atrial (LA) ablation after pulmonary vein isolation (PVI) was similar between groups (68.8% cryoballoon vs. 74.0% CFRF, P=0.19). Freedom from atrial arrhythmia recurrence was comparable between groups over a follow-up of 25.5±12.5 months (72.3% cryoballoon vs. 69.8% CFRF; adjusted hazard ratio (HR) 0.85, 95% confidence interval (CI) 0.59–1.21, P=0.36). Outcomes were similar in the subgroups of PVI alone and PVI plus additional LA ablation. LA posterior wall isolation, absence of defragmentation, and low creatine clearance, but not catheter selection, were associated with the primary endpoint. Periprocedural complications (adjusted HR 0.73, 95% CI 0.34–1.54, P=0.41) and repeat ablation (adjusted HR 1.11, 95% CI 0.71–1.74, P=0.64) were similar for both procedures.Conclusions:Cryoballoon ablation for persistent AF in Japanese clinical practice had acceptable outcomes comparable to those of advanced CFRF ablation.
- 著者
- Kenji Nakatsuma Hiroki Shiomi Takeshi Morimoto Yutaka Furukawa Yoshihisa Nakagawa Kenji Ando Kazushige Kadota Takashi Yamamoto Satoru Suwa Minoru Horie Takeshi Kimura on behalf of the CREDO-Kyoto AMI investigators
- 出版者
- 日本循環器学会
- 雑誌
- Circulation Journal (ISSN:13469843)
- 巻号頁・発行日
- pp.CJ-16-0204, (Released:2016-06-28)
- 参考文献数
- 24
- 被引用文献数
- 2 22
Background:Inter-facility transfer for primary percutaneous coronary intervention (PCI) from referring facilities to PCI centers causes a significant delay in treatment of ST-segment elevation acute myocardial infarction (STEMI) patients undergoing primary PCI. However, little is known about the clinical outcomes of STEMI patients undergoing inter-facility transfer in Japan.Methods and Results:In the CREDO-Kyoto acute myocardial infarction (AMI) registry that enrolled 5,429 consecutive AMI patients in 26 centers in Japan, the current study population consisted of 3,820 STEMI patients who underwent primary PCI within 24 h of symptom onset. We compared long-term clinical outcomes between inter-facility transfer patients and those directly admitted to PCI centers. The primary outcome measure was a composite of all-cause death or heart failure (HF) hospitalization. There were 1,725 (45.2%) inter-facility transfer patients, and 2,095 patients (54.8%) with direct admission to PCI centers. The cumulative 5-year incidence of death/HF hospitalization was significantly higher in the inter-facility transfer patients than in those with direct admission (26.9% vs. 22.2%; log-rank P<0.001). After adjusting for potential confounders, the risk for death/HF hospitalization was significantly higher (adjusted hazard ratio: 1.22, 95% confidence interval: 1.07–1.40, P<0.001) in the inter-facility transfer patients than in those directly admitted.Conclusions:Inter-facility transfer was associated with significantly worse long-term clinical outcomes for patients with STEMI undergoing primary PCI.
- 著者
- Kenji Nakatsuma Hiroki Shiomi Takeshi Morimoto Kenji Ando Kazushige Kadota Hiroki Watanabe Tomohiko Taniguchi Takashi Yamamoto Yutaka Furukawa Yoshihisa Nakagawa Minoru Horie Takeshi Kimura on behalf of the CREDO-Kyoto AMI investigators
- 出版者
- 日本循環器学会
- 雑誌
- Circulation Journal (ISSN:13469843)
- 巻号頁・発行日
- pp.CJ-15-0870, (Released:2015-12-15)
- 参考文献数
- 19
- 被引用文献数
- 2 32
Background:In the setting of elective percutaneous coronary intervention (PCI), intravascular ultrasound (IVUS)-guided PCI is associated with a reduction in the incidence of target vessel revascularization (TVR), but the impact of IVUS on long-term clinical outcome in the setting of emergency PCI for ST-segment elevation acute myocardial infarction (STEMI) is still unclear.Methods and Results:The subjects consisted of 3,028 STEMI patients who underwent primary PCI within 24 h of symptom onset in the CREDO-Kyoto acute myocardial infarction registry. Of these, 932 patients (31%) underwent IVUS-guided PCI. Compared with the angiography-guided PCI without IVUS, IVUS-guided PCI was associated with significantly lower incidences of TVR (primary outcome measure; 22% vs. 27%, log-rank P<0.001) and definite stent thrombosis (ST; 1.2% vs. 3.1%, log-rank P=0.003). The cumulative incidence of all-cause death was not significantly different between the 2 groups. After adjusting for confounders, however, there were no significant differences between the 2 groups in risk for TVR (adjusted HR, 1.14; 95% CI: 0.86–1.51, P=0.38) and definite ST (adjusted HR, 0.58; 95% CI: 0.19–1.72, P=0.33).Conclusions:IVUS-guided PCI was not associated with a lower risk for TVR or ST in STEMI patients undergoing primary PCI.
- 著者
- Tomotsugu Seki Makoto Murata Kensuke Takabayashi Takashi Yanagisawa Masayuki Ogihara Ritsuko Kurimoto Keisuke Kida Koichi Tamita Xiaoyang Song Neiko Ozasa Ryoji Taniguchi Miho Nishitani-Yokoyama Shinji Koba Ryosuke Murai Yutaka Furukawa Maki Hamasaki Hirokazu Kondo Hironori Hayashi Asako Ootakara-Katsume Kento Tateishi Satoaki Matoba Hitoshi Adachi Hirokazu Shiraishi for the START Investigators
- 出版者
- The Japanese Circulation Society
- 雑誌
- Circulation Reports (ISSN:24340790)
- 巻号頁・発行日
- pp.CR-22-0131, (Released:2023-02-25)
- 参考文献数
- 18
Background: Clinical practice guidelines strongly recommend optimal medical therapy (OMT), including lifestyle modification, pharmacotherapy, and exercise-based cardiac rehabilitation (CR), in patients with stable ischemic heart disease (SIHD). However, the efficacy and safety of CR in patients with SIHD without revascularization remain unclear.Methods and Results: The Prospective Registry of STable Angina RehabiliTation (Pre-START) study is a multicenter, prospective, single-arm, open-label pilot study to evaluate the efficacy and safety of CR on health-related quality of life (HRQL), exercise capacity, and clinical outcomes in Japanese patients with SIHD without revascularization. In this study, all patients will undergo guideline-based OMT and are encouraged to have 36 outpatient CR sessions within 5 months after enrollment. The primary endpoint is the change in the Seattle Angina Questionnaire-7 summary score between baseline and the 6-month visit; an improvement of ≥5 points will be defined as a clinically important change. Secondary endpoints include changes in other HRQL scores and exercise capacity between baseline and the 6-month visit, as well as clinical outcomes between enrollment and the 6-month visit.Conclusions: The Pre-START study will provide valuable evidence to elucidate the efficacy and safety of CR in patients with SIHD and indispensable information for a subsequent randomized controlled trial. The study was registered with the University Hospital Medical Information Network (UMIN) Clinical Trials Registry (ID: UMIN000045415) on April 1, 2022.
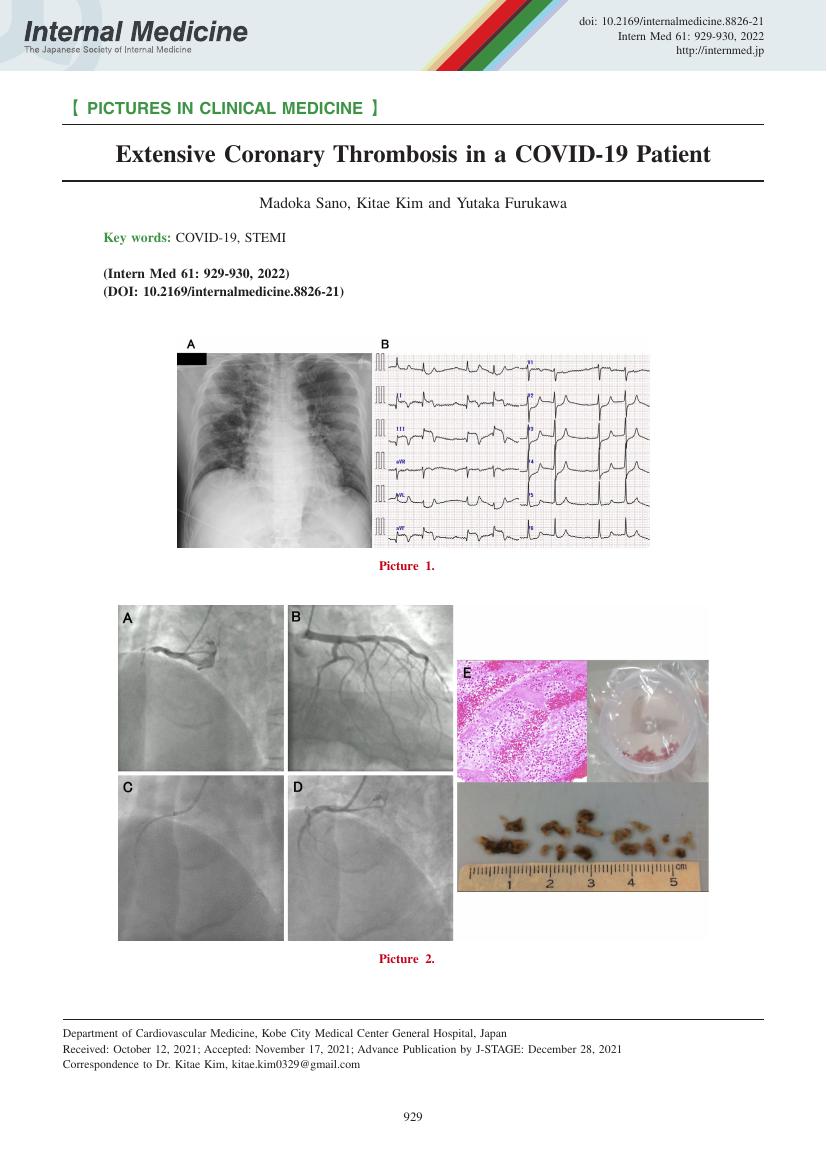
- 著者
- Madoka Sano Kitae Kim Yutaka Furukawa
- 出版者
- The Japanese Society of Internal Medicine
- 雑誌
- Internal Medicine (ISSN:09182918)
- 巻号頁・発行日
- vol.61, no.6, pp.929-930, 2022-03-15 (Released:2022-03-15)
- 参考文献数
- 3
- 著者
- Yuta Seko Takao Kato Takeshi Morimoto Hidenori Yaku Yasutaka Inuzuka Yodo Tamaki Neiko Ozasa Masayuki Shiba Erika Yamamoto Yusuke Yoshikawa Yugo Yamashita Takeshi Kitai Ryoji Taniguchi Moritake Iguchi Kazuya Nagao Takafumi Kawai Akihiro Komasa Ryusuke Nishikawa Yuichi Kawase Takashi Morinaga Mamoru Toyofuku Yutaka Furukawa Kenji Ando Kazushige Kadota Yukihito Sato Koichiro Kuwahara Takeshi Kimura for the KCHF Study Investigators
- 出版者
- The Japanese Circulation Society
- 雑誌
- Circulation Journal (ISSN:13469843)
- 巻号頁・発行日
- vol.86, no.10, pp.1547-1558, 2022-09-22 (Released:2022-09-22)
- 参考文献数
- 30
- 被引用文献数
- 3
Background: The clinical benefits of neurohormonal antagonists for patients with heart failure (HF) with mid-range and preserved ejection fraction (HFmrEF and HFpEF) are uncertain.Methods and Results: This study analyzed 858 consecutive patients with HFmrEF (EF: 40–49%) or HFpEF (EF ≥50%), who were hospitalized for acute HF, and who were discharged alive, and were not taking angiotensin-converting enzyme inhibitors (ACE)-I/ angiotensin II receptor blockers (ARB) or β-blockers at admission. The study population was classified into 4 groups according to the status of prescription of ACE-I/ARB and β-blocker at discharge: no neurohormonal antagonist (n=342, 39.9%), ACE-I/ARB only (n=128, 14.9%), β-blocker only (n=189, 22.0%), and both ACE-I/ARB and β-blocker (n=199, 23.2%) groups. The primary outcome measure was a composite of all-cause death or HF hospitalization. The cumulative 1-year incidence of the primary outcome measure was 41.2% in the no neurohormonal antagonist group, 34.0% in the ACE-I/ARB only group, 28.6% in the β-blocker only group, and 16.4% in the both ACE-I/ARB and β-blocker group (P<0.001). Compared with the no neurohormonal antagonist group, both the ACE-I/ARB and β-blocker groups were associated with a significantly lower risk for a composite of all-cause death or HF hospitalization (HR: 0.46, 95% CI: 0.28–0.76, P=0.002).Conclusions: In hospitalized patients with HFmrEF and HFpEF, starting both ACE-I/ARB and a β-blocker was associated with a reduced risk of the composite of all-cause death or HF hospitalization compared with patients not starting on an ACE-I/ARB or β-blocker.
- 著者
- Toshiaki Toyota Takeshi Morimoto Satoshi Iimuro Retsu Fujita Hiroshi Iwata Katsumi Miyauchi Teruo Inoue Yoshihisa Nakagawa Yosuke Nishihata Hiroyuki Daida Yukio Ozaki Satoru Suwa Ichiro Sakuma Yutaka Furukawa Hiroki Shiomi Hirotoshi Watanabe Kyohei Yamaji Naritatsu Saito Masahiro Natsuaki Yasuo Ohashi Masunori Matsuzaki Ryozo Nagai Takeshi Kimura
- 出版者
- The Japanese Circulation Society
- 雑誌
- Circulation Journal (ISSN:13469843)
- 巻号頁・発行日
- pp.CJ-22-0168, (Released:2022-09-14)
- 参考文献数
- 20
Background: The relationship between very low on-treatment low-density lipoprotein cholesterol (LDL-C) level and cardiovascular event risk is still unclear in patients receiving the same doses of statins.Methods and Results: From the REAL-CAD study comparing high-dose (4 mg/day) with low-dose (1 mg/day) pitavastatin therapy in patients with stable coronary artery disease, 11,105 patients with acceptable statin adherence were divided into 3 groups according to the on-treatment LDL-C level at 6 months (<70 mg/dL, 70–100 mg/dL, and ≥100 mg/dL). The primary outcome measure was a composite of cardiovascular death, non-fatal myocardial infarction, non-fatal ischemic stroke, or unstable angina requiring emergent admission. The adjusted risks of the LDL-C <70 mg/dL group relative to the LDL-C 70–100 mg/dL group (reference) was not significantly different for the primary outcome measure in both 1 mg/day and 4 mg/day strata (HR 0.84, 95% CI 0.58–1.18, P=0.32, and HR 1.25, 95% CI 0.88–1.79, P=0.22). The adjusted risk of the LDL-C ≥100 mg/dL group relative to the reference group was not significant for the primary outcome measure in the 1 mg/day stratum (HR 0.82, 95% CI 0.60–1.11, P=0.21), whereas it was highly significant in the 4 mg/day stratum (HR 3.32, 95% CI 2.08–5.17, P<0.001).Conclusions: A very low on-treatment LDL-C level (<70 mg/dL) was not associated with lower cardiovascular event risk compared with moderately low on-treatment LDL-C level (70–100 mg/dL) in patients receiving the same doses of statins.
- 著者
- Makoto Miyake Misa Takegami Yuki Obayashi Masashi Amano Takeshi Kitai Tomoyuki Fujita Tadaaki Koyama Hidekazu Tanaka Kenji Ando Tatsuhiko Komiya Masaki Izumo Hiroya Kawai Kiyoyuki Eishi Kiyoshi Yoshida Takeshi Kimura Ryuzo Nawada Tomohiro Sakamoto Yoshisato Shibata Toshihiro Fukui Kenji Minatoya Kenichi Tsujita Yasushi Sakata Tetsuya Kimura Kumiko Sugio Atsushi Takita Atsushi Iwakura Toshihiro Tamura Kunihiro Nishimura Yutaka Furukawa Chisato Izumi for the BPV-AF Registry Group
- 出版者
- The Japanese Circulation Society
- 雑誌
- Circulation Journal (ISSN:13469843)
- 巻号頁・発行日
- pp.CJ-22-0226, (Released:2022-07-08)
- 参考文献数
- 28
- 被引用文献数
- 2
Background: Current guidelines equally recommend direct oral anticoagulants (DOACs) and warfarin for atrial fibrillation (AF) patients with a bioprosthetic valve (BPV); however, there are limited data comparing DOACs and warfarin in AF patients with an aortic BPV.Methods and Results: This post-hoc subgroup analysis of a multicenter, prospective, observational registry (BPV-AF Registry) aimed to compare DOACs and warfarin in AF patients with an aortic BPV. The primary outcome was a composite of stroke, systemic embolism, major bleeding, heart failure requiring hospitalization, all-cause death, or BPV reoperation. The analysis included 479 patients (warfarin group, n=258; DOAC group, n=221). Surgical aortic valve replacement was performed in 74.4% and 36.7% of patients in the warfarin and DOAC groups, respectively. During a mean follow up of 15.5 months, the primary outcome occurred in 45 (17.4%) and 32 (14.5%) patients in the warfarin and DOAC groups, respectively. No significant difference was found in the primary outcome between the 2 groups (adjusted hazard ratio: 0.88, 95% confidence interval: 0.51–1.50). No significant multiplicative interaction was observed between the anticoagulant effects and type of aortic valve procedure (P=0.577).Conclusions: Among AF patients with an aortic BPV, no significant difference was observed in the composite outcome of adverse clinical events between patients treated with warfarin and those treated with DOACs, suggesting that DOACs can be used as alternatives to warfarin in these patients.
1 0 0 0 OA Concomitant Mitral Regurgitation in Severe Aortic Stenosis ― A Report From the CURRENT AS Registry ―
- 著者
- Ryosuke Murai Yuichi Kawase Tomohiko Taniguchi Takeshi Morimoto Kazushige Kadota Masanobu Ohya Takenobu Shimada Takeshi Maruo Yasushi Fuku Tatsuhiko Komiya Kenji Ando Michiya Hanyu Norio Kanamori Takeshi Aoyama Koichiro Murata Tomoya Onodera Fumio Yamazaki Takeshi Kitai Yutaka Furukawa Tadaaki Koyama Makoto Miyake Chisato Izumi Yoshihisa Nakagawa Kazuo Yamanaka Hirokazu Mitsuoka Manabu Shirotani Masashi Kato Shinji Miki Hiroyuki Nakajima Yutaka Hirano Shunichi Miyazaki Toshihiko Saga Sachiko Sugioka Shintaro Matsuda Mitsuo Matsuda Tatsuya Ogawa Kazuya Nagao Tsukasa Inada Shogo Nakayama Hiroshi Mabuchi Yasuyo Takeuchi Hiroki Sakamoto Genichi Sakaguchi Keiichiro Yamane Hiroshi Eizawa Mamoru Toyofuku Takashi Tamura Atsushi Iwakura Mitsuru Ishii Masaharu Akao Kotaro Shiraga Eri Minamino-Muta Takao Kato Moriaki Inoko Koji Ueyama Tomoyuki Ikeda Yoshihiro Himura Akihiro Komasa Katsuhisa Ishii Kozo Hotta Yukihito Sato Keiichi Fujiwara Yoshihiro Kato Ichiro Kouchi Yasutaka Inuzuka Shigeru Ikeguchi Senri Miwa Chiyo Maeda Eiji Shinoda Junichiro Nishizawa Toshikazu Jinnai Nobuya Higashitani Mitsuru Kitano Yuko Morikami Shouji Kitaguchi Kenji Minatoya Takeshi Kimura on behalf of the CURRENT AS Registry Investigators
- 出版者
- The Japanese Circulation Society
- 雑誌
- Circulation Journal (ISSN:13469843)
- 巻号頁・発行日
- vol.86, no.3, pp.427-437, 2022-02-25 (Released:2022-02-25)
- 参考文献数
- 26
- 被引用文献数
- 3
Background:The clinical significance of concomitant mitral regurgitation (MR) has not been well addressed in patients with severe aortic stenosis (AS).Methods and Results:We analyzed 3,815 patients from a retrospective multicenter registry of severe AS in Japan (CURRENT AS registry). We compared the clinical outcomes between patients with moderate/severe MR and with none/mild MR according to the initial treatment strategy (initial aortic valve replacement [AVR] or conservative strategy). The primary outcome measure was a composite of aortic valve-related death or heart failure hospitalization. At baseline, moderate/severe MR was present in 227/1,197 (19%) patients with initial AVR strategy and in 536/2,618 (20%) patients with a conservative strategy. The crude cumulative 5-year incidence of the primary outcome measure was significantly higher in patients with moderate/severe MR than in those with none/mild MR, regardless of the initial treatment strategy (25.2% vs. 14.4%, P<0.001 in the initial AVR strategy, and 63.3% vs. 40.7%, P<0.001 in the conservative strategy). After adjusting confounders, moderate/severe MR was not independently associated with higher risk for the primary outcome measure in the initial AVR strategy (hazard ratio [HR] 1.11, 95% confidence interval [CI] 0.67–1.83, P=0.69), and in the conservative strategy (HR 1.13, 95% CI 0.93–1.37, P=0.22).Conclusions:Concomitant moderate/severe MR was not independently associated with higher risk for the primary outcome measure regardless of the initial treatment strategy.
- 著者
- Masahiro Natsuaki Takeshi Morimoto Hiroki Shiomi Ko Yamamoto Kyohei Yamaji Hirotoshi Watanabe Takashi Uegaito Mitsuo Matsuda Toshihiro Tamura Ryoji Taniguchi Moriaki Inoko Hiroshi Mabuchi Teruki Takeda Takenori Domei Manabu Shirotani Natsuhiko Ehara Hiroshi Eizawa Katsuhisa Ishii Masaru Tanaka Tsukasa Inada Tomoya Onodera Ryuzo Nawada Eiji Shinoda Miho Yamada Takashi Yamamoto Hiroshi Sakai Mamoru Toyofuku Takashi Tamura Mamoru Takahashi Tomohisa Tada Hiroki Sakamoto Takeshi Tada Kazuhisa Kaneda Shinji Miki Takeshi Aoyama Satoru Suwa Yukihito Sato Kenji Ando Yutaka Furukawa Yoshihisa Nakagawa Kazushige Kadota Takeshi Kimura on behalf of the CREDO-Kyoto PCI/CABG Registry Cohort-Investigators
- 出版者
- The Japanese Circulation Society
- 雑誌
- Circulation Journal (ISSN:13469843)
- 巻号頁・発行日
- pp.CJ-21-0526, (Released:2021-09-16)
- 参考文献数
- 27
- 被引用文献数
- 1
Background:Optimal intensity is unclear for P2Y12receptor blocker therapy after percutaneous coronary intervention (PCI) in real-world clinical practice.Methods and Results:From the CREDO-Kyoto Registry, the current study population consisted of 25,419 patients (Cohort-2: n=12,161 and Cohort-3: n=13,258) who underwent their first PCI. P2Y12receptor blocker therapies were reduced dose of ticlopidine (200 mg/day), and global dose of clopidogrel (75 mg/day) in 87.7% and 94.8% of patients in Cohort-2 and Cohort-3, respectively. Cumulative 3-year incidence of GUSTO moderate/severe bleeding was significantly higher in Cohort-3 than in Cohort-2 (12.1% and 9.0%, P<0.0001). After adjusting 17 demographic factors and 9 management factors potentially related to the bleeding events other than the type of P2Y12receptor blocker, the higher bleeding risk in Cohort-3 relative to Cohort-2 remained significant (hazard ratio (HR): 1.52 95% confidence interval (CI) 1.37–1.68, P<0.0001). Cohort-3 compared with Cohort-2 was not associated with lower adjusted risk for myocardial infarction/ischemic stroke (HR: 0.96, 95% CI: 0.87–1.06, P=0.44).Conclusions:In this historical comparative study, Cohort-3 compared with Cohort-2 was associated with excess bleeding risk, which might be at least partly explained by the difference in P2Y12receptor blockers.
- 著者
- Atsuyoshi Kawagoshi Masahiro Iwakura Yutaka Furukawa Keiyu Sugawara Hitomi Takahashi Takanobu Shioya
- 出版者
- The Society of Physical Therapy Science
- 雑誌
- Journal of Physical Therapy Science (ISSN:09155287)
- 巻号頁・発行日
- vol.32, no.12, pp.804-809, 2020 (Released:2020-12-11)
- 参考文献数
- 30
- 被引用文献数
- 1
[Purpose] The effect of physical activity on systemic inflammation remains unclear and might be negative in patients with chronic obstructive pulmonary disease (COPD) and lower weight. We investigated the amount of physical activity as the time spent in posture and movement and its association with systemic inflammation. [Participants and Methods] In this retrospective cross-sectional pilot study, we evaluated 11 patients with COPD (age, 73 ± 7 years; body mass index, 18.9 ± 2.9 kg/m2). A recently developed triaxial accelerometer was used to measure the time spent in posture and movement. We also evaluated body composition, physiological indexes, and serum levels of inflammatory cytokines. Single correlation coefficients were calculated as the association between physical activity and other outcomes. [Results] The walking time was 36 ± 32 min/d, and the standing time was 151 ± 118 min/d. The time spent walking significantly correlated with the fat-free mass index (r=0.73) and interleukin (IL)-8 level (r=0.76). The time spent standing significantly correlated with the C-reactive protein (r=0.80) and IL-6 levels (r=0.74). [Conclusion] These data indicate that increased physical activity is associated with higher systematic inflammation. We should consider that the systemic inflammation may have been affected by the increased physical activity of the patients with COPD and lower weight in this study.
- 著者
- Mamoru Toyofuku Tomohiko Taniguchi Takeshi Morimoto Kyohei Yamaji Yutaka Furukawa Kosuke Takahashi Takashi Tamura Hiroki Shiomi Kenji Ando Norio Kanamori Koichiro Murata Takeshi Kitai Yuichi Kawase Chisato Izumi Makoto Miyake Hirokazu Mitsuoka Masashi Kato Yutaka Hirano Shintaro Matsuda Tsukasa Inada Tomoyuki Murakami Yasuyo Takeuchi Keiichiro Yamane Mitsuru Ishii Eri Minamino-Muta Takao Kato Moriaki Inoko Tomoyuki Ikeda Akihiro Komasa Katsuhisa Ishii Kozo Hotta Nobuya Higashitani Yoshihiro Kato Yasutaka Inuzuka Chiyo Maeda Toshikazu Jinnai Yuko Morikami Naritatsu Saito Kenji Minatoya Takeshi Kimura on behalf of the CURRENT AS Registry Investigators
- 出版者
- 日本循環器学会
- 雑誌
- Circulation Journal (ISSN:13469843)
- 巻号頁・発行日
- pp.CJ-16-1244, (Released:2017-04-08)
- 参考文献数
- 23
- 被引用文献数
- 34
Background:There is a paucity of data on the sex differences in the prevalence, clinical presentation, and prognosis of aortic stenosis (AS).Methods and Results:A total of 3,815 consecutive patients with severe AS were enrolled in the multicenter CURRENT AS registry between January 2003 and December 2011. The registry included 1,443 men (38%) and 2,372 women (62%). Women were much older than men (79±10 vs. 75±10 years, P<0.0001), and the ratio of women to men increased with age. The cumulative 5-year incidence of all-cause death was significantly higher in men than in women (47% vs. 41%, P=0.003), although women were more symptomatic and much older. The 5-year mortality was similar between men and women at age <65 years (16% vs. 15%, P=0.99), whereas it was significantly higher in men than in women at age ≥65 years (65–74 years, 38% vs. 19%, P<0.0001; 75–84 years, 55% vs. 34%, P<0.0001; ≥85 years: 82% vs. 72%, P=0.03).Conclusions:A large Japanese multicenter registry of consecutive patients with severe AS included a much higher proportion of women than men, with the female:male sex ratio increasing with age. The 5-year mortality rate of women was lower than that of men. Lower 5-year mortality rates in women were consistently seen across all age groups >65 years.