- 著者
- Hiroyuki Tsutsui Mitsuaki Isobe Hiroshi Ito Hiroshi Ito Ken Okumura Minoru Ono Masafumi Kitakaze Koichiro Kinugawa Yasuki Kihara Yoichi Goto Issei Komuro Yoshikatsu Saiki Yoshihiko Saito Yasushi Sakata Naoki Sato Yoshiki Sawa Akira Shiose Wataru Shimizu Hiroaki Shimokawa Yoshihiko Seino Koichi Node Taiki Higo Atsushi Hirayama Miyuki Makaya Tohru Masuyama Toyoaki Murohara Shin-ichi Momomura Masafumi Yano Kenji Yamazaki Kazuhiro Yamamoto Tsutomu Yoshikawa Michihiro Yoshimura Masatoshi Akiyama Toshihisa Anzai Shiro Ishihara Takayuki Inomata Teruhiko Imamura Yu-ki Iwasaki Tomohito Ohtani Katsuya Onishi Takatoshi Kasai Mahoto Kato Makoto Kawai Yoshiharu Kinugasa Shintaro Kinugawa Toru Kuratani Shigeki Kobayashi Yasuhiko Sakata Atsushi Tanaka Koichi Toda Takashi Noda Kotaro Nochioka Masaru Hatano Takayuki Hidaka Takeo Fujino Shigeru Makita Osamu Yamaguchi Uichi Ikeda Takeshi Kimura Shun Kohsaka Masami Kosuge Masakazu Yamagishi Akira Yamashina on behalf of the Japanese Circulation Society and the Japanese Heart Failure Society Joint Working Group
- 出版者
- The Japanese Circulation Society
- 雑誌
- Circulation Journal (ISSN:13469843)
- 巻号頁・発行日
- vol.83, no.10, pp.2084-2184, 2019-09-25 (Released:2019-09-25)
- 参考文献数
- 608
- 被引用文献数
- 435
- 著者
- Hayato Tada Hirofumi Okada Atsushi Nohara Masakazu Yamagishi Masayuki Takamura Masa-aki Kawashiri
- 出版者
- The Japanese Circulation Society
- 雑誌
- Circulation Journal (ISSN:13469843)
- 巻号頁・発行日
- vol.85, no.11, pp.2073-2078, 2021-10-25 (Released:2021-10-25)
- 参考文献数
- 23
- 被引用文献数
- 1 24
Background:Recent studies suggest that cumulative exposure to low-density lipoprotein-cholesterol (LDL-C) leads to the development of atherosclerotic cardiovascular disease (ASCVD). However, few studies have investigated whether this link extends to individuals with familial hypercholesterolemia (FH), a relevant patient population.Methods and Results:We retrospectively investigated the health records of 1,050 patients with clinical FH diagnosis between April 1990 and March 2019. We used Cox proportional hazards models adjusted for established ASCVD risk factors to assess the association between cholesterol-year-score and major adverse cardiovascular events (MACEs), including death from any cause or hospitalization due to ASCVD events. Cholesterol-year-score was calculated as LDL-C max × [age at diagnosis/statin initiation] + LDL-C at inclusion × [age at inclusion − age at diagnosis/statin initiation]. The median follow-up period for MACE evaluation was 12.3 (interquartile range, 9.1–17.5) years, and 177 patients experienced MACEs during the observation period. Cholesterol-year-score was significantly associated with MACEs (hazard ratio, 1.35; 95% confidence interval, 1.07–1.53; P=0.0034, per 1,000 mg-year/dL), independent of other traditional risk factors including age and LDL-C, based on cross-sectional assessment. Cholesterol-year-score improved the discrimination ability of other traditional risk factors for ASCVD events (C-index, 0.901 vs. 0.889; P=0.00473).Conclusions:Cumulative LDL-C exposure was strongly associated with MACEs in Japanese patients with FH, warranting early diagnosis and treatment initiation in these patients.
- 著者
- Masakazu Yamagishi Nagara Tamaki Takashi Akasaka Takanori Ikeda Kenji Ueshima Shiro Uemura Yutaka Otsuji Yasuki Kihara Kazuo Kimura Takeshi Kimura Yoshiki Kusama Shinichiro Kumita Hajime Sakuma Masahiro Jinzaki Hiroyuki Daida Yasuchika Takeishi Hiroshi Tada Taishiro Chikamori Kenichi Tsujita Kunihiko Teraoka Kenichi Nakajima Tomoaki Nakata Satoshi Nakatani Akihiko Nogami Koichi Node Atsushi Nohara Atsushi Hirayama Nobusada Funabashi Masaru Miura Teruhito Mochizuki Hiroyoshi Yokoi Kunihiro Yoshioka Masafumi Watanabe Toshihiko Asanuma Yuichi Ishikawa Takahiro Ohara Koichi Kaikita Tokuo Kasai Eri Kato Hiroshi Kamiyama Masaaki Kawashiri Keisuke Kiso Kakuya Kitagawa Teruhito Kido Toshio Kinoshita Tomonari Kiriyama Teruyoshi Kume Akira Kurata Satoshi Kurisu Masami Kosuge Eitaro Kodani Akira Sato Yasutsugu Shiono Hiroki Shiomi Junichi Taki Masaaki Takeuchi Atsushi Tanaka Nobuhiro Tanaka Ryoichi Tanaka Takuya Nakahashi Takehiro Nakahara Akihiro Nomura Akiyoshi Hashimoto Kenshi Hayashi Masahiro Higashi Takafumi Hiro Daisuke Fukamachi Hitoshi Matsuo Naoya Matsumoto Katsumi Miyauchi Masao Miyagawa Yoshitake Yamada Keiichiro Yoshinaga Hideki Wada Tetsu Watanabe Yukio Ozaki Shun Kohsaka Wataru Shimizu Satoshi Yasuda Hideaki Yoshino on behalf of the Japanese Circulation Society Working Group
- 出版者
- The Japanese Circulation Society
- 雑誌
- Circulation Journal (ISSN:13469843)
- 巻号頁・発行日
- pp.CJ-19-1131, (Released:2021-02-16)
- 参考文献数
- 1401
- 被引用文献数
- 50
- 著者
- Hayato Tada Masa-aki Kawashiri Masakazu Yamagishi
- 出版者
- 日本循環器学会
- 雑誌
- Circulation Journal (ISSN:13469843)
- 巻号頁・発行日
- pp.CJ-17-0586, (Released:2017-07-01)
- 参考文献数
- 11
- 被引用文献数
- 1
- 著者
- Koji Hara Yukihiro Tominari Masakazu Yamagishi Jun Takeya
- 出版者
- The Surface Science Society of Japan
- 雑誌
- e-Journal of Surface Science and Nanotechnology (ISSN:13480391)
- 巻号頁・発行日
- vol.13, pp.426-426, 2015-09-19 (Released:2015-09-19)
- 参考文献数
- 2
On July 30th 2015, the Editor-in-Chief sent a letter to the corresponding author of the above-mentioned manuscript [1] about the result of survey by the Editorial Committee of e-J. Surf. Sci. Nanotech. According to the letter, the Committee concluded that the above-mentioned manuscript resembles the paper published in another journal [2] too much. As a result of this report, all of the authors of the above-mentioned manuscript have agreed to a complete retraction of the paper.
- 著者
- Kenshi Hayashi Toyonobu Tsuda Akihiro Nomura Noboru Fujino Atsushi Nohara Kenji Sakata Tetsuo Konno Chiaki Nakanishi Hayato Tada Yoji Nagata Ryota Teramoto Yoshihiro Tanaka Masa-aki Kawashiri Masakazu Yamagishi on behalf of the Hokuriku-Plus AF Registry Investigators
- 出版者
- The Japanese Circulation Society
- 雑誌
- Circulation Journal (ISSN:13469843)
- 巻号頁・発行日
- pp.CJ-17-1085, (Released:2018-03-01)
- 参考文献数
- 22
- 被引用文献数
- 30
Background:B-type natriuretic peptide (BNP) may be a predictor of stroke risk in patients with nonvalvular atrial fibrillation (NVAF); because heart failure is associated with the incidence of stroke in AF patients. However, limited data exist regarding the association between BNP at baseline and risks of thromboembolic events (TE) and death in NVAF patients.Methods and Results:We prospectively studied 1,013 NVAF patients (725 men, 72.8±9.7 years old) from the Hokuriku-plus AF Registry to determine the relationship between BNP at baseline and prognosis among Japanese NVAF patients. During the follow-up period (median, 751 days); 31 patients experienced TE and there were 81 cases of TE/all-cause death. For each endpoint we constructed receiver-operating characteristic curves that gave cutoff points of BNP for TE (170 pg/mL) and TE/all-cause death (147 pg/mL). Multivariate analysis with the Cox-proportional hazards model indicated that high BNP was significantly associated with risks of TE (hazard ratio [HR] 3.86; 95% confidence interval [CI] 1.83–8.67; P=0.0003) and TE/all-cause death (HR 2.27; 95% CI 1.45–3.56; P=0.0003). Based on the C-index and net reclassification improvement, the addition of BNP to CHA2DS2-VASc statistically improved the prediction of TE.Conclusions:In a real-world cohort of Japanese NVAF patients, high BNP was significantly associated with TE and death. Plasma BNP might be a useful biomarker for these adverse clinical events.
- 著者
- Hayato Tada Masa-aki Kawashiri Taiji Yoshida Ryota Teramoto Atsushi Nohara Tetsuo Konno Akihiro Inazu Hiroshi Mabuchi Masakazu Yamagishi Kenshi Hayashi
- 出版者
- 日本循環器学会
- 雑誌
- Circulation Journal (ISSN:13469843)
- 巻号頁・発行日
- pp.CJ-15-0999, (Released:2015-12-02)
- 参考文献数
- 39
- 被引用文献数
- 7 62
Background:It has been shown that serum lipoprotein(a) [Lp(a)] is elevated in familial hypercholesterolemia (FH) with mutation(s) of the LDL receptor (LDLR) gene. However, few data exist regarding Lp(a) levels in FH with gain-of-function mutations of the PCSK9 gene.Methods and Results:We evaluated 42 mutation-determined heterozygous FH patients with aPCSK9gain-of-function mutation (FH-PCSK9, mean age 52, mean LDL-C 235 mg/dl), 198 mutation-determined heterozygous FH patients with aLDLRmutation (FH-LDLR, mean age 44, mean LDL-C 217 mg/dl), and 4,015 controls (CONTROL, mean age 56, mean LDL-C 109 mg/dl). We assessed their Lp(a), total cholesterol, triglycerides, HDL-C, LDL-C, use of statins, presence of hypertension, diabetes, chronic kidney disease, smoking, body mass index (BMI) and coronary artery disease (CAD). Multiple regression analysis showed that HDL-C, use of statins, presence of hypertension, smoking, BMI, and Lp(a) were independently associated with the presence of CAD. Under these conditions, the serum levels of Lp(a) in patients with FH were significantly higher than those of the CONTROL group regardless of their causative genes, among the groups propensity score-matched (median Lp(a) 12.6 mg/dl [IQR:9.4–33.9], 21.1 mg/dl [IQR:11.7–34.9], and 5.0 mg/dl [IQR:2.7–8.1] in the FH-LDLR, FH-PCSK9, and CONTROL groups, respectively, P=0.002 for FH-LDLR vs. CONTROL, P=0.002 for FH-PCSK9 vs. CONTROL).Conclusions:These data demonstrate that serum Lp(a) is elevated in patients with FH caused by PCSK9 gain-of-function mutations to the same level as that in FH caused by LDLR mutations.
- 著者
- Toyonobu Tsuda Kenshi Hayashi Takeshi Kato Takashi Kusayama Yoichiro Nakagawa Akihiro Nomura Hayato Tada Soichiro Usui Kenji Sakata Masa-aki Kawashiri Noboru Fujino Masakazu Yamagishi Masayuki Takamura on behalf of the Hokuriku-Plus AF Registry Investigators
- 出版者
- The Japanese Circulation Society
- 雑誌
- Circulation Journal (ISSN:13469843)
- 巻号頁・発行日
- pp.CJ-23-0418, (Released:2023-10-20)
- 参考文献数
- 37
- 被引用文献数
- 1
Background: The prognostic effect of concomitant hypertrophic cardiomyopathy (HCM) on adverse events in patients with atrial fibrillation (AF) has not been evaluated in a multicenter prospective cohort study in Japan.Methods and Results: Using the Hokuriku-Plus AF Registry, 1,396 patients with nonvalvular AF (1,018 men, 72.3±9.7 years old) were assessed prospectively; 72 (5.2%) had concomitant HCM. During a median follow-up of 5.0 years (interquartile range 3.5–5.3 years), 79 cases of thromboembolism (1.3 per 100 person-years) and 192 of heart failure (HF) (3.2 per 100 person-years) occurred. Kaplan-Meier analysis revealed that the HCM group had a significantly greater incidence of thromboembolism (P=0.002 by log-rank test) and HF (P<0.0001 by a log-rank test) than the non-HCM group. The Cox proportional hazards model demonstrated that persistent AF (adjusted hazard ratio 2.98, 95% confidence interval 1.56–6.21), the CHA2DS2-VASc score (1.35, 1.18–1.54), and concomitant HCM (2.48, 1.16–4.79) were significantly associated with thromboembolism. Conversely, concomitant HCM (2.81, 1.72–4.43), older age (1.07, 1.05–1.10), lower body mass index (0.95, 0.91–0.99), a history of HF (2.49, 1.77–3.52), and lower left ventricular ejection fraction (0.98, 0.97–0.99) were significantly associated with the development of HF.Conclusions: Concomitant HCM predicts the incidence of thromboembolism and HF in AF patients.
- 著者
- Toyonobu Tsuda Takeshi Kato Keisuke Usuda Takashi Kusayama Soichiro Usui Kenji Sakata Kenshi Hayashi Masa-aki Kawashiri Masakazu Yamagishi Masayuki Takamura Takayuki Otsuka Shinya Suzuki Akio Hirata Masato Murakami Mitsuru Takami Masaomi Kimura Hidehira Fukaya Shiro Nakahara Wataru Shimizu Yu-ki Iwasaki Hiroshi Hayashi Tomoo Harada Ikutaro Nakajima Ken Okumura Junjiroh Koyama Michifumi Tokuda Teiichi Yamane Yukihiko Momiyama Kojiro Tanimoto Kyoko Soejima Noriko Nonoguchi Koichiro Ejima Nobuhisa Hagiwara Masahide Harada Kazumasa Sonoda Masaru Inoue Koji Kumagai Hidemori Hayashi Kazuhiro Satomi Yoshinao Yazaki Yuji Watari Masaru Arai Ryuta Watanabe Katsuaki Yokoyama Naoya Matsumoto Koichi Nagashima Yasuo Okumura on behalf of the AF Ablation Frontier Registry and the Hokuriku-Plus AF Registry Investigators
- 出版者
- The Japanese Circulation Society
- 雑誌
- Circulation Journal (ISSN:13469843)
- 巻号頁・発行日
- vol.87, no.7, pp.939-946, 2023-06-23 (Released:2023-06-23)
- 参考文献数
- 36
- 被引用文献数
- 5
Background: A recent randomized trial demonstrated that catheter ablation for atrial fibrillation (AF) in patients with heart failure with reduced ejection fraction (EF) is associated with a reduction in death or heart failure. However, the effect of catheter ablation for AF in patients with heart failure with mid-range or preserved EF is unclear.Methods and Results: We screened 899 AF patients (72.4% male, mean age 68.4 years) with heart failure and left ventricular EF ≥40% from 2 Japanese multicenter AF registries: the Atrial Fibrillation registry to Follow the long-teRm Outcomes and use of aNTIcoagulants aftER Ablation (AF Frontier Ablation Registry) as the ablation group (525 patients who underwent ablation) and the Hokuriku-Plus AF Registry as the medical therapy group (374 patients who did not undergo ablation). Propensity score matching was performed in these 2 registries to yield 106 matched patient pairs. The primary endpoint was a composite of cardiovascular death and hospitalization for heart failure. At 24.6 months, the ablation group had a significantly lower incidence of the primary endpoint (hazard ratio 0.32; 95% confidence interval 0.13–0.70; P=0.004) than the medical therapy group.Conclusions: Compared with medical therapy, catheter ablation for AF in patients with heart failure and mid-range or preserved EF was associated with a significantly lower incidence of cardiovascular death or hospitalization for heart failure.
- 著者
- Toyonobu Tsuda Takeshi Kato Keisuke Usuda Takashi Kusayama Soichiro Usui Kenji Sakata Kenshi Hayashi Masa-aki Kawashiri Masakazu Yamagishi Masayuki Takamura Takayuki Otsuka Shinya Suzuki Akio Hirata Masato Murakami Mitsuru Takami Masaomi Kimura Hidehira Fukaya Shiro Nakahara Wataru Shimizu Yu-ki Iwasaki Hiroshi Hayashi Tomoo Harada Ikutaro Nakajima Ken Okumura Junjiroh Koyama Michifumi Tokuda Teiichi Yamane Yukihiko Momiyama Kojiro Tanimoto Kyoko Soejima Noriko Nonoguchi Koichiro Ejima Nobuhisa Hagiwara Masahide Harada Kazumasa Sonoda Masaru Inoue Koji Kumagai Hidemori Hayashi Kazuhiro Satomi Yoshinao Yazaki Yuji Watari Masaru Arai Ryuta Watanabe Katsuaki Yokoyama Naoya Matsumoto Koichi Nagashima Yasuo Okumura on behalf of the AF Ablation Frontier Registry and the Hokuriku-Plus AF Registry Investigators
- 出版者
- The Japanese Circulation Society
- 雑誌
- Circulation Journal (ISSN:13469843)
- 巻号頁・発行日
- pp.CJ-22-0461, (Released:2022-12-02)
- 参考文献数
- 36
- 被引用文献数
- 5
Background: A recent randomized trial demonstrated that catheter ablation for atrial fibrillation (AF) in patients with heart failure with reduced ejection fraction (EF) is associated with a reduction in death or heart failure. However, the effect of catheter ablation for AF in patients with heart failure with mid-range or preserved EF is unclear.Methods and Results: We screened 899 AF patients (72.4% male, mean age 68.4 years) with heart failure and left ventricular EF ≥40% from 2 Japanese multicenter AF registries: the Atrial Fibrillation registry to Follow the long-teRm Outcomes and use of aNTIcoagulants aftER Ablation (AF Frontier Ablation Registry) as the ablation group (525 patients who underwent ablation) and the Hokuriku-Plus AF Registry as the medical therapy group (374 patients who did not undergo ablation). Propensity score matching was performed in these 2 registries to yield 106 matched patient pairs. The primary endpoint was a composite of cardiovascular death and hospitalization for heart failure. At 24.6 months, the ablation group had a significantly lower incidence of the primary endpoint (hazard ratio 0.32; 95% confidence interval 0.13–0.70; P=0.004) than the medical therapy group.Conclusions: Compared with medical therapy, catheter ablation for AF in patients with heart failure and mid-range or preserved EF was associated with a significantly lower incidence of cardiovascular death or hospitalization for heart failure.
2 0 0 0 OA Retraction: Organic Single-Crystal Transistors with Secondary Gates on Source and Drain Electrodes
- 著者
- Koji Hara Yukihiro Tominari Masakazu Yamagishi Jun Takeya
- 出版者
- The Japan Society of Vacuum and Surface Science
- 雑誌
- e-Journal of Surface Science and Nanotechnology (ISSN:13480391)
- 巻号頁・発行日
- vol.6, pp.138-141, 2008-05-29 (Released:2008-05-29)
- 参考文献数
- 10
This article was retracted.
- 著者
- Kiyoo Mori Kazunori Yamada Tetsuo Konno Dai Inoue Yoshihide Uno Michio Watanabe Miho Okuda Kotaro Oe Mitsuhiro Kawano Masakazu Yamagishi
- 出版者
- 一般社団法人 日本内科学会
- 雑誌
- Internal Medicine (ISSN:09182918)
- 巻号頁・発行日
- vol.54, no.10, pp.1231-1235, 2015 (Released:2015-05-15)
- 参考文献数
- 17
- 被引用文献数
- 4 24
We herein report the case of a 65-year-old man with pericardial involvement associated with autoimmune pancreatitis. Chest CT imaging showed pericardial thickening. The patient responded to corticosteroid therapy, and the pericardial thickening resolved. Multiple organs are involved in immunoglobulin G4 (IgG4)-related disease (IgG4-RD); however, only a few cases of IgG4-related chronic constrictive pericarditis have been reported. To our knowledge, this is the first reported case of IgG4-RD with pericardial involvement at an early stage. This case indicates that recognizing pericardial complications in autoimmune pancreatitis is important and that CT imaging may be useful for obtaining the diagnosis and providing follow-up of pericardial lesions in cases of IgG4-RD.
- 著者
- Shigetsugu Tsuji Atsushi Nohara Yoshiaki Hayashi Isao Yoshida Rie Oka Tadashi Moriuchi Tomomi Hagishita Susumu Miyamoto Ayako Suzuki Toshihide Okada Masakazu Yamagishi
- 出版者
- 一般社団法人 日本動脈硬化学会
- 雑誌
- Journal of Atherosclerosis and Thrombosis (ISSN:13403478)
- 巻号頁・発行日
- pp.25825, (Released:2014-10-23)
- 参考文献数
- 42
Aim: The role of gastrectomy in glycemic control has been established in the current era of bariatric surgery for obesity. Gastrectomy in obese patients is associated with increased levels of high-density lipoprotein cholesterol (HDL-C). However, limited data on the effects of gastrectomy in nonobese patients are available. We herein investigated the long-term plasma lipid changes in nonobese patients who had undergone gastrectomy. Methods: Patients were enrolled as part of routine healthcare examinations from 1984 to 2003. Preoperative and postoperative data from patients who had undergone curative gastrectomy were analyzed for up to 10 years postoperatively. Three age- and sex-matched controls were assigned to each case. Results: Sixty-four nonobese patients without diabetes mellitus or a history of having taken lipidlowering drugs who underwent curative gastrectomy during the study period were enrolled (60 subtotal gastrectomies, four total gastrectomies). The median follow-up period was 7.6 years. The mean body mass index was 9.6% lower one year after gastrectomy (p<0.01), then plateaued with a slight recovery. Intriguingly, the preoperative HDL-C level was 21% higher one year after gastrectomy (p<0.01), increased by another 30% six years after gastrectomy and remained at this level for the rest of the follow-up period. No significant changes in the HDL-C level were observed in the controls. The degree of HDL-C elevation was consistently significant, irrespective of the baseline triglyceride level, HDL-C level or body weight. Conclusions: Gastrectomy in nonobese patients was associated with consistent and distinct long-term HDL-C elevations and body mass index reductions.
- 著者
- Miwa Ono Satoshi Nakatani Keiji Hirooka Masakazu Yamagishi Kunio Miyatake
- 出版者
- Japanese Society of Echocardiography
- 雑誌
- Journal of Echocardiography (ISSN:13490222)
- 巻号頁・発行日
- vol.1, no.1, pp.8-14, 2003 (Released:2005-07-08)
- 参考文献数
- 25
- 被引用文献数
- 2 2
OBJECTIVES: Mitral valve closure produces a flow which propagates through the left atrium (LA) to the pulmonary vein (PV) and forms a small flow reversal (C wave) on the PV flow pattern. We examined whether propagation of mitral closure flow into LA might reflect LA compliance in patients with atrial fibrillation (AF).METHODS: We recorded PV flow velocity pattern using transesophageal echocardiography in 73 patients with AF. They were divided into 3 groups according to the estimated severity of LA damage; almost normal (Group I, 16 patients with lone AF), mildly damaged (Group II, 23 patients), and severely damaged LA function (Group III, 34 patients). C wave peak velocity (CV), the time from Q wave on ECG to the C wave peak (QC) and QC divided by LA long-axis diameter (QC/LAD) were obtained. Of the study population, in 18 patients with mitral stenosis who underwent percutaneous mitral valvotomy, mean LA compliance was calculated by dividing cardiac stroke volume by systolic rise in LA pressure.RESULTS: QC and QC/LAD proportionally prolonged as the disease severity increased (QC; 84±23 vs. 93±21 vs. 107±27 ms, p<0.01, QC/LAD; 1.44±0.32 vs. 1.47±0.32 vs. 1.79±0.55ms/mm, p<0.05 for Group I, II and III, respectively). QC and QC/LAD showed significant negative correlations with mean LA compliance (p<0.05).CONCLUSION: Propagation of a flow into LA produced by mitral closure may provide new noninvasive indexes to assess LA compliance in patients with AF.
- 著者
- Hayato Tada Hirofumi Okada Akihiro Nomura Soichiro Usui Kenji Sakata Atsushi Nohara Masakazu Yamagishi Masayuki Takamura Masa-aki Kawashiri
- 出版者
- The Japanese Circulation Society
- 雑誌
- Circulation Journal (ISSN:13469843)
- 巻号頁・発行日
- pp.CJ-20-0901, (Released:2020-12-03)
- 参考文献数
- 21
- 被引用文献数
- 11
Background:This study is aimed to compare the efficacy of the 2017 Japan Atherosclerosis Society (JAS) familial hypercholesterolemia (FH) criteria, which focuses on only 3 essential clinical manifestations, with that of Dutch Lipid Clinic Network (DLCN) FH criteria, which adopts a scoring system of multiple elements.Methods and Results:A total of 680 Japanese dyslipidemic participants (51% men) were enrolled between 2006 and 2018, all of whom had full evaluations of low-density lipoprotein (LDL) cholesterol, Achilles tendon X-rays, family history records, and genetic analysis of FH-associated genes (LDLR,APOB, andPCSK9). Predictive values for the existence of FH mutations by both clinical criteria were evaluated. Overall, 173 FH patients were clinically diagnosed by using the 2017 JAS criteria and 100, 57, 156, and 367 subjects were also diagnosed as having definite, probable, possible, and unlikely FH by the DLCN FH criteria, respectively. The positive and negative likelihood ratio predicting the presence of FH mutations by using the 2017 JAS FH criteria were 19.8 and 0.143, respectively; whereas, using the DLCN criteria of definite, probable, and possible FH, the ratios were 29.2 and 0.489, 9.70 and 0.332, and 3.43 and 0.040, respectively.Conclusions:Among Japanese patients, the JAS 2017 FH criteria is considered superior to diagnose FH mutation-positive patients and simultaneously rule out FH mutation-negative patients compared with the DLCN FH criteria.
- 著者
- Akira Funada Yoshikazu Goto Hayato Tada Ryota Teramoto Masaya Shimojima Kenshi Hayashi Masakazu Yamagishi
- 出版者
- The Japanese Circulation Society
- 雑誌
- Circulation Journal (ISSN:13469843)
- 巻号頁・発行日
- pp.CJ-16-1251, (Released:2017-02-11)
- 参考文献数
- 28
- 被引用文献数
- 5 7
Background:The appropriate duration of prehospital cardiopulmonary resuscitation (CPR)administered by emergency medical service (EMS) providers for patients with out-of-hospital cardiac arrest (OHCA) necessary to achieve 1-month survival with favorable neurological outcome (Cerebral Performance Category 1 or 2, CPC 1–2) is unclear and could differ by age.Methods and Results:We analyzed the records of 35,709 adult OHCA patients with return of spontaneous circulation (ROSC) before hospital arrival in a prospectively recorded Japanese registry between 2011 and 2014. The CPR duration was defined as the time from CPR initiation by EMS providers to prehospital ROSC. The rate of 1-month CPC 1–2 was 21.4% (7,650/35,709). The CPR duration was independently and inversely associated with 1-month CPC 1–2 (adjusted odds ratio, 0.93 per 1-min increment; 95% confidence interval, 0.93–0.94). The CPR duration increased with age (P<0.001). However, the CPR duration beyond which the proportion of OHCA patients with 1-month CPC 1–2 decreased to <1% declined with age: 28 min for patients aged 18–64 years, 25 min for 65–74 years, 23 min for 75–84 years, 20 min for 85–94 years, and 18 min for ≥95 years.Conclusions:In patients who achieved prehospital ROSC after OHCA, the duration of CPR administered by EMS providers necessary to achieve 1-month CPC 1–2 varied by age.
- 著者
- Kenji Sakata Tadatsugu Gamou Hayato Tada Kenshi Hayashi Hidekazu Ino Masakazu Yamagishi Masa-aki Kawashiri behalf of the MILLION Study Group
- 出版者
- Japan Atherosclerosis Society
- 雑誌
- Journal of Atherosclerosis and Thrombosis (ISSN:13403478)
- 巻号頁・発行日
- pp.44255, (Released:2018-09-21)
- 参考文献数
- 25
- 被引用文献数
- 3
Aim: The prospective, randomized, multicenter Myocardial Ischemia Treated with Percutaneous Coronary Intervention and Plaque Regression by Lipid Lowering & Blood Pressure Controlling assessed by Intravascular Ultrasonography (MILLION) study demonstrated that combined treatment with atorvastatin and amlodipine enhanced coronary artery plaque regression. Although the baseline high-sensitive C-reactive protein (hs-CRP) reportedly plays an important role in atherogenesis, few data exist regarding the relationship between hs-CRP and plaque regression in patients receiving a combined atorvastatin and amlodipine therapy.Methods: A total of 68 patients (male, 55; mean age, 64.2 years) with baseline and follow-up 3-dimensional intravascular ultrasound examinations in the MILLION study were stratified by baseline hs-CRP level quartiles. The serial measurements of lipid, blood pressure, and percentage changes in the plaque volume were compared between the groups, and the factors associated with the percentage change in the plaque volume were assessed.Results: There were no significant between-group differences in the extent of change in low-density lipoprotein cholesterol (LDL-C) or systolic and diastolic blood pressure after 18–24 months of treatment. The percentage change in the plaque volume showed a linear association with the baseline hs-CRP (p for trend <0.05); however, there was no correlation with changes in LDL-C or systolic and diastolic blood pressure. In the multiple regression analysis, the baseline hs-CRP level was independently associated with the percentage change in the plaque volume (β=0.29, p=0.022).Conclusions: Coronary plaque regression was associated with the baseline hs-CRP level in patients treated with a combined lipid- and blood pressure-lowering therapy.
1 0 0 0 OA Oral Fat Tolerance Test for Sitosterolemia and Familial Hypercholesterolemia: A Study Protocol
- 著者
- Akihiro Nomura Hayato Tada Atsushi Nohara Masa-aki Kawashiri Masakazu Yamagishi
- 出版者
- Japan Atherosclerosis Society
- 雑誌
- Journal of Atherosclerosis and Thrombosis (ISSN:13403478)
- 巻号頁・発行日
- pp.42960, (Released:2018-01-20)
- 参考文献数
- 27
- 被引用文献数
- 7
Aim: Sitosterolemia is an extremely rare, autosomal recessive disease characterized by high plasma cholesterols and plant sterols because of increased absorption of dietary cholesterols and sterols from the intestine, and decreased excretion from biliary tract. Previous study indicated that sitosterolemic patients might be vulnerable to post-prandial hyperlipidemia, including high remnant-like lipoprotein particles (RLP) level. Here we evaluate whether a loading dietary fat increases a post-prandial RLP cholesterol level in sitosterolemic patients compared to heterozygous familial hypercholesterolemic patients (FH).Methods: We recruit total of 20 patients: 5 patients with homozygous sitosterolemia, 5 patients with heterozygous sitosterolemia, and 10 patients with heterozygous FH as controls from May 2015 to March 2018 at Kanazawa University Hospital, Japan. All patients receive Oral Fat Tolerance Test (OFTT) cream (50 g/body surface area square meter, orally only once, and the cream includes 34% of fat, 74 mg of cholesterol, and rich in palmitic and oleic acids. The primary endpoint is the change of a RLP cholesterol level after OFTT cream loading between sitosterolemia and FH. We measure them at baseline, and 2, 4, and 6 hours after the oral fat loading.Results: This is the first study to evaluate whether sitosterolemia patients have a higher post-prandial RLP cholesterol level compared to heterozygous FH patients.Conclusion: The result may become an additional evidence to restrict dietary cholesterols for sitosterolemia. This study is registered at University Hospital Medical Information Network (UMIN) Clinical Trials Registry (UMIN ID: UMIN000020330).
- 著者
- Tadatsugu Gamou Kenji Sakata Hayato Tada Tetsuo Konno Kenshi Hayashi Hidekazu Ino Masakazu Yamagishi Masa-aki Kawashiri on behalf of the MILLION Study Group
- 出版者
- 日本循環器学会
- 雑誌
- Circulation Journal (ISSN:13469843)
- 巻号頁・発行日
- vol.81, no.10, pp.1490-1495, 2017-09-25 (Released:2017-09-25)
- 参考文献数
- 31
- 被引用文献数
- 4
Background:The MILLION study, a prospective randomized multicenter study, revealed that lipid and blood pressure (BP)-lowering therapy resulted in regression of coronary plaque as determined by intravascular ultrasound (IVUS). In the present study we performed additional analysis to investigate the associated factors with regression of coronary plaque.Methods and Results:We investigated serial 3D IVUS images from 68 patients in the MILLION study. Standard IVUS parameters were assessed at both baseline and follow-up (18–24 months). Volumetric data were standardized by length as normalized volume. In patients with plaque regression (n=52), plaque volumenormalizedsignificantly decreased from 64.8 to 55.8 mm3(P<0.0001) and vessel volumenormalizedsignificantly decreased from 135.0 to 127.5 mm3(P=0.0008). There was no difference in lumen volumenormalizedfrom 70.1 to 71.8 mm3(P=0.27). There were no correlations between % changes in vessel volume and cholesterol or BP. On the other hand, negative correlations between % change in vessel volume and vessel volumenormalizedat baseline (r=−0.352, P=0.009) or plaque volumenormalizedat baseline (r=−0.336, P=0.01) were observed.Conclusions:The current data demonstrated that in patients with plaque regression treated by aggressive lipid and BP-lowering therapy, the plaque regression was derived from reverse vessel remodeling determined by vessel volume and plaque burden at baseline irrespective of decreases in lipids and BP.
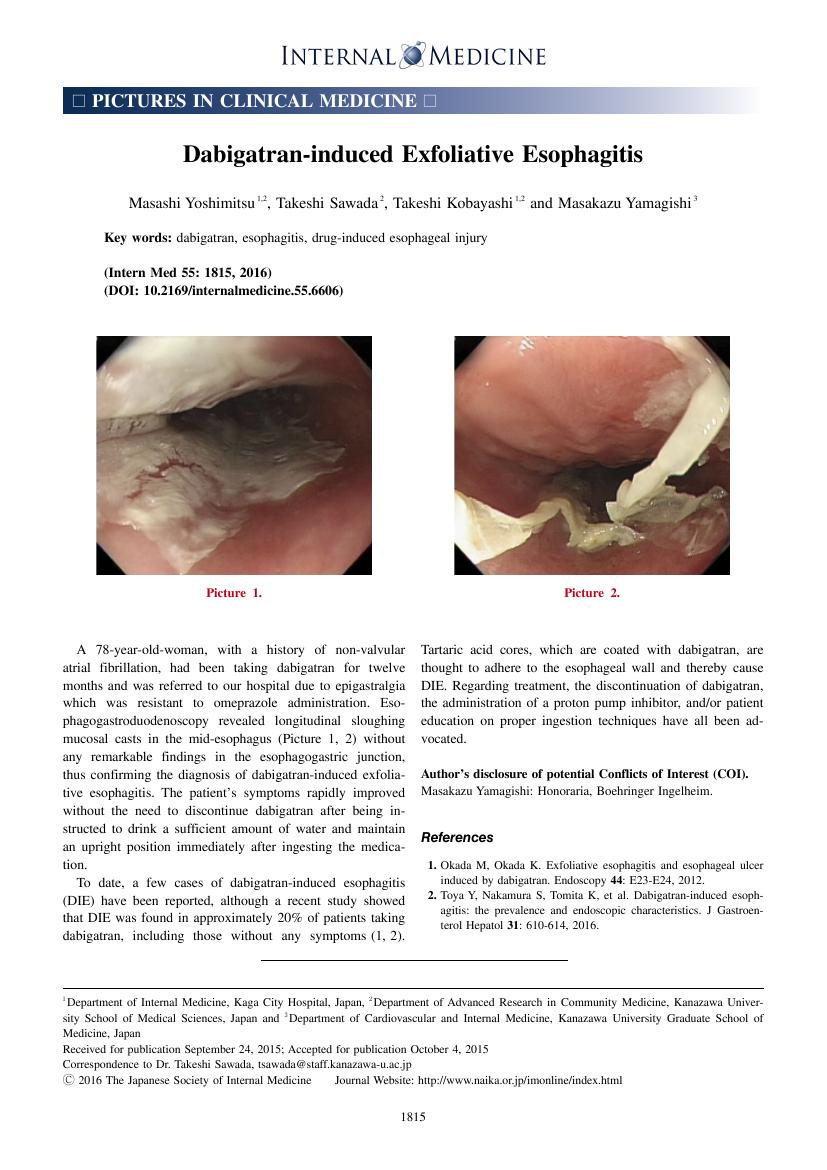
1 0 0 0 OA Dabigatran-induced Exfoliative Esophagitis
- 著者
- Masashi Yoshimitsu Takeshi Sawada Takeshi Kobayashi Masakazu Yamagishi
- 出版者
- 一般社団法人 日本内科学会
- 雑誌
- Internal Medicine (ISSN:09182918)
- 巻号頁・発行日
- vol.55, no.13, pp.1815-1815, 2016-07-01 (Released:2016-07-01)
- 参考文献数
- 2
- 被引用文献数
- 1 4