10 0 0 0 OA 尿中妊娠反応が陰性であった異所性妊娠破裂の1例
- 著者
- 水田 馨 三好 潤也 黒田 くみ子 井手上 隆史 田中 義弘 松岡 智史 吉松 かなえ 荒金 太
- 出版者
- 日本産科婦人科内視鏡学会
- 雑誌
- 日本産科婦人科内視鏡学会雑誌 (ISSN:18849938)
- 巻号頁・発行日
- vol.34, no.1, pp.123-127, 2018 (Released:2018-07-21)
- 参考文献数
- 19
Ectopic pregnancy is considered as a possible diagnosis in cases in which women experience acute abdominal pain and a urinary human chorionic gonadotropin (hCG) test produces a positive result. However, we present a case of ruptured ectopic pregnancy involving a negative urinary pregnancy test result. A 34-year-old nulliparous woman was admitted to the emergency room of our hospital due to the sudden onset of lower abdominal pain. Rebound pain in the lower abdomen was detected during a physical examination. Since transabdominal ultrasonography showed massive ascites, and a urinary pregnancy test produced a negative result, we performed a contrast-enhanced computed tomography scan and found a 5-cm right-sided ovarian cyst and extravasation around the left adnexa. We diagnosed the patient with left ovarian hemorrhaging and a right ovarian hemorrhagic luteal cyst. Two hours later, hemorrhagic shock occurred, and an emergency laparoscopic operation was carried out. We detected a swollen left fallopian tube, which had ruptured and was bleeding. We performed left salpingectomy. After the operation, the patient's preoperative serum sample was re-examined to re-assess her hCG level. As a result, her serum hCG level was found to be 23.3 mIU/ml. Pathological examinations showed a very small number of chorionic villi. The final diagnosis was ectopic pregnancy. The patient's postoperative course was uneventful. This case report illustrates the difficulty of diagnosing ectopic pregnancy. Clinicians should include ectopic pregnancy in the differential diagnoses for cases of acute abdominal pain involving women of reproductive age, regardless of the results of urinary pregnancy tests.
5 0 0 0 OA 腹腔内異物が疑われたヨード油性造影剤遺残の1例
- 著者
- 大橋 和明 小寺 宏平 伊藤 信一郎 原口 正史 入江 準二
- 出版者
- 日本産科婦人科内視鏡学会
- 雑誌
- 日本産科婦人科内視鏡学会雑誌 (ISSN:18849938)
- 巻号頁・発行日
- vol.32, no.1, pp.260-264, 2016 (Released:2017-01-21)
- 参考文献数
- 8
Lipiodized oil has been widely used for hysterosalpingography because it has superior imaging capability. We report a case of prolonged retention of lipiodized oil suspicious for foreign material in the abdomen. A 34-year-old woman who had undergone hysterosalpingography for evaluation of primary infertility visited our hospital with complaints of lower abdominal pain. She was found to have a metal-like shadow in the right side of the pelvis that was present on abdominal radiography performed at another facility. Computed tomography showed a high absorption range with halation in the right side of the pelvis. We suspected retention of metallic material because she had a history of cesarean section in our hospital several years prior, but we did not consider the likelihood of prolonged retention of lipiodized oil. Laparoscopic surgery was performed for diagnosis. During the operation we did not find any metallic material in the pelvis; we confirmed the position of the mass by using X-ray imaging and resected a cystic mass from the right side of the pelvis. The cyst showed high absorption on radiography and contained a yellowish oily fluid. We carried out a combustion experiment and it was found that the oily fluid included iodine; we therefore concluded that the cystic mass was due to prolonged retention of lipiodized oil rather than metallic material. It is necessary to consider the possibility of prolonged retention of lipiodized oil in patients with a history of hysterosalpingography.
- 著者
- 小田 日東美 田中 浩彦 秋山 登 徳山 智和 南 結 中野 讓子 小林 良成 井澤 美穂 朝倉 徹夫 谷口 晴記
- 出版者
- 日本産科婦人科内視鏡学会
- 雑誌
- 日本産科婦人科内視鏡学会雑誌 (ISSN:18849938)
- 巻号頁・発行日
- vol.33, no.1, pp.144-150, 2017 (Released:2017-06-06)
- 参考文献数
- 20
- 被引用文献数
- 1 1
Objective: Various developmental cysts arise in the retrorectal space because the 3 germ layers in this region are involved in fetal development. We encountered 2 patients with developmental cysts in the retrorectal space that were difficult to differentiate from an endometrial cyst before surgery; the cysts were laparoscopically diagnosed and treated. Patients: Both patients had a medical history in which an endometrial cyst was suspected; however, when the intra-abdominal cavity was examined, no abnormal finding was observed, and the abdomen was closed. In both patients, the presence of endometrial cysts measuring 7 cm on the right side of the rectum were suspected on preoperative magnetic resonance imaging. On laparoscopy, cysts were present in the right posterior region of the rectum in the retroperitoneal space and were excised. Pathological examination identified cystic hamartomas and epidermoid cysts. Conclusion: Complete excision is necessary because this lesion may lead to infection and conversion to malignancy. The procedure is performed in the deep extraperitoneal pelvic region, and requires corresponding knowledge and experience with gynecological malignancies; however, laparoscopic surgery may be feasible.
3 0 0 0 OA 妊娠中の子宮脱に対する新しい治療法
- 著者
- 横田 美幸 松元 隆 田坂 美恵 西 睦正 濱田 郁代
- 出版者
- 日本産科婦人科内視鏡学会
- 雑誌
- 日本産科婦人科内視鏡学会雑誌 (ISSN:18845746)
- 巻号頁・発行日
- vol.14, no.1, pp.109-111, 1998 (Released:2010-09-09)
- 参考文献数
- 11
2 0 0 0 OA 腹腔鏡下に処置できた腹膜妊娠の2例
- 著者
- 三浦 成陽 藤下 晃 濱崎 哲史 小寺 宏平 北島 道夫 今村 健仁 増崎 英明 石丸 忠之
- 出版者
- JAPAN SOCIETY OF GYNECOLOGIC AND OBSTETRIC ENDOSCOPY AND MINIMALLY INVASIVE THERAPY
- 雑誌
- 日本産科婦人科内視鏡学会雑誌 (ISSN:18845746)
- 巻号頁・発行日
- vol.20, no.2, pp.133-136, 2004 (Released:2010-09-09)
- 参考文献数
- 19
- 著者
- 山本 さやか 堀澤 信 品川 真奈花 今井 宗 羽田 智則
- 出版者
- 日本産科婦人科内視鏡学会
- 雑誌
- 日本産科婦人科内視鏡学会雑誌 (ISSN:18849938)
- 巻号頁・発行日
- vol.36, no.2, pp.348-357, 2020 (Released:2021-02-02)
- 参考文献数
- 14
Introduction: A discussion that uses surgical videos in a real conference room is called a Video Conference (VC) in Japan. Although VC is a useful tool in the education of laparoscopic surgery, it is difficult to hold VCs frequently between some facilities. An Online Surgical Video Discussion (OSVD) is the idea of holding VCs through the internet. We launched OSVDs in 2017 and report on the efficacy thereof.Methods: OSVD is approved by Institutional Review Board of Nagano Red Cross Hospital. OSVDs are held via You Tube™ Live. We conducted a questionnaire to investigate the perceived efficacy of OSVD.Results: We performed OSVDs 22 times from September 2017 to November 2019. There were 27 participants that completed the questionnaire. More than 70% of them thought that they had become more motivated, their frequency of watching surgical videos had increased, and OSVD was a good opportunity to learn from other facilities. All of the participants answered that OSVD would improve their surgical skills. In addition, more certified doctors participated in OSVDs than in VCs (OSVD 38.8%; VC 12.0%).Discussion: OSVD provides a valuable opportunity for furthering laparoscopic surgery education. Participants can discuss surgical videos without actually getting together physically, for free, and without any conflict of interest. Moreover, OSVDs may contribute to reducing disparities in laparoscopic surgery between regions and facilities, and thereby lead to a standardization of surgical skills.
- 著者
- 安藤 有里子 大西 賢人 緒方 佑莉 郷田 朋子 諸宇 ヒブン 中西 美紗緒 定月 みゆき 大石 元
- 出版者
- 日本産科婦人科内視鏡学会
- 雑誌
- 日本産科婦人科内視鏡学会雑誌 (ISSN:18849938)
- 巻号頁・発行日
- vol.35, no.2, pp.377-382, 2019
<p> Omental pregnancy is a subtype of abdominal pregnancy, which accounts for <1% of all ectopic pregnancies. Definitive diagnosis is challenging due to its rarity and difficulty in localizing its implantation site. Here, we describe the case of a 20-year-old nulliparous woman with omental pregnancy, referred to our hospital due to acute abdominal pain and high serum human chorionic gonadotropin levels. The gestational sac was not detected on a pelvic ultrasound examination. Abdominal contrast enhanced computerized tomography (CT) revealed an intra-abdominal hemorrhage and a 3-cm mass in the omentum. Diagnostic laparoscopy confirmed the omentum as the implantation site, following which complete resection of the lesion was performed. Histopathological analysis confirmed the diagnosis of omental pregnancy. Her postoperative course was uneventful. Our findings suggest that CT and laparoscopy are useful when the implantation site could not be visualized via ultrasonography in ectopic pregnancy. In addition, we discuss the association between emergency contraception and ectopic pregnancies.</p><p></p>
2 0 0 0 OA 腹腔鏡下人工造腟術―S状結腸利用法―
- 著者
- 伊熊 健一郎 子安 保喜 山田 幸生 林 輝美 脇本 栄子
- 出版者
- 日本産科婦人科内視鏡学会
- 雑誌
- 日本産科婦人科内視鏡学会雑誌 (ISSN:18845746)
- 巻号頁・発行日
- vol.12, no.1, pp.87-91, 1996 (Released:2010-09-09)
- 参考文献数
- 10
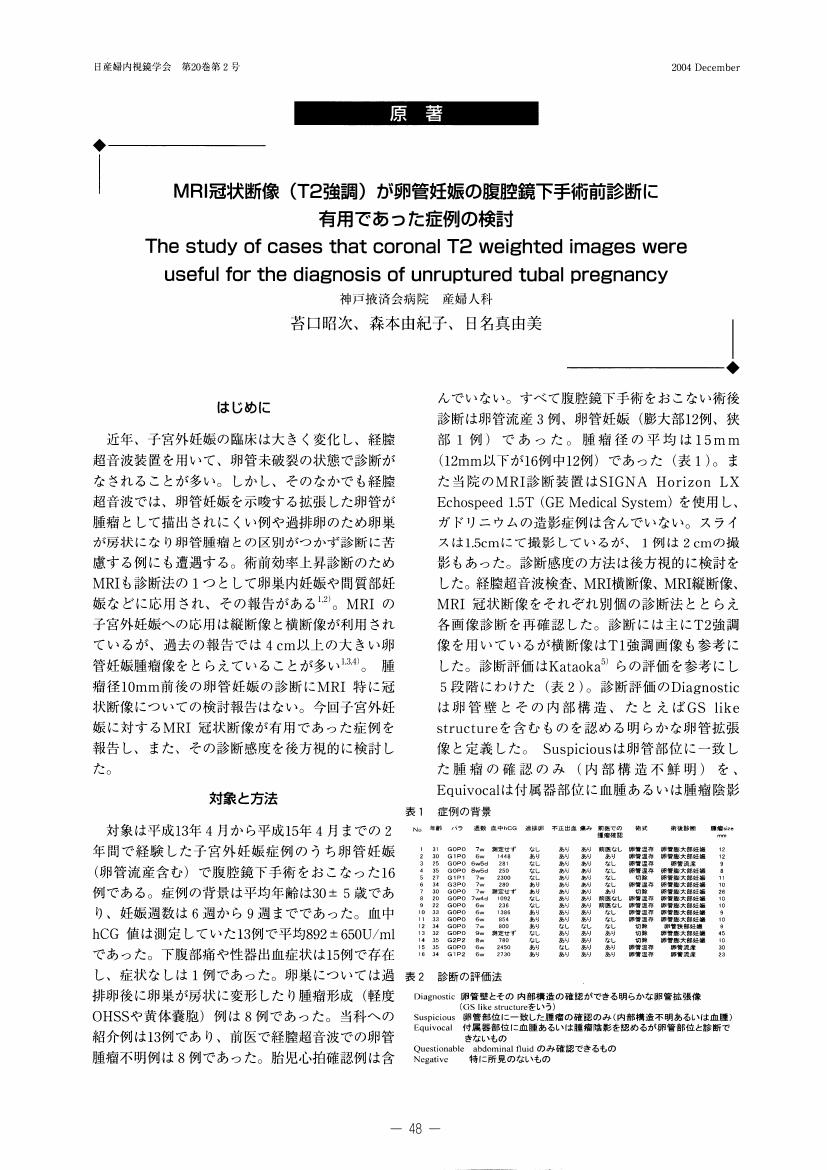
1 0 0 0 OA MRI冠状断像 (T2強調) が卵管妊娠の腹腔鏡下手術前診断に有用であった症例の検討
- 著者
- 苔口 昭次 森本 由紀子 日名 真由美
- 出版者
- JAPAN SOCIETY OF GYNECOLOGIC AND OBSTETRIC ENDOSCOPY AND MINIMALLY INVASIVE THERAPY
- 雑誌
- 日本産科婦人科内視鏡学会雑誌 (ISSN:18845746)
- 巻号頁・発行日
- vol.20, no.2, pp.48-52, 2004 (Released:2010-09-09)
- 参考文献数
- 15
1 0 0 0 OA 不妊患者における多嚢胞性卵巣症候群に対する腹腔鏡下卵巣多孔術後の治療成績
- 著者
- 青木 卓哉 中村 公彦 成本 勝彦 刈谷 方俊 壺井 和彦
- 出版者
- Japan Society of Gynecologic and Obstetric Endoscopy and Minimally Invasive Therapy
- 雑誌
- 日本産科婦人科内視鏡学会雑誌 (ISSN:18849938)
- 巻号頁・発行日
- vol.25, no.2, pp.379-384, 2009 (Released:2010-11-11)
- 参考文献数
- 19
- 被引用文献数
- 1 1
Objective: The aim of this study was to evaluate the ovulatory performance and reproductive outcome after laparoscopic ovarian drilling using a harmonic scalpel in infertile women with clomiphene-resistant polycystic ovarian syndrome (PCOS).Patients: Twenty clomiphene-resistant anovulatery women with PCOS underwent laparoscopic ovarian drilling between March 2005 and December 2006.Results: After surgery, LH serum levels and the LH/FSH ratio showed statistically significant reductions, and ovulation occurred spontaneously in 70% (14/20) of the patients. The pregnancy rate was 50% (10/20) in < 1 year. Within 4 months postoperatively, 50% of all pregnancies had occurred.Conclusion: Laparoscopic ovarian drilling is an effective treatment in women with clomiphene-resistant polycystic ovarian syndrome, yet without major complications associated with medical treatment, such as ovarian hyperstimulation syndrome and, plural gestations.
- 著者
- 永井 富裕子 青井 裕美 國見 聡子 河村 彩 山田 敦子 小泉 朱里 山口 貴史 須賀 新 糸賀 知子 西岡 暢子
- 出版者
- 日本産科婦人科内視鏡学会
- 雑誌
- 日本産科婦人科内視鏡学会雑誌 (ISSN:18849938)
- 巻号頁・発行日
- vol.29, no.2, pp.525-528, 2013 (Released:2014-06-16)
- 参考文献数
- 11
Atypical polypoid adenomyoma (APAM) is an endometrial tumor that arises from the uterine corpus or cervix in premenopausal woman. Although APAM is pathologically benign, it should be distinguished from atypical endometrial hyperplasia and complex invasive endometrial adenocarcinoma (G1) because these conditions are similar and often coexist. We report a patient with APAM treated with hysteroscopic transcervical resection (TCR). The 28-year-old nullipara patient had hypermenorrhea for 1 year and genital bleeding for 3 months. Ultrasound and MRI revealed a 27 mm×12 mm tumor in the uterine cavity, which was considered to be an endometrial polyp or submucosal myoma. TCR was performed after GnRHa administration for 3 months. Pathological diagnosis showed APAM. Dilatation and curettage was performed 1 month after surgery, showing several residual atypical glands of APAM. The patient was followed every 3 months, and no recurrence of APAM has been detected for 1.5 years. Although clinical management of APAM has not been established, TCR is a reliable procedure for conservative treatment under careful follow-up.
1 0 0 0 28.子宮頚部, 内膜のエンドマクロ, エンドミクロスコピー所見
- 著者
- 大川 公康 大川 了〓
- 出版者
- JAPAN SOCIETY OF GYNECOLOGIC AND OBSTETRIC ENDOSCOPY AND MINIMALLY INVASIVE THERAPY
- 雑誌
- 日本産科婦人科内視鏡学会雑誌 (ISSN:18849938)
- 巻号頁・発行日
- vol.2, no.1, pp.44-44, 1987
1 0 0 0 OA 腹腔鏡下子宮筋腫核出術後に下肢コンパートメント症候群を生じた1例
- 著者
- 山本 勢津子 楳木 美智子 新田 愼 荒金 太
- 出版者
- 日本産科婦人科内視鏡学会
- 雑誌
- 日本産科婦人科内視鏡学会雑誌 (ISSN:18849938)
- 巻号頁・発行日
- vol.35, no.1, pp.199-205, 2019 (Released:2019-06-08)
- 参考文献数
- 32
Well leg compartment syndrome (WLCS) is a rare but potentially devastating complication that is seen after gynecological, urological, and colorectal operations. We report a case of a 31-year-old woman presenting with right lower limb WLCS after laparoscopic myomectomy. The operation was performed in the lithotomy position combined with the Levitator and Trendelenburg positions and the duration of the procedure was approximately 6 hours. Both legs were attached with elastic stockings and intermittent pneumatic compression applied for prevention of deep vein thrombosis.Hemodynamic parameters of the patient were stable during the procedure. The Trendelenburg position was suspended, with the aim of preventing WLCS, for 5 minutes and 50 minutes at about 3 hours and 4 hours, respectively, from the beginning of the operation. Immediately after the operation, the patient complained of right crural pain, yet serum creatine phosphokinase (CPK) was detected to be within the normal range (100 IU/L). The following morning, on examination, we observed foot drop, paresthesia, swelling of the right calf, and an increased CPK (5316 IU/L). Three-dimensional computed tomography (3D CT) revealed the right lower limb muscle to be swollen and edematous in the posterior compartment. Acute arterial occlusion or deep vein thrombosis was not found. Fortunately, the patient did not need to undergo fasciotomy as the foot drop recovered after 3 months. WLCS is believed to be a life-threatening iatrogenic complication following surgery in the lithotomy position. As a result of this clinical experience, we have decided not to use elastic stockings, to mobilize the legs every 2 hours, and to take the supine position without Trendelenburg for 10 minutes at 3.5 hours from the beginning of the operation in this position. Moreover, to prevent irreversible damage, 3D CT angiography should not be delayed if WLCS is clinically suspected even in cases in which CPK is within the normal range.
- 著者
- 笠原 佑太 上田 和 上井 美里 横溝 陵 齋藤 良介 白石 絵莉子 駒崎 裕美 岡本 愛光
- 出版者
- 日本産科婦人科内視鏡学会
- 雑誌
- 日本産科婦人科内視鏡学会雑誌 (ISSN:18849938)
- 巻号頁・発行日
- vol.35, no.1, pp.158-162, 2019
<p><b>Introduction:</b> Heterotopic pregnancies are rare, with an incidence of approximately 0.003% in a natural ovulation cycle. We report a case of combined ovarian and intrauterine pregnancies, in which laparoscopic surgery confirmed the diagnosis and enabled successful pregnancy.</p><p><b>Case Report:</b> A 31-year-old nulliparous primigravida had received ovulation-inducing treatment, and pregnancy was successful. At 5 weeks of gestation, one gestational sac was found in the uterus, but at 6 weeks of gestation, a gestational-sac-like structure was found in the right adnexa, and the patient was referred to our hospital. Upon admission, her serum hCG level was 76,303 mIU/mL, and transvaginal ultrasonography revealed the presence of a gestational sac inside the uterus, a gestational-sac-like structure in contact with the right adnexa, and an echo-free space around the uterus. As intraperitoneal bleeding and heterotopic pregnancy were suspected, the risks and benefits of general anesthesia and laparoscopic surgery were explained to the patient, and an emergency laparoscopic surgery was performed.</p><p> Her intraoperative findings revealed intraperitoneal bleeding and enlargement of the right adnexa, with a 9.3-cm gestational sac adhered to the surface. A diagnosis of ovarian pregnancy with concomitant intrauterine pregnancy was confirmed, and the gestational sac on the right adnexa was removed. The postoperative course was uneventful.</p><p> A spontaneous vaginal delivery occurred at 39 weeks of gestation and resulted in a live birth.</p><p><b>Conclusions:</b> We report a case of combined ovarian and intrauterine pregnancies. Pregnancy can be adequately continued with appropriate diagnosis and treatment, and laparoscopic surgery may be a useful treatment option.</p><p></p>
1 0 0 0 OA 腹腔鏡下修復術を行った帝王切開瘢痕症候群の1例
- 著者
- 安岡 稔晃 藤岡 徹 上野 愛実 村上 祥子 井上 彩 内倉 友香 高木 香津子 宇佐美 知香 森 美妃 田中 寛希 松元 隆 松原 裕子 濱田 雄行 松原 圭一 杉山 隆
- 出版者
- 日本産科婦人科内視鏡学会
- 雑誌
- 日本産科婦人科内視鏡学会雑誌 (ISSN:18849938)
- 巻号頁・発行日
- vol.33, no.1, pp.121-125, 2017 (Released:2017-06-06)
- 参考文献数
- 9
BACKGROUND: With the increase in the cesarean section rate, the complications associated with cesarean section wounds have also increased. The presence of a cesarean scar defect and diverticulum has recently been identified as a source of persistent, irregular vaginal bleeding, menstrual pain, secondary infertility, and lower abdominal pain, known as cesarean scar syndrome. CASE: A 33-year-old woman presented with menstrual and lower abdominal pain in association with an anterior extrauterine cystic mass detected by pelvic ultrasound, thought to represent a cesarean scar diverticulum. The cystic diverticulum was laparoscopically excised, and the lower anterior uterine wall was repaired. The postoperative course was good and the patient was discharged on the fifth day after surgery. Menstrual and lower abdominal pain resolved after surgery. CONCLUSION: In cases of cesarean scar syndrome associated with a cystic diverticulum, laparoscopic surgery should be considered, especially when menstrual and lower abdominal pain is present.
1 0 0 0 OA 腹腔鏡下性腺摘出術を施行した性分化疾患の3例
- 著者
- 厚井 知穂 栗田 智子 庄 とも子 荒牧 聡 稲垣 博英 柴田 英治 蜂須賀 徹
- 出版者
- 日本産科婦人科内視鏡学会
- 雑誌
- 日本産科婦人科内視鏡学会雑誌 (ISSN:18849938)
- 巻号頁・発行日
- vol.29, no.2, pp.508-513, 2013 (Released:2014-06-16)
- 参考文献数
- 13
Disorders of sex development (DSD) are defined as congenital conditions in which development of chromosomal, gonadal, or anatomic sex is atypical. In some cases of DSD, especially 46,XY DSD and Turner syndrome (+Y), early bilateral gonadectomy is recommended; this recommendation is based upon the high incidence of gonadal tumors in affected individuals. Because these cases are frequently found in younger women, laparoscopic surgery is an excellent choice for minimally invasive treatment. We performed a prophylactic laparoscopic gonadectomy on three patients at the appropriate time after carefully determining the correct diagnosis.
- 著者
- 西澤 庸子 馬場 敦志 山下 剛
- 出版者
- 日本産科婦人科内視鏡学会
- 雑誌
- 日本産科婦人科内視鏡学会雑誌 (ISSN:18849938)
- 巻号頁・発行日
- vol.33, no.1, pp.209-213, 2017 (Released:2017-06-06)
- 参考文献数
- 24
Chylous ascites due to lymphorrhea is one of the complications following abdominal oncologic surgery. Chylous ascites requires long-term treatment and leads to a delay in additional treatment. We tried to detect and prevent chylous ascites. A 46-year-old woman with endometrial cancer and ovarian cancer underwent laparoscopic pelvic lymph node dissection and para-aortic lymph node (b1) dissection. She was fed milk as a high-fat diet 3 hours before the surgery. We could successfully detected chyle leakage after b1 dissection and performed clipping.
1 0 0 0 OA 卵巣成熟嚢胞性奇形種再発症例についての検討
- 著者
- 大熊 優子 西山 紘子 塚田 ひとみ 河西 明代 小野寺 成実 弟子丸 亮太 岸 郁子
- 出版者
- 日本産科婦人科内視鏡学会
- 雑誌
- 日本産科婦人科内視鏡学会雑誌 (ISSN:18849938)
- 巻号頁・発行日
- vol.35, no.2, pp.205-208, 2019 (Released:2020-01-07)
- 参考文献数
- 14
Objective: The objective of this study was to assess the risk of recurrence of ovarian mature cystic teratoma (OMCT) and to evaluate the feasibility of ovarian-conserving surgery.Methods: This retrospective clinical study investigated patients with OMCT who underwent laparoscopic surgery between January 2014 and March 2017.Results: Recurrence of OMCT was observed in 7 of 81 patients (8.6 %)—three patients (3.7%) showed ipsilateral recurrence, and four patients (4.9 %) showed recurrence in the contralateral ovary. Patients with recurrence (mean age 22.5 years [range 15–30 years]) were younger than those without recurrence (mean age 33.5 years [range 16–63 years]). No significant intergroup differences were observed in gravidity, parity, cyst size, intraoperative cyst rupture (cysts that did or did not rupture), number of cysts, and laterality. Conclusion: The recurrence tendency of OMCT in adolescents and in patients in their early 20s was higher than that in older patients. Cystectomy should be considered in children and patients of reproductive age for conservation of the affected ovary. An initial adnexectomy may not obviate the risk of multiple subsequent surgeries because OMCT may recur in the contralateral ovary.
1 0 0 0 OA 肥満症例における腹腔鏡手術
- 著者
- 高島 明子 大高 究 斉藤 麻由美 石田 洋昭 安田 豊 川島 秀明 斉藤 智博 深谷 暁 矢野 ともね 木下 俊彦
- 出版者
- JAPAN SOCIETY OF GYNECOLOGIC AND OBSTETRIC ENDOSCOPY AND MINIMALLY INVASIVE THERAPY
- 雑誌
- 日本産科婦人科内視鏡学会雑誌 (ISSN:18845746)
- 巻号頁・発行日
- vol.23, no.1, pp.218-220, 2007 (Released:2010-09-09)
- 参考文献数
- 11
1 0 0 0 習慣性流産におけるヒステロスコープ検査の意義
- 著者
- 佐藤 孝道 塩田 恭子 堀口 雅子 木村 宗昭 曽 栄輝 児島 孝久 島 由美子 安田 摂子 宇野 かおる 高橋 敬一
- 出版者
- 日本産科婦人科内視鏡学会
- 雑誌
- 日本産科婦人科内視鏡学会雑誌 (ISSN:18849938)
- 巻号頁・発行日
- vol.5, no.1, pp.44-46, 1989