- 著者
- 原周 一郎 別宮 若菜 松川 淳 佐々木 恵子 益子 尚子 関川 佳奈 佐藤 美和 齋藤 裕 浅田 弘法
- 出版者
- 日本産科婦人科内視鏡学会
- 雑誌
- 日本産科婦人科内視鏡学会雑誌 (ISSN:18849938)
- 巻号頁・発行日
- vol.35, no.1, pp.103-107, 2019
<p><b>Introduction:</b> Myomas are a common disorder in women of reproductive age, affecting 20%–50% of the population. The relationship between myomas and infertility is still unclear, and the effect of myomectomy on reproductive outcomes is uncertain. We retrospectively investigated patients with infertility who had laparoscopic myomectomy (LM) in our hospital and discussed the impact of LM on reproductive outcomes.</p><p><b>Methods:</b> A total of 54 patients with infertility who underwent LM in our hospital between January 2015 and September 2016 were analyzed. All patients received both preoperative and postoperative treatments for infertility, such as timed intercourse, intrauterine insemination (IUI), and assisted reproductive technology (ART).</p><p><b>Results:</b> Mean age was 37.0 (29–44, median 39) years. Of 54 patients, 34 (63.0%) conceived after LM (timed intercourse = 10, IUI = 1, and ART = 23). Mean duration between the operation and pregnancy was 9.2 (4–24, median 8.5) months. Uterine cavity distortion did not have an influence on reproductive outcomes. All pregnant women delivered by cesarean section. No uterine rupture was observed.</p><p><b>Conclusion:</b> LM may be offered to patients who do not become pregnant after infertility treatment.</p><p></p>
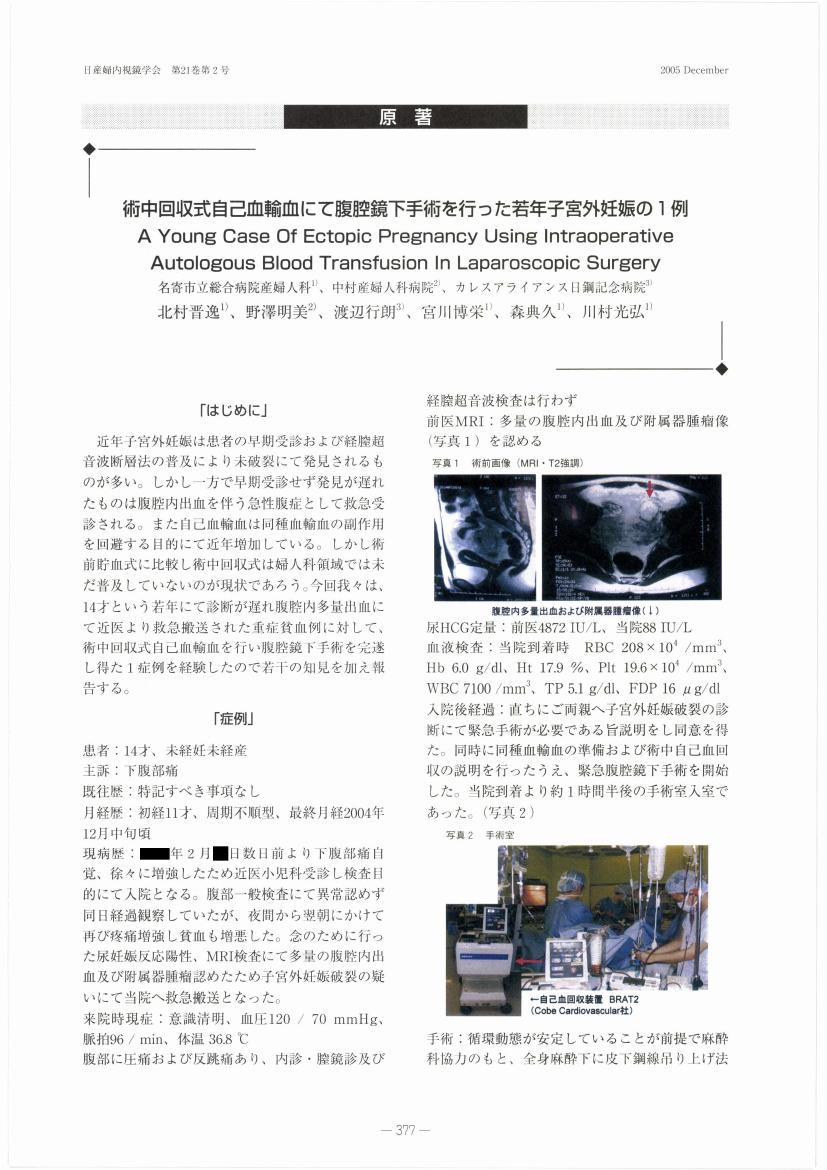
1 0 0 0 OA 術中回収式自己血輸血にて腹腔鏡下手術を行った若年子宮外妊娠の1例
- 著者
- 北村 晋逸 野澤 明美 渡辺 行朗 宮川 博栄 森 典久 川村 光弘
- 出版者
- JAPAN SOCIETY OF GYNECOLOGIC AND OBSTETRIC ENDOSCOPY AND MINIMALLY INVASIVE THERAPY
- 雑誌
- 日本産科婦人科内視鏡学会雑誌 (ISSN:18845746)
- 巻号頁・発行日
- vol.21, no.2, pp.377-379, 2005 (Released:2010-09-09)
- 参考文献数
- 7
1 0 0 0 OA 子宮内膜症開腹手術後不妊150名の腹腔鏡所見と予後
- 著者
- 小林 善宗 井上 正人 本田 育子 野見山 真理 鈴木 隆弘 淡路 英雄 藤井 明和
- 出版者
- 日本産科婦人科内視鏡学会
- 雑誌
- 日本産科婦人科内視鏡学会雑誌 (ISSN:18845746)
- 巻号頁・発行日
- vol.8, no.1, pp.15-18, 1992 (Released:2010-09-09)
- 参考文献数
- 7
1 0 0 0 OA 子宮内膜ポリープ摘出法に関する検討 (子宮内膜掻爬術と子宮鏡下手術の比較)
- 著者
- 谷村 悟 小林 寛人 吉本 英生 中川 俊信 川原 領一
- 出版者
- JAPAN SOCIETY OF GYNECOLOGIC AND OBSTETRIC ENDOSCOPY AND MINIMALLY INVASIVE THERAPY
- 雑誌
- 日本産科婦人科内視鏡学会雑誌 (ISSN:18845746)
- 巻号頁・発行日
- vol.17, no.2, pp.25-27, 2001 (Released:2010-09-09)
- 参考文献数
- 7
1 0 0 0 22.子宮内腔拡張術後妊娠に至ったアッシャーマン症候群の1例
- 著者
- 塩津 英美 大須賀 穰 梁 善光 三橋 直樹 武谷 雄二
- 出版者
- 日本産科婦人科内視鏡学会
- 雑誌
- 日本産科婦人科内視鏡学会雑誌 (ISSN:18849938)
- 巻号頁・発行日
- vol.8, no.1, pp.118, 1992
1 0 0 0 OA 稀な子宮頸部嚢胞性腺筋症に対してTLHを施行した1例―2つの尿路損傷を避ける工夫―
- 著者
- 今井 宗 舟本 寛 山口 彩華 吉越 信一 南 里恵 飴谷 由佳 谷村 悟
- 出版者
- 日本産科婦人科内視鏡学会
- 雑誌
- 日本産科婦人科内視鏡学会雑誌 (ISSN:18849938)
- 巻号頁・発行日
- vol.35, no.1, pp.238-242, 2019 (Released:2019-06-08)
- 参考文献数
- 11
Introduction: Uterine cystic adenomyosis is a rare proliferative disease in which the endometrial tissue focally repeats hemorrhage in the myometrium and forms cystic lesions. We report a case of uterine cervical cystic adenomyosis for which we performed total laparoscopic hysterectomy (TLH) with two techniques to avoid urinary tract injury.Case: The patient was a 45-year-old woman with G0 who had two times of surgery for endometriosis. A local doctor diagnosed uterine cervical cystic adenomyosis about 30 mm in diameter and followed her up. Due to the worsening dysmenorrhea and the enlarging cystic lesion, she was referred to our hospital for treatment. Pelvic MRI showed uterine cervical adenomyosis about 35 mm in diameter and diffuse adenomyosis of the uterine body. TLH was performed because of the worsening dysmenorrhea due to uterine adenomyosis. Anatomical change due to a cervical tumor and severe adhesions because of endometriosis were expected; hence, we carried out two techniques. Firstly, urinary catheters were preoperatively placed, secondary, we injected air into the bladder when the uterus and the bladder were detached, then, TLH was safely completed while monitoring the bladder wall. Histopathology showed endometrial glands in the cervical myometrium, and uterine cervical cystic adenomyosis was diagnosed. Her symptoms have improved, and no recurrence after surgery has been observed. Discussion: Cystic adenomyosis is rarer in the cervix than in the uterine body. There is no report about TLH for uterine cervical cystic adenomyosis. A difficult surgery was expected due to a cervical tumor and endometriosis, but the urinary tract injury was avoided using two techniques, and the surgery was safely completed.
1 0 0 0 OA ダグラス窩閉鎖を伴う症例に対する腹腔鏡下仙骨子宮靱帯切除術~合併症を減らす工夫~
- 著者
- 山中 章義 安藤 正明 小玉 敬亮 白根 晃 柳井 しおり 中島 紗織 福田 美香 黒土 升蔵 海老沢 桂子 羽田 智則 太田 啓明
- 出版者
- 日本産科婦人科内視鏡学会
- 雑誌
- 日本産科婦人科内視鏡学会雑誌 (ISSN:18849938)
- 巻号頁・発行日
- vol.31, no.1, pp.257-263, 2015 (Released:2015-12-23)
- 参考文献数
- 13
- 被引用文献数
- 1
Deeply infiltrating endometriosis (DIE) is defined as subperitoneal invasion by endometriotic lesions. These lesions are considered very active and are strongly associated with pelvic pain. The incidence of DIE is reportedly 20 % in all cases of endometriosis, with uterosacral ligaments representing the most frequent location. Therefore, the resection of uterosacral ligaments is effective in reducing the pelvic pain and dyspareunia that is experienced by patients with endometriosis. However, the operation is associated with a risk of injury to the ureter and rectum; a laparoscopic resection is more useful and safer than open surgery, particularly in patients with adhesion in the pouch of Douglas. Thus, in our study, we initially identified and isolated the ureter and open spaces around the uterosacral ligaments. From June 2012 to December 2013, 262 patients underwent laparoscopic resection of the uterosacral ligaments. Of these, 10 (3.8 %) patients had mild dysuria after the operation, but all cases improved within 2 months. One (0.38 %) patient required clean intermittent catheterization after the operation, which was discontinued 14 months later. Bilateral hydronephrosis occurred in one (0.38 %) patient, which required ureteral dilatation. No ureteral or rectal injury occurred in any patient. Therefore, if the operation is carefully performed, it is possible to safely resect the uterosacral ligaments in patients with endometriosis.
1 0 0 0 OA 腹腔鏡下子宮亜全摘術に対する新しいアプローチ
- 著者
- 西尾 永司 廣田 穰 南 元人 宮田 雅子 山田 英登 宮村 浩徳 西山 幸江 安江 朗 塚田 和彦 宇田川 康博
- 出版者
- JAPAN SOCIETY OF GYNECOLOGIC AND OBSTETRIC ENDOSCOPY AND MINIMALLY INVASIVE THERAPY
- 雑誌
- 日本産科婦人科内視鏡学会雑誌 (ISSN:18845746)
- 巻号頁・発行日
- vol.23, no.1, pp.273-277, 2007 (Released:2010-09-09)
- 参考文献数
- 12
1 0 0 0 腹腔鏡下手術を施行した陳旧性卵管妊娠の2症例
- 著者
- 石山 美由紀 渡辺 正 黒澤 大樹 氷室 裕美 鈴木 久也 宇賀神 智久 中西 透 渡部 洋
- 出版者
- 日本産科婦人科内視鏡学会
- 雑誌
- 日本産科婦人科内視鏡学会雑誌 (ISSN:18849938)
- 巻号頁・発行日
- vol.35, no.2, pp.345-351, 2019
<p><b>Objective:</b> To report our experience with the management of two cases of chronic tubal pregnancy by laparoscopic surgery.</p><p><b>Case 1:</b> A 37-year-old woman presented to our hospital with a small amount of genital bleeding at 10 weeks and 3 days of gestation, calculated from the date of her last menstrual period. Serum human chorionic gonadotropin level was elevated to 108.5 mIU/mL and transvaginal sonography (TVS) revealed a 52-mm diameter of irregularly shaped left periovarian mass. Magnetic resonance imaging (MRI) also showed a periovarian cystic mass with suspicion of an old hemorrhage. We performed laparoscopic left salpingectomy after the diagnosis of chronic left tubal pregnancy.</p><p><b>Case 2:</b> A 31-year-old woman was referred to our hospital with suspected left tubal abortion at 16 weeks and 1 day of gestation. Both TVS and MRI revealed a left periovarian mass with a diameter of 40 mm. After the mass was diagnosed as chronic left tubal pregnancy under laparoscopic vision, left fallopian tube was preserved by salpingotomy. She achieved twin pregnancy by ovulation induction with clomiphene 7 months after laparoscopic surgery.</p><p><b>Conclusion:</b> Although preoperative diagnosis of chronic tubal pregnancy is difficult, laparoscopic approach would be feasible, especially when salpingotomy would be performed for future fertility preservation.</p><p></p>
1 0 0 0 OA 進行卵巣癌に対する審査腹腔鏡の有用性に対する検討
- 著者
- 永井 智之 島田 宗昭 湊 敬道 田中 恵子 土岐 麻実 工藤 敬 橋本 千明 星合 哲郎 徳永 英樹 八重樫 伸生
- 出版者
- 日本産科婦人科内視鏡学会
- 雑誌
- 日本産科婦人科内視鏡学会雑誌 (ISSN:18849938)
- 巻号頁・発行日
- vol.35, no.1, pp.92-97, 2019 (Released:2019-06-08)
- 参考文献数
- 11
Objective: To evaluate the usefulness of diagnostic laparoscopy in patients with advanced ovarian cancer.Methods: We retrospectively analyzed nine patients for whom primary debulking surgery was considered unfeasible. We evaluated whether laparoscopic procedure was adequate in making pathological diagnosis and intraabdominal assessment.Results: Median age was 63 years (range, 47-79 years), and median operation time was 59 minutes (range, 43-103 minutes). All nine patients were pathologically diagnosed with high-grade serous carcinoma and were considered unfit to undergo primary debulking surgery. All patients received chemotherapy. Six patients underwent interval debulking surgery. Only one patient showed mild adhesions between the omentum and the abdominal wall. Conclusion: Diagnostic laparoscopy is safe and feasible in advanced ovarian cancer patients.
1 0 0 0 正常子宮内妊娠と判断されたが卵管間質部妊娠であった一例
- 著者
- 上地 秀昭 野原 理
- 出版者
- 日本産科婦人科内視鏡学会
- 雑誌
- 日本産科婦人科内視鏡学会雑誌 (ISSN:18849938)
- 巻号頁・発行日
- vol.33, no.2, pp.197-201, 2017
<p> Interstitial pregnancy is a rare and life-threatening condition. The most important facet of caring for women with interstitial pregnancy is early diagnosis. We report a case of interstitial pregnancy that was indistinguishable from normal intrauterine pregnancy. A 38-year-old woman, gravida 4 para 3, with a history of laparoscopic salpingectomy for ectopic pregnancy, felt a strong lower abdominal pain and visited our emergency department. The pregnancy test result was positive, and transvaginal ultrasonography revealed intrauterine pregnancy of 11 weeks with intrapelvic hemorrhage but without an adnexal mass. Two hours later, she felt severe upper abdominal pain. Urgent ultrasonography revealed increased intra-abdominal hemorrhage. Emergency laparoscopy was performed. We collected 1400 ml of blood in the abdominopelvic cavity and found that she had a left interstitial pregnancy with bleeding. We removed all gestational tissue and performed a cornuostomy. After the surgery, 4 blood units were transfused. Interstitial pregnancy was difficult to diagnose at 11 weeks of pregnancy. However, ultrasonography revealed intrauterine pregnancy with intrapelvic hemorrhage. Concomitant intrauterine and extrauterine pregnancies or interstitial pregnancy should be considered.</p>
1 0 0 0 OA 抗NMDA受容体脳炎を疑い、緊急腹腔鏡下手術を行った卵巣奇形腫の2例
- 著者
- 長尾 有佳里 鈴木 一弘 新保 暁子 坂堂 美央子 齋藤 愛 廣村 勝彦 安藤 智子
- 出版者
- 日本産科婦人科内視鏡学会
- 雑誌
- 日本産科婦人科内視鏡学会雑誌 (ISSN:18849938)
- 巻号頁・発行日
- vol.31, no.2, pp.399-405, 2016 (Released:2016-05-17)
- 参考文献数
- 10
Anti-N-methyl-D-aspartate (NMDA)-receptor encephalitis is a paraneoplastic encephalitide that causes various symptoms. It occurs especially in young women, with about 60% of cases being associated with ovarian teratoma. We report two cases of emergency laparoscopic surgeries for anti-NMDA-receptor encephalitis associated with ovarian teratoma.Case 1: A 17-year-old woman had headache, fever and vomiting. A week later, she also had abnormal behavior and hallucination and entered hospital. CT scan detected left ovarian teratoma. As anti-NMDA-receptor encephalitis was suspected, she underwent laparoscopic left ovarian cystectomy. She needed post-operative respirator management for 2.5 months. Although discharged after 4.5 months, she was sent to a psychiatrist after 7 months because of domestic violence. The pathological diagnosis was an immature teratoma, but there is no sign of recurrence.Case 2: A 26-year-old woman had fever, headache and fatigue. A few days later, she also had memory disorder and entered hospital. CT scan detected right ovarian teratoma. As anti-NMDA-receptor encephalitis was suspected, she underwent single incision laparoscopic right salpingo-oophorectomy. She needed post-operative respirator management for 9 months and left hospital after 1 year. The pathological diagnosis was a mature teratoma. Antibodies against NMDA-receptor were positive in both cerebrospinal fluids. Early diagnosis and surgery are important for quick recovery of anti-NMDA-receptor encephalitis associated with ovarian teratoma. Even so, patients don't necessarily recover quickly without aftereffects. We should review operative methods, because the patient is young and cannot agree and immature teratoma prevalence is high. Whether a tumor is benign or malignant, it is important to prevent leakage of tumor contents whenever possible.
- 著者
- 奥田 知宏 吉岡 崇 秋山 誠 山下 貞雄
- 出版者
- Japan Society of Gynecologic and Obstetric Endoscopy and Minimally Invasive Therapy
- 雑誌
- 日本産科婦人科内視鏡学会雑誌 (ISSN:18849938)
- 巻号頁・発行日
- vol.26, no.2, pp.429-434, 2010 (Released:2011-06-02)
- 参考文献数
- 17
Laparoscopic surgery is a valuable tool in the definitive diagnosis and treatment of benign uterine tumors. Here we report two cases diagnosed as benign uterine tumors by laparoscopic surgery: the first is an adenomatoid tumor that was suspected preoperatively as a uterine leiomyoma; the second is a uterine leiomyoma that was suspected preoperatively as an adenomatoid tumor.Cases: Case 1: A 63 year-old woman presented to our hospital complaining of lumbago. Uterine myoma was suspected and ultrasound and MRI were performed. A cystic uterine tumor suggesting benign uterine leiomyoma was discovered. However, malignancy could not be ruled out, therefore, the patient consented to LAVH (laparoscopic assisted vaginal hysterectomy). Upon removal of the patient's uterus, macroscopic examination of the tumor was strongly suggestive of uterine leiomyoma. The specimen was sent to pathology; microscopic examination and immunohistological testing provided the definitive diagnosis of benign adenomatoid tumor. Case 2: A 44 year-old woman presented to our hospital for periodic examination of a uterine myoma that she had been diagnosed with several years ago. MRI was performed and myoma nodule was found. To rule out malignancy, a diagnostic and therapeutic laparoscopic assisted myomectomy (LAM) was recommended. LAM was chosen because the tumor surface appeared as a usual myoma nodule. Final pathology findings on immunohistochemical study of the surgical specimen confirmed the diagnosis of uterine leiomyoma.Conclusion: Laparoscopic surgery provides many advantages in clinical gynecological practice. We stress the importance of laparoscopic surgery in preventing misdiagnosis, and in providing definitive diagnosis and treatment in cases of benign gynecologic tumors, including the rare uterine adenomatoid tumor presented herein. We recommend laparoscopic surgical intervention particularly in cases where various imaging studies including MRI, CT, and sonogram, are incompatible with or unable to confirm benign tumor origin.
- 著者
- 亀井 清 玉崗 有吉 吉田 憲一 横倉 恒雄 中村 英世 落合 寛
- 出版者
- 日本産科婦人科内視鏡学会
- 雑誌
- 日本産科婦人科内視鏡学会雑誌 (ISSN:18849938)
- 巻号頁・発行日
- vol.4, no.1, pp.93, 1988
1 0 0 0 OA 腹腔鏡下手術後広範囲な皮下気腫を来たした一例
- 著者
- 関 賢一 高橋 誠治 林 保良 蛯原 照男 福田 俊子 宮本 尚彦 坂倉 啓一 曽山 嘉夫 岩田 嘉行 斉藤 寿一郎 栗林 靖
- 出版者
- 日本産科婦人科内視鏡学会
- 雑誌
- 日本産科婦人科内視鏡学会雑誌 (ISSN:18845746)
- 巻号頁・発行日
- vol.5, no.1, pp.19-22, 1989 (Released:2010-09-09)
- 参考文献数
- 6
1 0 0 0 OA 不正性器出血症例における経腟超音波所見と子宮鏡所見の比較
- 著者
- 大高 究 深谷 暁 三宅 潔 伊藤 元博
- 出版者
- 日本産科婦人科内視鏡学会
- 雑誌
- 日本産科婦人科内視鏡学会雑誌 (ISSN:18845746)
- 巻号頁・発行日
- vol.11, no.1, pp.113-117, 1995 (Released:2010-09-09)
- 参考文献数
- 16
1 0 0 0 OA 9. 当科における原発性無月経症例の検討
- 著者
- 今城 雅彦 松田 博 上田 克憲 藤井 恒夫 藤原 篤 勝部 泰裕
- 出版者
- 日本産科婦人科内視鏡学会
- 雑誌
- 日本産科婦人科内視鏡学会雑誌 (ISSN:18845746)
- 巻号頁・発行日
- vol.5, no.1, pp.62-62, 1989 (Released:2010-09-09)
1 0 0 0 OA 婦人科内視鏡下手術の麻酔で何に留意すべきか
- 著者
- 釘宮 豊城
- 出版者
- 日本産科婦人科内視鏡学会
- 雑誌
- 日本産科婦人科内視鏡学会雑誌 (ISSN:18845746)
- 巻号頁・発行日
- vol.16, no.1, pp.32-32, 2000 (Released:2010-09-09)